Translate this page into:
Challenges and opportunities in providing palliative care services to children with a life-limiting illness: A systematic review
Correspondence to RAKESH GARG; drrgarg@hotmail.com
[To cite: Agrawal US, Sarin J, Bakhshi S, Garg R. Challenges and opportunities in providing palliative care services to children with a life-limiting illness: A systematic review. Natl Med J India 2022;35:284–9.]
Abstract
Background
Palliative care for children is an innovative approach that helps improve the quality of life of children suffering from life-limiting illnesses, and their family members. The WHO recognized palliative care as a part of universal health coverage. However, there is inadequate availability and inequitable distribution of palliative care services for children in most parts of the world. We reviewed the existing literature to assess (i) the challenges in providing palliative care services for children suffering from life-limiting illnesses and (ii) the strategies or opportunities to overcome these challenges.
Methods
We conducted systematic searches in the PubMed and Scopus databases to find articles published in the past 10 years (January 2011 to December 2020). The population, concept and context (PCC) framework was used to devise a search strategy in an electronic database.
Results
A total of 1562 articles were found by searching the database and other sources. Title and abstracts of articles were screened, and 206 articles were selected for full-text review. After scrutiny 28 articles met the inclusion criteria. Barriers to and opportunities in the provision of palliative care services for children were identified at policy, organizational, healthcare provider, and patient/family levels.
Conclusion
We found that the majority of barriers to provision of palliative care services for children with life-limiting illnesses can be addressed by adopting research-driven strategies. Adequate and equitable distribution of palliative care services is required for improving children and their family members’ quality of life.
INTRODUCTION
Palliative care is a science that aims to alleviate the symptoms and improve patients’ quality of life. Patients with life-limiting chronic medical illnesses may be offered palliative care services irrespective of whether the patient is receiving the treatment directed at the disease or not. The WHO defines ‘palliative care as the prevention and relief of suffering of adult and paediatric patients and their families facing problems associated with a life-threatening illness. These problems include the physical, psychological, social and spiritual suffering of patients and family members.’1
Palliative care needs to be provided to all, irrespective of age. Palliative care for children is a philosophy and also a systematic way to provide individualized care to children with life-limiting illnesses. The main aims of the provision of palliative care to children include improving the quality of life of the child and family, preventing or reducing suffering, functional optimization, and offering opportunities for growth in the personal and spiritual domain of the suffering child.2 The early integration of palliative care for children at the time of diagnosis of the life-limiting illness leads to a better impact on the overall outcome and should be considered irrespective of whether or not a child receives disease-modification treatment.3 It should be integrated into the holistic care of children suffering along with curative/ disease-modifying treatment/other innovative modalities such as metronomic therapy to improve the quality of life of the child and family.4,5 The provision of palliative care to children requires a multidisciplinary approach. It can be provided by a child’s treating doctor trained in basic or intermediate level palliative care. All children may not always require a palliative care specialist. Some children with refractory or complex symptoms may require intervention by palliative care physicians.6
As per the WHO estimate, globally 1.2 million children require palliative care at the end of life.3 Of these, almost 98% live in low- and middle-income countries with few palliative care provisions.7 Various obstacles have been reported to the optimal provision of palliative care to children such as low assess and inequitable distribution of services, lack of support from policy-makers, limited resources, lack of trained workforce, financial constraints, etc.
We did this systematic review to synthesize the evidence in the published literature with the objectives to assess the (i) challenges in the provision of palliative care services for children suffering from life-limiting illnesses and (ii) strategies and opportunities to overcome these challenges.
METHOD
This systematic review was planned and conducted as per the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (Fig. 1).
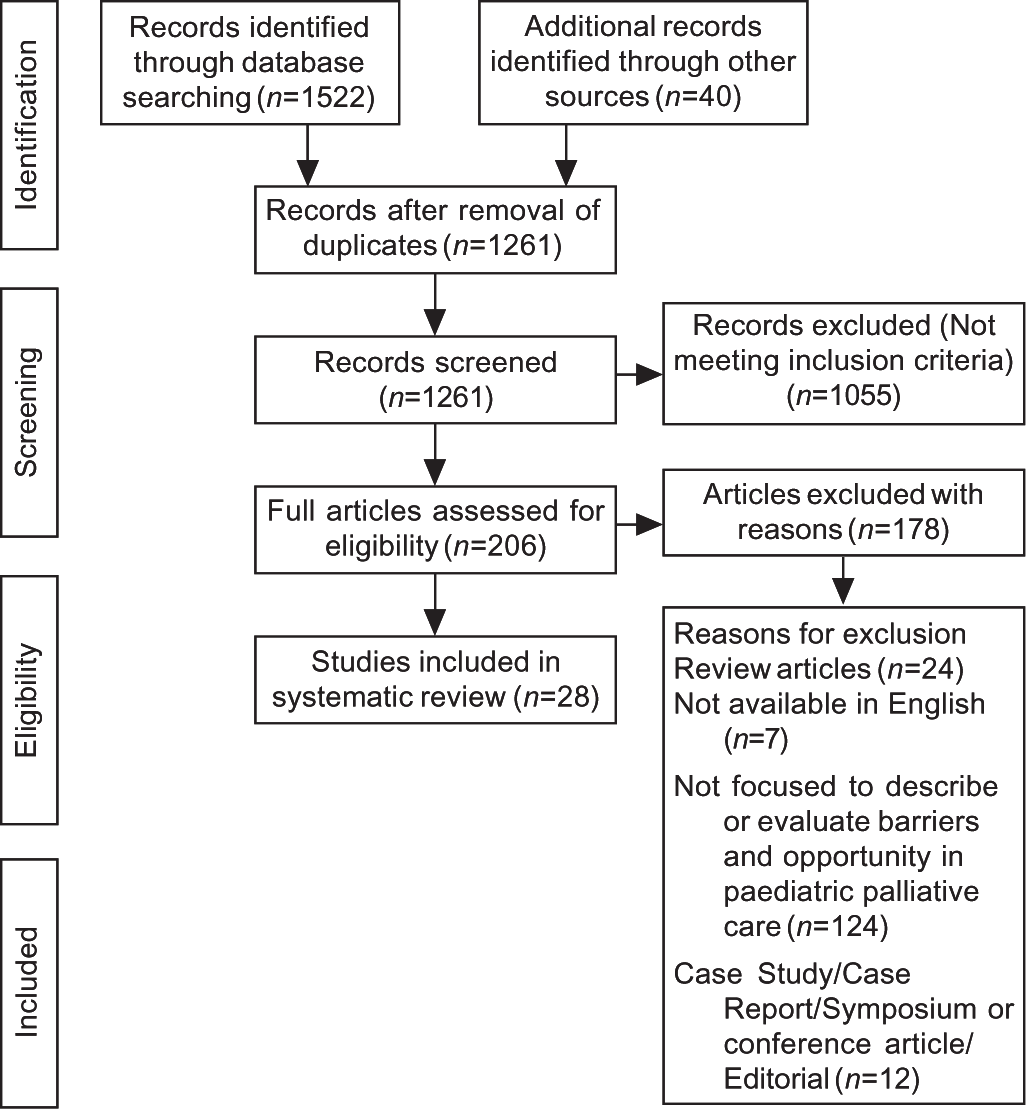
- PRISMA flowchart of search and inclusion of the articles for the systematic review
Data sources and search
We did systematic searches in the databases of PubMed and Scopus for articles published in the past 10 years (January 2011 to December 2021). The population, concept and context (PCC) framework was used to devise a search strategy in an electronic database. The search was conducted using MeSH terms and keywords ‘Palliative care, Hospice care, Terminal care, End of life care, Child, Children, Pediatric, Pediatric, Challenges, Obstacles, Barriers, Opportunities’ in various combinations. The author’s database and secondary bibliographies from the retrieved articles were also searched.
Criteria for inclusion of study in this review
The following criteria were used to include studies in the present systematic review:
Original research articles
Articles focused on assessing challenges or opportunities in providing palliative care to children with life-limiting illnesses
Published within the last 10 years
Written in English
Articles excluded from the review were:
Review articles, editorials, protocols, conference reports or abstracts, guidelines, and policies
Only abstract available through online search
Articles on perinatal palliative care
Study selection
The retrieved studies were exported to Zotero, which was used to remove duplicate articles. Two authors (USA and RG) screened the title and abstracts of the studies as per pre-defined criteria. The full text of the articles was retrieved for further evaluation to ascertain the eligibility to include in the review. The authors (USA, JS and RG) reviewed the studies independently to assess their eligibility. In case of any disagreement, a consensus among the authors was sought for resolution. Reasons for not including the articles were identified and documented.
Qualitative data from each study were compiled in a tabulated form with the following information: (i) citation details: authors, year of publication, and country of the first author; (ii) aim of the study; (iii) population; (iv) method; (v) challenges related to personnel, system, policy and organizational factors; and (vi) recommendation or opportunities to overcome these challenges.
RESULTS
Study characteristics
A total of 1562 articles were found on searching the databases. Title and abstracts of articles were screened and 206 articles were selected for full-text review. Of these, 28 articles dealing with barriers to and opportunities in providing paediatric palliative care services were identified and were included for further consideration in the present systematic review. The characteristics of included studies were extracted and summarized (Table I; available at www.nmji.in).
DISCUSSION
The present systematic review identified many barriers to the provision of palliative care services for children at different levels. These barriers related to policy and system, while others related to organizations or healthcare providers (HCPs). The literature also emphasized suggestions to improve the provision of palliative care among children with life-limiting illnesses.
The barriers to provision of palliative care for children with life-limiting illnesses have been compiled under four broad headings (Fig. 2).

- Barriers to the provision of services to children palliative care
Policy and system-level barriers
It has been observed that there is less focus on palliative care in the state’s policy and strategy framework.8 Bureaucratic hurdles and non-availability of a bridging care system serve as a barrier to provision of palliative care for children.9 Lack of financial resources, pre-employment education regarding palliative care in children, and lack of awareness among policy-makers were found to be the main obstacles at the policy level.10,11 There is a skewed distribution of services related to palliative care in children resulting in limited access.12 Inadequate supply of opioids for pain management, lack of financial resources, large or remote areas of coverage are major constraints to achieving the required reach and quality of services.8
Organizational barriers
Difficulty in maintaining continuity of care due to inadequacy or absence of home-based care or a bridging care system from hospital to home, inadequate workforce and infrastructure of hospitals, variability of factual and emotional knowledge among parents and HCPs are major organizational barriers to the provision of palliative care for children.10,12 Lack of trained workforce, high workload with complexity in care, low rates of referrals, and lack of partnering community service providers are the barriers to providing palliative care to children.13 The non-governmental organizations (NGOs) providing specialized care to children focus only on patients with AIDS and cancer, with some of them exclusively focusing on adults.8 The lack of standardization of palliative care referral practice is a hurdle in initiating palliative care consultations.14 Sometimes non-availability of a support person for the family such as a psychosocial worker or spiritual leader may act as a barrier to providing palliative care to children at the end of life.15
Healthcare provider-related barriers
Frequently reported barriers are lack of knowledge, experience and improper understanding of palliative care for children among HCPs.8,16 However, it has been found that despite adequate knowledge about palliative care, an unfavourable attitude of HCPs, feeling uncomfortable when addressing palliative care requirements, and associating palliative care with end of life or death acts as an obstacle to timely referral to palliative care services for children.17,18
There may be a delay in palliative care consultation due to the non-availability of widely accepted unified practice for implementation, conflict among primary physicians about the consistency of palliative care with curative therapy, and difference of opinion regarding the timing or eligibility of patients.17,19 There is confusion among providers in defining hospice and palliative care with many believing that both share the same definition.20 Physicians’ limited knowledge about the benefits of palliative care, feeling discomfort while raising the topic of palliative care with family, desire to maintain hope, the uncertainty of prognosis, emotional labour in calling palliative care consult, and time constraints are the leading causes of delay in initiating palliative care for children. Many times physicians are resistant to giving up their traditional roles to the palliative care team.12,21,22 Many times more than one physician is involved in the care of a patient and they have differences of opinion about the direction of care.15 HCPs’ reluctance to prescribe or administer morphine also serves as a barrier to adequate pain relief in this population.8
Lack of parental involvement in decision-making including treatment, prognostication, and lack of empathy in communication are also barriers. Parents felt a lack of support from the healthcare team regarding decision-making at the end of life. HCPs give less attention to the family during the illness and there is a lack of bereavement care; providers give much emphasis on symptom management and treatment and do not give attention to the child as a person.9
Lack of appropriate referrals by the paediatricians to a hospice because of ongoing therapy with curative intent has been found to be a barrier.23 Seven broad categories of uncertainties that can delay referral of children to palliative care are: prognostic, informational, individual, communication, relational, collegial and inter-institutional uncertainty.24 HCPs, as well as family, perceive referral to hospice as giving up hope. There is a negative connotation of palliative care due to the synonymous use of the terms end of life and palliative care. Care requirements of children are complex and there is a lack of personnel trained to provide palliative care to them. Language also serves as an obstacle to care.25,26
Palliative care in children is difficult as communication with them requires a different set of skills and building rapport with parents is quite challenging. Care of children suffering from life-limiting illnesses is emotionally intensive and multifaceted for HCPs.27,28 Providers also feel stressed about getting things right for the children and work-related stress.27
Patient and family-related barriers
Family members of the patient may not be willing to use or sometimes even feel offended by the suggestion to introduce palliative care because they have negative connotation of palliative care services. Using the term ‘palliative care’ and ‘end-of-life’ interchangeably or synonymously might have contributed to the negative perception of such services.13,21,26,29–32 Cultural aspects, irrational parental hopes, and incomplete communication may also serve as a barrier to the involvement of palliative services.10 Non-availability of support persons such as religious leaders may cause hindrance in availing the benefits of palliative care services.33 These services are not covered by insurance, therefore reimbursement of expenses for palliative care services was found to be a barrier.23,31 Families are not aware of the benefits and availability of palliative care services.11,13
RECOMMENDATION AND OPPORTUNITIES TO OVERCOME THE BARRIERS/CHALLENGES
In this systematic review, we have identified opportunities to improve palliative care service provisions by appropriate steps at policy, organization, healthcare provider and family levels (Fig. 3).

- Recommendation and opportunities to improve the provision of palliative care for children
At the policy level
Local governments should be aware and empowered to strengthen the health system and increase its capacity to improve provision of palliative care services. Adequate funding, workforce and training of palliative care specialists for children should be supported. There should be guidelines to promote the timely implementation of palliative care services, which should be modified to align with the political and cultural preferences of each country.10,12 Paediatric palliative care should be integrated into the broader health system of every country. It is also important to bring paediatric palliative care on the priority development agenda of policy-makers.8 Patient managers may be introduced to act as a bridge between patients, family and different HCPs and may help in resolving bureaucratic problems.9 Palliative care should be incorporated in the postgraduate, undergraduate, and pre-service training curriculum of HCPs.10,23,28 Empowering nurses to consult paediatric palliative care through policy change may help in the early initiation of palliative care.23 Countries with higher service provisions can take mentorship roles and handhold other countries to develop such services. Guidelines and good practices should be shared across the countries. Opioid demand should be tackled from all sides and an adequate supply of these drugs should be maintained. Facilitative policies should be adopted in prescribing opioids and providing access to them.13,34
At the organizational level
Children are not miniature adults; therefore, it is important to disentangle palliative care for children from palliative care for adults. Palliative care services should be integrated with mainstream health services.11 Adequate provision of a bridging care system should be in place to maintain the continuity of care from hospital to home. Implementing regular team meetings may be beneficial for teamwork. The approach to staffing and recruitment should be flexible to address the shortage of staff.
Proper disclosure of information should be given to parents and family regarding the palliative care services through the use of a more flexible approach in communication.10 Quality of life of the patient and family members can be improved with early initiation of palliative care in the illness trajectory; therefore, the palliative care team should be part of the healthcare team and all providers must be aware of the potential benefits of early initiation of palliative care.23 Organizational heads must support the introduction of multidisciplinary palliative care teams in healthcare facilities and home-based care to ensure continuity of care. It will also help in smooth transitions of care between different care settings. Efforts must be made to reduce the cost of care to mitigate the financial burden of the family.12 Hospice organizations should provide flexible services and may cater to curative treatment needs as well. There should be the provision of concurrent access to palliative care and disease-directed treatment. Further research should be conducted to understand the perspective of parents, paediatricians and other specialists.25 Standards of care should be developed for current and new palliative care services for children to ensure the quality of these services. Continuous research should be done to support the development and maintenance of these services.23 Support must be provided to HCPs to retain them in their roles.28 Training and standardized way of identification of patients requiring secondary or tertiary palliative care services may help to facilitate integration of palliative care.26 Enhancing collaboration for training and capacity building may help to strengthen the delivery of palliative care services for children.11,13
At the HCP level
Lack of knowledge is a commonly identified barrier to the provision of palliative care services, which may be addressed by giving training to HCPs in palliative care for children. It should be integrated into the training or pre-employment education of all health professionals.8,25 Educational strategies for physicians to develop comfort with palliative care patients may be helpful.18,33 HCPs should be open to communication with family and parents, for which training in communication skills is important. They should develop strategies and techniques to deal with difficult situations, breaking bad news, interact with family members and co-workers in difficult situations, and collaborate with other organizations.24 HCPs should reconsider and update their approach regarding palliative care implementation and discussion with parents.19 Shared decision-making, more involvement of parents in deciding on the care of their child, and supporting parents in making end-of-life decisions are critical to remove barriers to palliative care. Professional intimacy should be used cautiously to detect the need of the family.9 HCPs should be experienced in child care and they should be able to speak with non-English-speaking children and their parents. Improving interdisciplinary communication and providing palliative care skill training may help in better coordination and early referral to palliative care.14
At the patient and family level
Targeted educational interventions may be provided to family members and the community regarding the potential benefits of palliative care services.31 This may help in removing their myths or misconceptions and improving the acceptance of palliative care services. Receptive and understanding family members may be identified to explain all the aspects of care and the active involvement of a religious leader may help gain the confidence of the family.15,33
Limitations
Only qualitative studies were included; hence a meta-analysis could not be performed. The published literature may have an inherent component of publication bias.
CONCLUSION
Palliative care services for children are facing many barriers at the level of policy, organization, HCP and patient or family. These barriers can be addressed by adopting research-driven strategies at every level. Adequate and equitable distribution of such palliative care services will help in improving the quality of life of children with life-limiting illness, and their families.
Conflicts of interest
None declared
References
- Definition of Palliative Care. 1998. Available at www.who.int/news-room/fact-sheets/detail/palliative-care (accessed on 15 Jan 2022)
- [Google Scholar]
- National Hospice and Palliative Care Organization (USA) Standards of Practice for Pediatric Palliative Care and Hospice. Available at www.nhpco.org/wp-content/uploads/2019/07/Pediatric_Standards.pdf (accessed on 15 Jan 2022)
- [Google Scholar]
- Assessment of the need for palliative care for children in South Africa In: Int J Palliat Nurs. Vol 20. 2014. p. :130-4. Erratum Int J Palliat Nurs 2014; 20:201
- [CrossRef] [PubMed] [Google Scholar]
- Metronomic chemotherapy vs best supportive care in progressive pediatric solid malignant tumors: A randomized clinical trial. JAMA Oncol. 2017;3:1222-7.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life assessment in retinoblastoma: A cross-sectional study of 122 survivors from India. Pediatr Blood Cancer. 2016;63:313-17.
- [CrossRef] [PubMed] [Google Scholar]
- Integrating palliative care and symptom relief into primary health care: A WHO guide for planners, implementers and managers. 2018. Geneva: WHO; Available at www.who.int/publications/i/item/integrating-palliative-care-and-symptom-relief-into-primary-health-care (accessed on 15 Jan 2022)
- [Google Scholar]
- Alleviating the access abyss in palliative care and pain relief-an imperative of universal health coverage: The Lancet Commission report In: Lancet. Vol 391. 2018. p. :1391-454. Erratum Lancet 2018;391:2212
- [Google Scholar]
- Barriers in care for children with life-threatening conditions: A qualitative interview study in the Netherlands. BMJ Open. 2020;10:e035863.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to palliative care in pediatric oncology in Switzerland: A focus group study. J Pediatr Oncol Nurs. 2020;37:35-45.
- [CrossRef] [PubMed] [Google Scholar]
- Qualitative situational analysis of palliative care for adolescents with cancer and HIV in South Africa: Healthcare worker perceptions. BMJ Open. 2019;9:e023225.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to the early integration of palliative care in pediatric oncology in 11 Eurasian countries In: Cancer. Vol 126. 2020. p. :4984-93. Erratum Cancer 2021;127:4517
- [CrossRef] [PubMed] [Google Scholar]
- Paediatric palliative care in the Asia Pacific region: Where are we now? BMJ Support Palliat Care. 2017;7:17-22.
- [CrossRef] [PubMed] [Google Scholar]
- Initiating palliative care referrals in pediatric oncology. J Pain Symptom Manage. 2021;61:81-9.e1.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric end-of-life care barriers and facilitators: Perception of nursing professionals in Jordan. Indian J Palliat Care. 2017;23:199-206.
- [CrossRef] [PubMed] [Google Scholar]
- Provision of palliative and hospice care to children in the community: A population study of hospice nurses. J Pain Symptom Manage. 2019;57:241-50.
- [CrossRef] [PubMed] [Google Scholar]
- Underlying barriers to referral to paediatric palliative care services: Knowledge and attitudes of health care professionals in a paediatric tertiary care centre in the United Kingdom. J Child Health Care. 2014;18:19-30.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with knowledge and comfort providing palliative care: A survey of pediatricians in Mexico. J Palliat Care. 2019;34:132-8.
- [CrossRef] [PubMed] [Google Scholar]
- The timing and circumstances of the implementation of pediatric palliative care in Hungarian pediatric oncology. Eur J Pediatr. 2018;177:1173-9.
- [CrossRef] [PubMed] [Google Scholar]
- Strengths, gaps, and opportunities: Results of a statewide community needs assessment of pediatric palliative care and hospice resources. J Pain Symptom Manage. 2020;60:512-21.e7.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric oncology providers' perceptions of barriers and facilitators to early integration of pediatric palliative care. Pediatr Blood Cancer. 2013;60:1875-81.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric oncology providers' perceptions of a palliative care service: The influence of emotional esteem and emotional labor. J Pain Symptom Manage. 2018;55:1260-8.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge, beliefs, and behaviors related to palliative care delivery among pediatric oncology health care providers. J Pediatr Oncol Nurs. 2018;35:247-56.
- [CrossRef] [PubMed] [Google Scholar]
- Seven types of uncertainty when clinicians care for pediatric patients with advanced cancer. J Pain Symptom Manage. 2020;59:86-94.
- [CrossRef] [PubMed] [Google Scholar]
- Barriers to hospice for children as perceived by hospice organizations in North Carolina. Am J Hosp Palliat Care. 2012;29:171-6.
- [CrossRef] [PubMed] [Google Scholar]
- Defining the boundaries of palliative care in pediatric oncology. J Pain Symptom Manage. 2020;59:1033-42.e1.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring the rewards and challenges of paediatric palliative care work-a qualitative study of a multi-disciplinary children's hospice care team. BMC Palliat Care. 2017;16:73.
- [CrossRef] [PubMed] [Google Scholar]
- Community palliative care nurses' challenges and coping strategies on delivering home-based pediatric palliative care. Am J Hosp Palliat Care. 2017;34:125-31.
- [CrossRef] [PubMed] [Google Scholar]
- The conceptual understanding of pediatric palliative care: A Swiss healthcare perspective. BMC Palliat Care. 2019;18:55.
- [CrossRef] [PubMed] [Google Scholar]
- Perceptions of pediatric palliative care among physicians who care for pediatric patients in South Korea. J Palliat Med. 2020;23:346-52.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with perceived barriers to pediatric palliative care: A survey of pediatricians in Florida and California. Palliat Med. 2012;26:268-74.
- [CrossRef] [PubMed] [Google Scholar]
- Perceptions of barriers and facilitators to early integration of pediatric palliative care: A national survey of pediatric oncology providers. Pediatr Blood Cancer. 2018;65:e26996.
- [CrossRef] [PubMed] [Google Scholar]
- Nursing staff's perception of barriers in providing end-of-life care to terminally ill pediatric patients in southeast Iran. Am J Hosp Palliat Care. 2016;33:115-23.
- [CrossRef] [PubMed] [Google Scholar]
- Palliative care for children with cancer in the Middle East: A comparative study. Indian J Palliat Care. 2017;23:379-86.
- [CrossRef] [PubMed] [Google Scholar]
- Qualitative analysis of palliative care for pediatric patients with cancer at Bugando Medical Center: An evaluation of barriers to providing end-of-life care in a resource-limited setting. J Glob Oncol. 2018;4:1-10.
- [CrossRef] [PubMed] [Google Scholar]




