Translate this page into:
Feasibility of mobile telephonic follow-up among patients with alcohol dependence syndrome
Corresponding Author:
Susmita Chandramouleeswaran
Department of Psychiatry, Christian Medical College, Vellore, Tamil Nadu
India
susmit1984@yahoo.co.in
| How to cite this article: Nandyal M, Chandramouleeswaran S, Braganza D. Feasibility of mobile telephonic follow-up among patients with alcohol dependence syndrome. Natl Med J India 2019;32:77-82 |
Abstract
Background. Losses to follow-up impact the collection of outcomes among patients with alcohol dependence syndrome (ADS). We aimed to study the feasibility and acceptability of using telephonic contact as a means of following up new patients with ADS. The outcomes assessed were complete abstinence at the end of 6 months and associated factors.Methods. We followed up a cohort of 54 new patients diagnosed with ADS after 6 months, in the psychiatry department of a tertiary care hospital in India. We also assessed sociodemographic, alcohol-related, medical and treatmentrelated details of the patients; and scores on the Short Alcohol Dependence Data Questionnaire, Rotter's scale for the locus of control, and the Clinical Institute of Withdrawal Assessment of Alcohol scale-revised. The primary outcome was complete abstinence at the end of 6 months. The data at follow-up were collected through a combination of in-person and telephonic interviews with the patients and caregivers and supplemented with chart reviews.
Results. Follow-up at 6 months could be carried out for 51 of 54 patients enrolled (94.4%; 32 through direct, and 19 through telephonic interviews). The proportion of patients who achieved and maintained complete abstinence during this period was 27.5%. The factors found to be associated with abstinence were regularity of follow-up, adherence to medicines and having had the habit of drinking alcohol with friends, as opposed to solitary drinking.
Conclusion. Using mobile telephonic technology, we were able to obtain an excellent follow-up and improve the collection of outcomes by 35.2% at the end of a 6-month period among new patients with ADS. This potentially effective tool is widely available and cost-effective, and could have a role in improving outcomes among patients with ADS.
Introduction
A practical problem in obtaining outcomes from patients with alcohol dependence syndrome (ADS) is the poor rate of follow- up. [1],[2] This is especially true in a large developing country such as India, which lacks financial and material resources for home-based follow-up, and which has patients often presenting to hospitals from distant locations due to lack of adequate local health services. The range of follow-up varies from 10% to 60% one year after the index visit, with the use of postal services to remind patients to attend the sessions.2,3 With home-based follow- up using social workers, losses up to 20% are reported due to patients being untraceable or having gone for work as migrant labour. [1] This loss to follow-up impacts negatively the quality of outcome data obtained, and existing studies on factors associated with abstinence have not been able to reach a strong consensus. [5],[6],[7] With widespread mobile connectivity and availability of cheap handsets, contacting patients using mobile phones could be an effective means to improve follow-up. This would be especially beneficial for patients presenting from distant locations and those who might work as migrant labourers. In India, both patients and families are involved in the treatment process, and therefore obtaining information from the families even via telephone is likely to improve the veracity of the data obtained.
We studied the feasibility and acceptability of following up patients with ADS using mobile phones, in the psychiatry department of a large tertiary care hospital. The outcomes estimated were proportion of new patients with ADS who achieved and maintained abstinence over a 6-month period after undergoing routine treatment according to hospital protocols, and to study factors associated with abstinence.
Methods
This pilot study was done by the Department of Psychiatry-Unit 2, Christian Medical College and Hospital, Vellore, India. The study design was of a prospective cohort. The Department of Psychiatry has 122 beds and is a tertiary care psychiatric centre catering to patients from all over India, apart from having a primary catchment area covering three southern states.
All new patients who presented to the outpatient services of our Unit from 1 October 2012 to 31 March 2013, diagnosed with ADS according to the International Classification of Diseases-10 by a psychiatrist, were included in the study after obtaining written informed consent. In case the person was not cognitively intact at the time of initial presentation, the informed consent was obtained from a primary caregiver. Once the patients regained their cognitive ability, we re-obtained informed consent from them. Permission to contact the patient and caregiver for review after 6 months was also obtained, along with their telephone numbers. Whenever available, the telephone number of the caregiver was also obtained with their permission. Patients with other psychiatric illness and permanent cognitive deficits, such as dementia, were excluded. The study was cleared by the Institutional Review Board. All the study patients continued to receive care as per hospital protocols during these 6 months. This included outpatient, emergency, inpatient stay and therapy, and appropriate pharmacological treatment according to the needs of the patients, carried out by the multidisciplinary team.
The primary investigator did an initial semi-structured interview to document sociodemographic details, alcohol use and family data. This included factors such as age, gender, marital status, employment, education, distance from the hospital, distance from the nearest liquor shop, patterns of alcohol use, family history of alcohol use and comorbid medical illness.
The questionnaire and scales administered were as follows:
- Short Alcohol Dependence Data Questionnaire (SADD) to assess the severity of alcohol use. It has 15 items rated on a Likert scoring system from 0 to 3. A total score of 1-9 indicates low dependence, 10-19 medium dependence and > 20 indicates high levels of dependence.
- The Clinical Institute Withdrawal Assessment of Alcohol Scale, Revised (CIWA-Ar) was administered to measure the severity of withdrawal symptoms. It has 10 items, 9 of which are rated from 0 to 7, and 1 from 0 to 4.
- Rotter′s scale was administered to categorize the locus of control into internal or external categories. It has 23 items with two possible responses to each question: one representing an internal, and the other an external locus of control. Higher scores indicate an external locus of control.
Follow-up
Six months after the initial assessment, the patient was contacted by the primary investigator over the phone to come in person for the second study assessment. Whenever possible, caregivers were also requested to come with the patient. An interview with the patient was conducted by the primary investigator, and a hospital chart review was done. The details provided by the patient and caregiver were substantiated, and cross-checked with data from the patient′s chart, to overcome recall bias.
Patients who were unable to come for the second assessment for any reason, were interviewed over the telephone. Information was also collected from the available primary caregivers over the telephone. This was cross-checked with the information in the chart, and in case of loss to follow-up, the information collected in the chart at the last review was taken for final analysis. The outcomes assessed were the number of abstinent days, number of lapses and relapses and details of treatment. All the data were kept confidential and personal identifiers were removed to make the data untraceable.
Statistical analysis was performed using SPSS (Statistical Package for Social Sciences, IBM, USA) version 16.0. Descriptive statistics were used to assess the sociodemographic profile of the participants. Frequencies were calculated for the categorical variables. Measures of central tendency were described as mean or median, depending on the distribution of the variable, for continuous variables. The sample was divided into two groups-- an abstinent and a non-abstinent group. The risk factors for non- abstinence were analysed using appropriate non-parametric tests such as chi-square test. Crude odds ratios and their 95% confidence intervals were calculated. For the continuous predictor variable, we used logistic regression to find the odds ratios and their 95% confidence interval. A value of p<0.05 was taken as a cut-off for statistical significance.
Results
We recruited 54 patients during the study period through convenience sampling. All the patients we approached were willing to participate in the study and to give their mobile phone contact details. Of the original 54 patients, 3 could not be contacted over the phone at the time of follow-up. Therefore, 51 patients were followed up after 6 months (32 reported in person and 19 communicated over the phone). Of these, in 48 cases, we were able to collect information from the caregivers as well.
Sociodemographic details
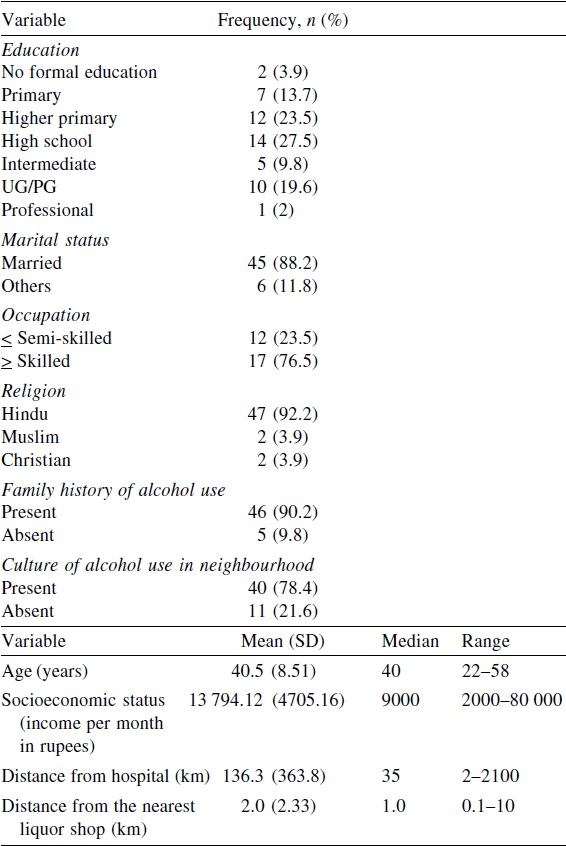
All the participants were males and their mean age was 40.5 years (standard deviation 8.51, range 22-58 years). Of the 51 participants who completed the study, 45 were married (88.2%). The majority of the participants were skilled labourers (33.3%). The median distance between their homes and the hospital was 35 km [Table - 1].
Clinical characteristics
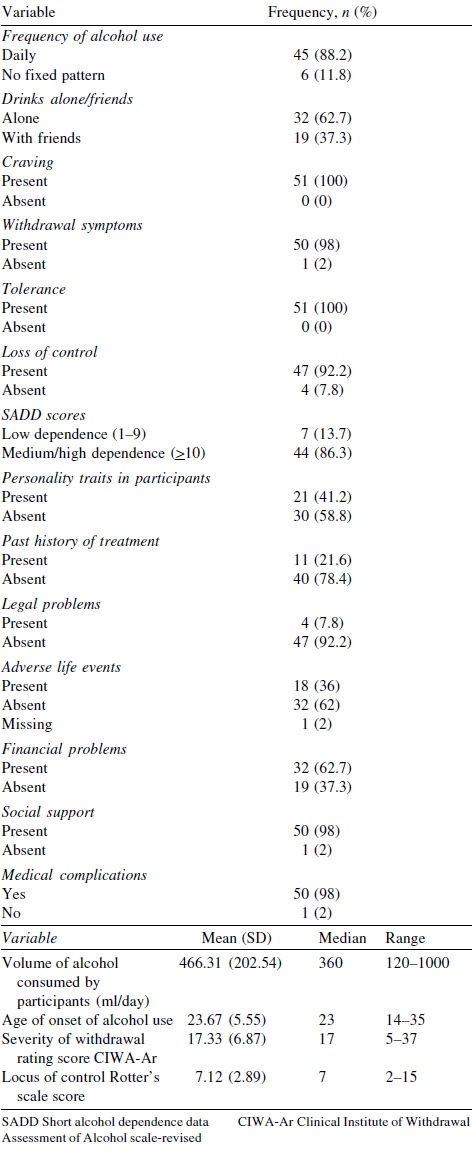
At the time of presentation, all but one of the patients were in withdrawal (50/51). Forty-four (86.3%) participants had medium- to-high dependence on alcohol. Forty-five (88.2%) participants drank every day, and all experienced craving and tolerance. All but one participant (98%) reported a history of withdrawal symptoms. A vast majority, i.e. 47 (97.2%) participants reported loss of control in initiating and stopping alcohol use and over the quantities consumed. Eleven (21.6%) patients had received treatment elsewhere before presenting to us [Table - 2].
Outcomes at follow-up
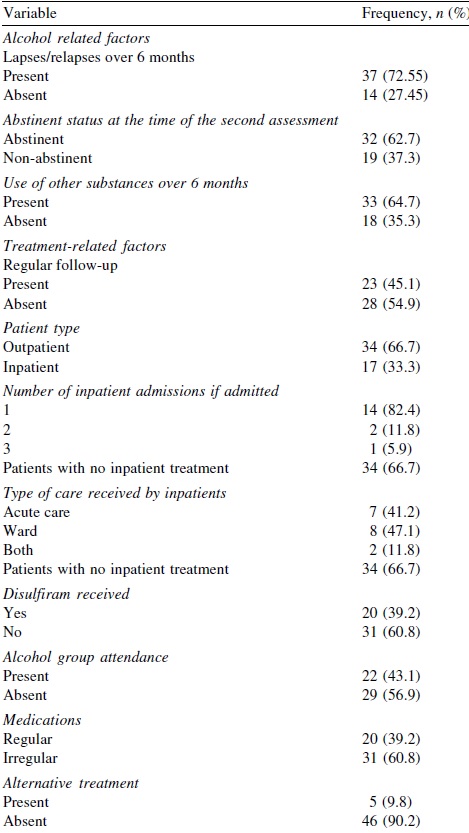
At the end of 6 months from the index visit, 32 (62.7%) participants reported abstinence for 1 month at the time of follow-up. Fourteen (27.5%) were abstinent throughout the 6 months of follow-up.
Thirty-three (64.7%) participants were using other substances during the second assessment compared to 39 participants who were using them at the beginning of the study [Table - 3].
Factors associated with abstinence
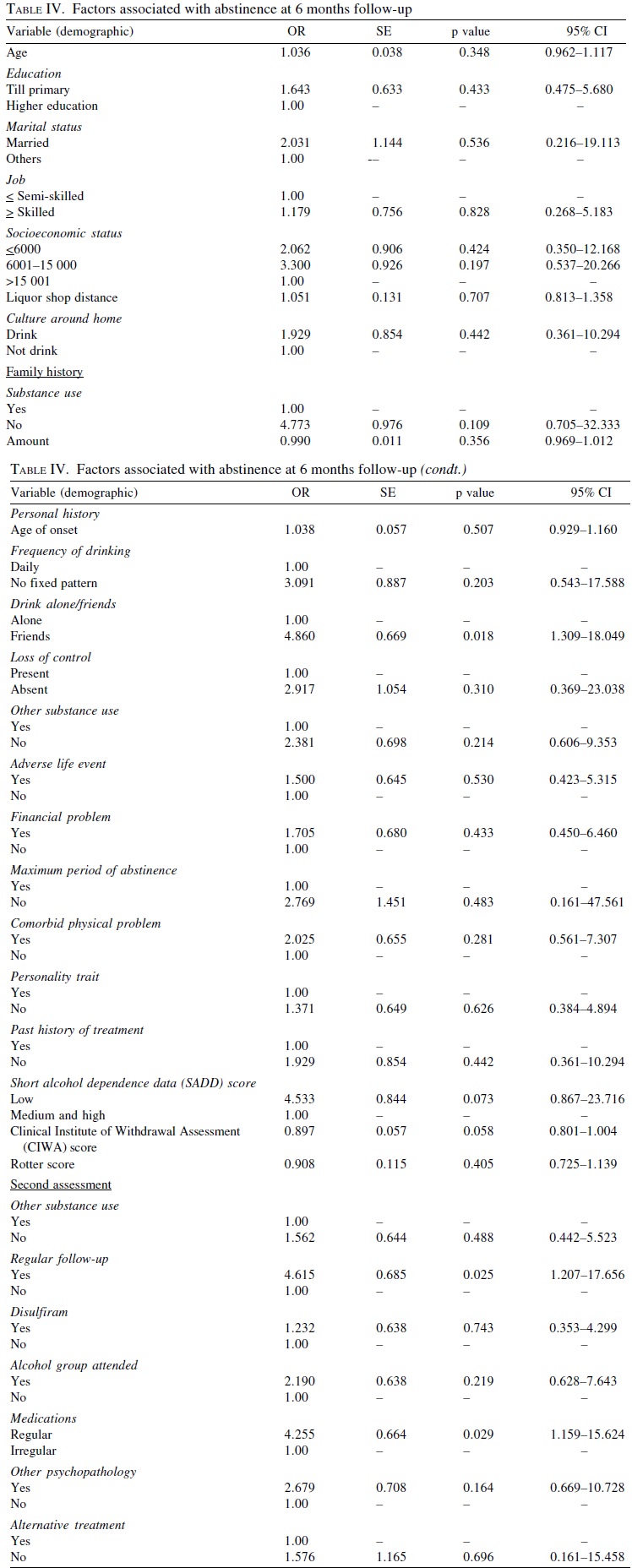
The factors related to abstinence after 6 months of follow-up were studied through univariate analysis [Table - 4]. It was found that the pattern of drinking alcohol with friends (as opposed to solitary drinking), compliance with drug therapy, and regular follow-up were associated with complete abstinence. Other factors including baseline characteristics, family and history, treatment with disulfiram, distance from the liquor shop and hospital were not found to have any statistical significance.
Analysis of missing participants
The analysis conducted on the four participants who were unavailable for the second assessment (by using the baseline characteristics and chart review), did not reveal any significant difference from those who had completed the follow-up. The on person who had died, due to a road traffic accident, while sober. Statistical analysis could not be performed due to the small number of missing participants.
Discussion
All the patients we approached for recruitment into the study were willing to share their contact details and be contacted over the phone after 6 months. Despite largely living in rural areas and having a median family income of ₹9000/month, all participants had access to mobile phones with adequate coverage.
Thirty-two of the 54 patients (59.2%) enrolled in the study were able to report in person at the end of 6 months. We were able to collect satisfactory data from 19 other patients over the phone, by talking to the patient and/or caregiver, substantiated with information from the chart review. Only 4 of the initial 54 patients (7.4%) could not be followed up (1 patient had died and 3 were not contactable over the phone). The availability of information from the caregivers for 48 of the 51 patients added value to the quality of the information obtained. Discrepancies between the chart data, patient and caregiver reports were used to obtain subjective evidence of the veracity of the information provided over the phone, to overcome recall bias, and helped to clarify doubtful information.
All participants recruited for the study were males, probably because the prevalence of ADS was more among males; this was consistent with previous findings.8-10 It could also suggest that women in India with alcohol use disorders did not present to healthcare services because of the social stigma. The majority of participants belonged to the lower middle socioeconomic status and were mostly semi-skilled workers, farmers and shopkeepers, with an educational profile ranging from higher primary to high school. This could be a reflection of the primary catchment area served by this hospital, as it is located in a tier 2 city. The number of married participants grossly outnumbered other categories, probably reflecting the social trend in India where marriage is the norm. [9] The odds of a married person remaining abstinent were two times higher than that of an unmarried person. However, this did not reach statistical significance due to smaller numbers in the unmarried category; this was not robustly supported by previous studies. [11]
Follow-up outcomes
The proportion of participants with complete abstinence during 6 months was 27.5%. This agreed with the rates of abstinence in previous studies, which have varied between 30% and 50% due to methodological and cultural differences. [2] It is possible that the lower rate of abstinence in our study was due to the higher rates of follow-up possible through mobile phone contact. We would not have obtained data on 19 of 51 patients without this method, and we hypothesize that the retention of these patients could have reduced the abstinence rate as these were patients who had dropped out of regular hospital visits.
We found that 72% of participants had lapses or relapses during the follow-up period, and 62% of the participants were abstinent for 1 month at the time of follow-up.
Factors associated with abstinence
Studies that assessed patient parameters for abstinence [1],[3],[11],[12],[13],[14],[15],[16] have revealed multiple associated factors including personal (older age, female gender and better education), alcohol use (lower levels of alcohol use and later age of onset), comorbid condition (comorbid depression) and treatment-related factors (adherence to Alcoholics Anonymous, disulfiram use, regular follow-up). The regular follow-up, duration of disulfiram use, and ongoing support have been associated with abstinence in India. [2],[8]
In our study, the odds of participants without a family history of alcohol dependence remaining abstinent was almost five times that of those with a positive family history, although not statistically significant. This is consistent with prior studies and probably indicates both the role of genetics and a familial culture of problem drinking in the initiation and maintenance of alcohol use disorders. [16] A history of drinking with friends (as opposed to drinking alone) was found to be significantly associated with abstinence (OR=4.86, p=0.018). This indicated that participants who had external cues derived greater benefits and had greater success at being abstinent compared to participants who drank alone, who probably had more internal cues. Hardly any study has addressed this variable in particular. However, a recent study established that peer pressure was the most common cause for relapse. [17] In the abstinent group, the odds of being regular on follow-up was four times that of the non-abstinent group (OR=4.62, p=0.025), in keeping with previous studies.5 In the abstinent participant group, the odds of being on regular medication were four times those of the non-abstinent group (OR=4.26, p=0.029). A subgroup analysis revealed that use of disulfiram was not associated with abstinent rates. This is contrary to studies that revealed that disulfiram was associated with better outcomes.2,8 This finding probably indicated that unless associated with adherence, disulfiram use in itself did not improve abstinence. We did not find significant associations between abstinence at 6 months and factors such as group therapy attendance, volume and type of alcohol used, distance from hospital and liquor shop, SADD, Rotter′s and CIWA scores, comorbid conditions, history of treatment and age of onset of alcohol use. This was consistent with previous Indian studies that revealed no association between good outcome and pre-treatment variables.
An interesting, though non-significant, finding of our study is that people who earned less than ₹6000/month had a lower chance of being abstinent at 6 months than those earning more. This association suggested that higher income and better education profile could favour abstinence. This is consistent with findings that ADS is more common among those from the lower socioeconomic strata. [18]
Strengths and limitations of the study
Of the 54 patients initially enrolled in this pilot study, 3 were lost to follow-up, and 1 died during the study period. A follow-up rate of 94% (51 patients) was a positive finding of the study. Had we not used mobile phones for follow-up, we would not have obtained the data of 19 (35.2%) of the 54 patients who were enrolled. The short period of follow-up of 6 months in this study was to assess the feasibility of using telephonic contact to improve follow-up. Our results suggest that this method could also potentially be used over longer durations. The pragmatic nature of the study with broad inclusion criteria was another strength. However, while the therapy received by the participants was in keeping with standard care, the care received by each participant was individualized. Therefore, it is possible that unrecorded variations in these affected the outcomes. While telephonic contact improved the number of patients who were followed up, there could be a difference in the veracity of the data obtained via telephone as opposed to direct interviews. There is also a possibility of information bias as many of the assessments were based on recall. We have tried to overcome these by using multiple sources of information including caregivers and hospital charts. Some of the questions were personal and were potentially stigmatizing and could have induced false answers, as could a personality factor of deceptiveness in some substance users. While in this study we did not assess the effect of regular contact using a mobile phone in improving abstinence rates, our findings suggest that this is a feasible and acceptable method, and we aim to study this in future studies.
Conclusions
We were able to use mobile telephones effectively to improve follow-ups in patients with ADS. Our study showed that patients with ADS and their caregivers were receptive to be contacted over the phone. Thus, this widely available and cost-effective technology could be increasingly used to improve adherence and follow-up, and needs to be tested over longer durations of follow-up.
Acknowledgement
We received funding from the CMC Vellore internal research grant.
Conflicts of interest. None declared
| 1. | Nadkarni A, Weiss HA, Naik A, Bhat B, Patel V. The six-year outcome of alcohol use disorders in men: A population based study from India. Drug Alcohol Depend 2016; 162: 107-15. [Google Scholar] |
| 2. | Abraham J, Chandrasekaran R, Chitralekha V. A prospective study of treatment outcome in alcohol dependence from a deaddiction centre in India. Indian J Psychiatry 1997; 39: 18-23. [Google Scholar] |
| 3. | Kar N, Sengupta S, Sharma P, Rao G. Predictors of outcome following alcohol deaddiction treatment: A prospective longitudinal study for one year. Indian J Psychiatry 2003; 45: 174-7. [Google Scholar] |
| 4. | Prasad R. Alcohol use on the rise in India. Lancet 2009; 373: 17-18. [Google Scholar] |
| 5. | Heramani Singh N, Sharma SG, Pasweth AM. Psychiatric co-morbidity among alcohol dependants. Indian J Psychiatry 2005; 47: 222-4. [Google Scholar] |
| 6. | Soyka M, Schmidt P. Outpatient alcoholism treatment-24-month outcome and predictors of outcome. Subst Abuse Treat Prev Policy 2009; 4: 15. [Google Scholar] |
| 7. | Terra MB, Barros HM, Stein AT, Figueira I, Athayde LD, Ott DR, et al. Predictors of relapse in 300 Brazilian alcoholic patients: A 6-month follow-up study. Subst Use Misuse 2008; 43: 403-11. [Google Scholar] |
| 8. | Walter H, Gutierrez K, Ramskogler K, Hertling I, Dvorak A, Lesch OM. Gender- specific differences in alcoholism: Implications for treatment. Arch Womens Ment Health 2003; 6: 253-8. [Google Scholar] |
| 9. | Room R, Graham K, Rehm J, Jernigan D, Monteiro M. Drinking and its burden in a global perspective: Policy considerations and options. Eur Addict Res 2003; 9: 165-75. [Google Scholar] |
| 10. | O'Malley PM, Johnston LD. Epidemiology of alcohol and other drug use among American college students. J Stud Alcohol Suppl 2002; s14: 23-39. J Stud Alcohol Suppl 2002; s14: 23-39.'>[Google Scholar] |
| 11. | Kuruvilla PK, Vijayakumar N, Jacob KS. A cohort study of male subjects attending an alcoholics anonymous program in India: One-year follow-up for sobriety. J Stud Alcohol 2004; 65: 546-9. [Google Scholar] |
| 12. | Hurcombe R, Bayley M, Goodman M. Ethnicity and alcohol: A review of the UK literature. York, UK: Joseph Rowntree Foundation; 2010. [Google Scholar] |
| 13. | Gureje O, Mavreas V, Vazquez-Barquero JL, Janca A. Problems related to alcohol use: A cross-cultural perspective. Cult Med Psychiatry 1997; 21: 199-211. [Google Scholar] |
| 14. | Miller WR, Mount KA. A small study of training in motivational interviewing: Does one workshop change clinician and client behavior? Behav Cogn Psychother 2001; 29: 457-71. [Google Scholar] |
| 15. | Gual A, Bravo F, Lligoña A, Colom J. Treatment for alcohol dependence in Catalonia: Health outcomes and stability of drinking patterns over 20 years in 850 patients. Alcohol Alcohol 2009; 44: 409-15. [Google Scholar] |
| 16. | Sharma HK, Tripathi BM, Pelto PJ. The evolution of alcohol use in India. AIDS Behav 2010; 14 (1 Suppl):S8-S17. [Google Scholar] |
| 17. | May PA, Gossage P. New data on the epidemiology of adult drinking and substance use among American Indians of the northern states: Male and female data on prevalence, patterns, and consequences. Am Indian Alsk Native Ment Health Res 2001; 10: 1-26. [Google Scholar] |
| 18. | Grant BF. The impact of a family history of alcoholism on the relationship between age at onset of alcohol use and DSM-IV alcohol dependence: Results from the national longitudinal alcohol epidemiologic survey. Alcohol Health Res World 1998; 22: 144-7. [Google Scholar] |
Fulltext Views
1,700
PDF downloads
750




