Translate this page into:
Footwear in the causation and prevention of foot ulcers in diabetes mellitus
2 Department of Distance Education, Christian Medical College, Vellore 632004, Tamil Nadu, India
Corresponding Author:
Ramaswamy Premkumar
4, Vallalr Street Thirunagar, Katpadi Township West, Vellore 632006, Tamil Nadu
India
prem@jamkhed.org
| How to cite this article: Premkumar R, Rajan P, Rima J, Richard J. Footwear in the causation and prevention of foot ulcers in diabetes mellitus. Natl Med J India 2017;30:255-261 |
Abstract
Background. Inappropriate footwear may be a major cause of foot ulceration among patients with diabetic neuropathy in India. No study has specifically examined the types of footwear or its components in patients with diabetes mellitus and their role in causing foot ulcers. We analysed the role of commonly used footwear in India in inducing first foot ulcers (FFU) in people with diabetes.Methods. Of 4800 patients with diabetes attending our centre over 1 year, 301 had FFU from different causes. Sixty-six patients with diabetic neuro-/vasculopathy presenting with ulcers due to footwear were included as cases. An equal number of patients with diabetes but without foot ulcers were enrolled as controls. Cases and controls were matched demographically and clinically for type of diabetes, metabolic control, duration of diabetes, comorbid conditions and foot neurovascular status. We did a detailed foot examination for neurological, vascular and wound status. We also evaluated the footwear in both groups.
Results. In one-fifth of 335 limbs (301 patients), the primary cause for the FFU was use of inappropriate footwear. The patients used seven different models of footwear, six of which were found to be inappropriate. The straps of footwear caused over 50% of ulcers. Another one-third were due to penetration of sharp objects through the outer sole of footwear; among these cases, 1 3.6% of ulcers were caused by not using soft inner soles.
Conclusions. The use of softer insole is least effective in preventing foot ulcers. Similarly, straps contribute to a higher percentage of foot ulcers. Foot ulcers can be prevented by a combination of soft insole, with midsole and hard outsole with proper back counter and adjustable front and back straps.
Introduction
Diabetic foot infection and ulceration is the most common reason for lower limb amputation.[1] To prevent such foot ulcers we need to know the causes. Multiple factors have been postulated for the occurrence of infection and ulceration that lead to amputation. These include walking barefoot, illiteracy, low socioeconomic status, late presentation, ignorance about diabetic foot care among primary care physicians, and belief in alternative systems of medicine.[2],[3],[4] Many studies have assessed the benefit of footwear and shoes in the prevention of foot ulceration and its recurrence in people with diabetes.[5],[6],[7],[8] Inappropriate footwear has also been implicated as one of the primary causes of foot ulcers.[9] However, no study has analysed the type of footwear used by people with diabetes during the first foot ulcer (FFU) episode and its causes. Similarly, little research has focused on the role of soft or hard inner soles, outer soles and straps in the prevention/causation of ulcers.
We surveyed the type of footwear used and attempted to answer the following: (i) What is the role of footwear in the prevention or causation of FFUs? (ii) What kind of footwear/ footwear component(s) such as uppers/straps, inner soles and outer soles either prevent or cause ulcers? (iii) What type of injury is caused by footwear, and at which site?
Methods
We collected data from our centre at Karigiri in southern India, which serves a population of both rural and urban residents of Vellore town. Around 4800 patients attended the Karigiri centre for treatment of diabetes during the 1-year study period.
Inclusion and exclusion criteria
Patients who had type 1 or 2 diabetes with FFU due to footwear-related causes, and diabetic neuropathy or vasculopathy were included. Controls were individuals with diabetic neuropathy or vasculopathy but with no past or present foot ulcer. Patients with other causes of peripheral neuropathies such as leprosy and/or recurrent foot ulcers and foot deformities were excluded. Patients and controls were matched demographically and clinically. The clinical features matched were type of diabetes, metabolic control, duration of diabetes and any existing comorbid conditions.
We defined FFU as a full-thickness skin lesion below the ankle which either occurred for the first time after the diagnosis of diabetes or when the patient, unaware of his/her diabetes, sought medical assistance with foot ulcer as the presenting symptom and was diagnosed to have diabetes.
Data collection
Both patients and controls were known to have diabetes mellitus (either at the time of data collection or before enrolment). The details regarding type of diabetes and duration up to the point of data collection were obtained for both patients and controls. Additional demographic information such as age, gender, education and occupation were also obtained from the patients and controls. The diagnostic criteria for diabetes mellitus were FPG >126 mg/dl on at least two occasions.[11] An HbA1c <6.5% was considered as well-controlled blood sugar while >6.5% was considered as uncontrolled.[12]
Details on disabling comorbid conditions were obtained from patients and controls. Evidence of the following was recorded: (i) severe visual impairment defined as inability to read a newspaper after correction; (ii) end-stage renal disease, defined as need for renal replacement therapy ; (iii) heart failure and/or angina pectoris as per the New York Heart Association classification 3 and 4;[13] and/or (iv) mobility impairment which refers to inability to stand or walk without help.[1]
Examination of the foot
A detailed neurological, vascular and wound evaluation was done for the patients. In the controls a neurological and vascular evaluation was done.
Neurological evaluation. We identified patients with loss of protective sensation using the following tests. The data collectors were blinded to the study classification of the patients.
- Touch pressure sensation. No. 10 g Semmes-Weinstein monofilament (5.07) was used to test protective sensation. The 10-foot examination sites suggested by Singh et al.[10] were tested. If the patient was unable to localize two or more, it was considered as loss of protective sensation due to diabetic peripheral neuropathy.[10]
- A biothesiometer was used to test sense of vibration at two sites, one on the dorsum of the hallux and the other over the medial malleolus. Inability to detect a vibration perception of >25 V in these sites was considered as a severe loss of vibratory sense due to diabetic peripheral neuropathy.
- Pain stimuli: This was done with the use of a neuro-tip to differentiate between sharp and blunt objects. If at two or more of the 10-foot examination sites (same as for touch sensation[10]) the patient was not able to appreciate pain stimuli, it was considered to be due to diabetic neuropathy.
If any two of the above three neurological examinations were abnormal, the limb was considered to be neuropathic.[14]
Vascular evaluation. Vascularity was assessed by the presence of claudication or rest pain, by checking the pedal pulses, and by measuring the ankle-brachial pressure index (ABPI) using a handheld Doppler device. An ABPI of <0.9 and/or two absent pedal pulses, namely, dorsalis pedis and posterior tibial pulse in the foot with the ulcer was considered to represent vasculopathy.[15] Based on the above examinations, the foot was categorized as neuropathic, ischaemic or neuro-ischaemic.
Evaluation of the wound. Ulcers were graded at the time of enrolment, based on the PEDIS (Perfusion, Extent, Depth, Infection and Sensation) system developed by the International Consensus on the Diabetic Foot for the classification of patients for clinical research purposes.[1] The foot lesion(s) was marked on a foot map divided into 10 areas [Figure - 1]. The ulcer was considered infected if two or more of the following signs were present: frank pus, local warmth, erythema, lymphangitis, oedema, pain, fever and foul smell (as per Eurodiale definition).[1]
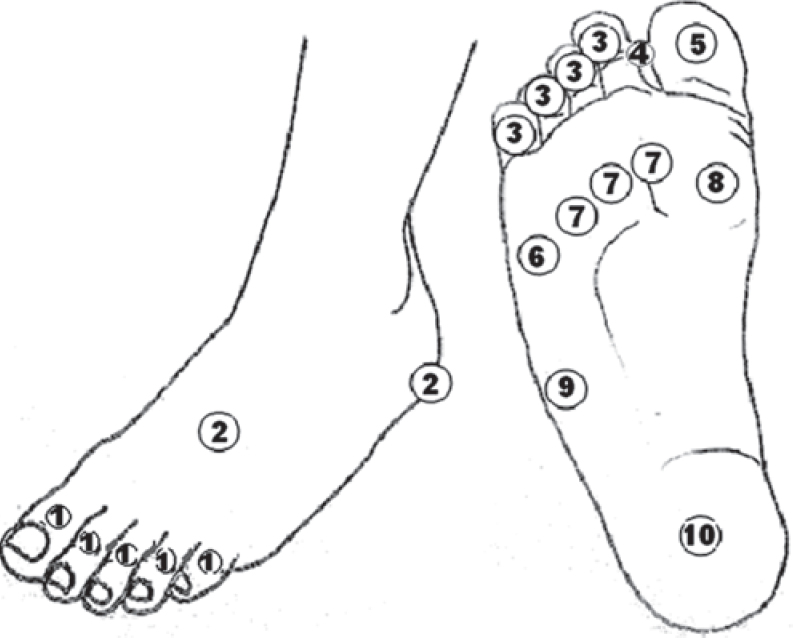 |
| Figure 1: Division of the foot for mapping an ulcer—1. Dorsum of the toes; 2. Dorsal and lateral aspect of the foot (except toes); 3. Plantar lesser toes; 4. Inter-digital space of toes; 5. Plantar great toe; 6. 5th metatarsal head; 7. 2nd to 4th metatarsal head; 8. 1st metatarsal head; 9. Lateral border of the foot, in-between head of the 5th metatarsal and heel; and 10. Plantar hind foot, weight-bearing area of the heel. |
The foot included for the study was examined thoroughly for deformities such as claw toes, hammer toes, high and low arch foot, prominent metatarsal heads and hallux rigidus/limitus. If any were present, the patient was excluded from the study.
Evaluation of footwear
A detailed interview was conducted of the type of footwear worn over the past 3–6 months including the quality of the straps/upper cover, inner sole and outer sole. A history of footwear use inside and outside the house and hours of use per day including the use or non-use of footwear at the time of the formation of the ulcer was collected. Using the algorithm for choosing footwear in diabetes,[8] each type was classified as appropriate or inappropriate based on the underlying foot pathology of each person with diabetes. A brief description of the algorithm is given below.
Each patient's foot was categorized into low, moderate and high risk for ulceration based on sensory and motor neuropathy, vasculopathy, presence of pressure skin lesions, and previous history of ulceration and foot deformities. The low-risk category were those with normal sensation, normal muscle strength, palpable pulses and no high-pressure skin lesions. Patients with low risk can wear footwear of any type with a back strap as an optional feature. Those with moderate risk for ulceration had loss of protective sensation, with/without intrinsic muscle paralysis, with/without mobile deformities such as low and high arch foot and, with/without high-pressure skin lesions. Patients in this category can wear microcellular rubber (MCR) insole with hard outsole and adjustable front and back straps. Patients at high risk for ulceration had loss of protective sensation, intrinsic muscle paralysis and fixed deformities such as rocker bottom foot due to Charcot osteoarthropathy, or severe scars in high-pressure areas. Such patients require custom-made footwear with/without braces. Only moderate risk patients without secondary foot deformities were enrolled in the study.
Statistical analysis
We estimated a sample size of 300 people with diabetes presuming a 25% prevalence of diabetic foot ulcers[10] with a 95% confidence interval and 80% power. Among the 4800 people with diabetes visiting our centre during the study period (April 2011 to March 2012), 345 people presented with FFU.
The statistical package of social sciences (SPSS Inc., Chicago, IL) was used for all analysis. A p value <0.05 was considered significant.
Results
Of the 301 patients who agreed to participate in the study, 267 had an FFU in one leg, 4 of whom had had a below knee amputation of their contralateral leg due to a foot ulcer before inclusion in the study. They had developed a foot ulcer in their contralateral leg for the first time. The remaining 34 had ulcers in both legs. Thus, data on 335 limbs were available for analysis.
Case-control study
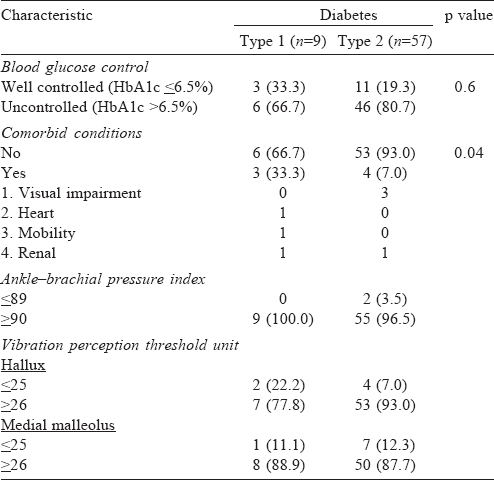
Demographic and clinical. The demographic characteristics of both patients and controls were comparable [Table - 1]. The study population's age ranged between 35 and 81 years. Disabling comorbid conditions were present in 7 patients (10%) and 12 controls (18%) and were not significantly different [Table - 2]. Diabetes was detected at the time of development of the foot ulcer in 5 patients (7.6%).
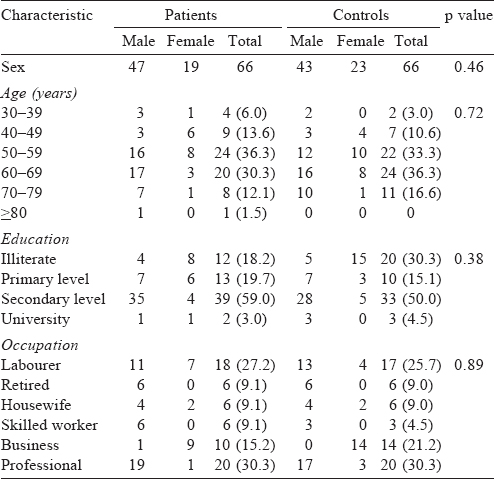
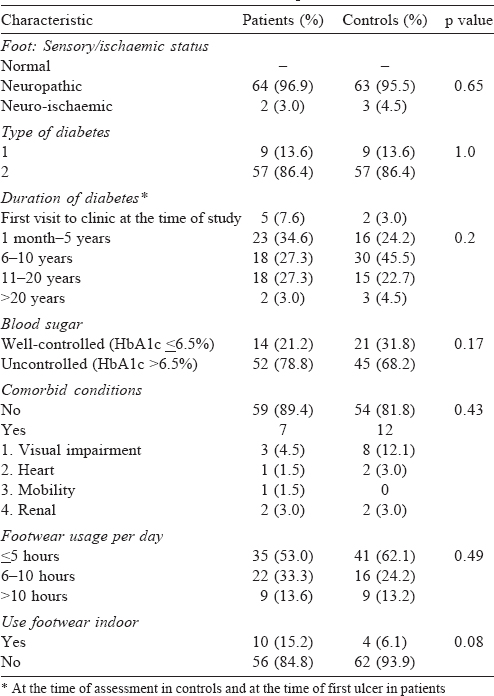
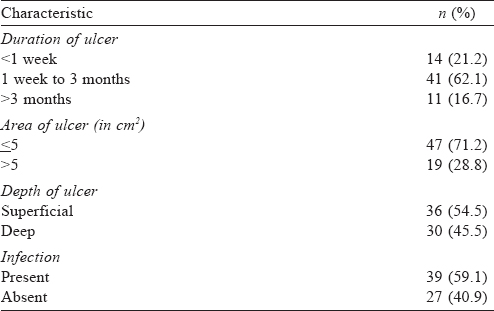
Characteristics of FFU and use of footwear. About one-fifth of patients reported to us for treatment within a week of developing their FFU. The surface area of the ulcer during their first visit was <5 cm2 area in 47 (71.2%) and superficial in 39 (59.1%) limbs. However, 39 (59.1%) foot ulcers were infected at the time of presentation [Table - 3]. There was no difference in footwear use in terms of hours and habit of using it indoors between patients and controls. None of the patients or controls had features only of ischaemia. They were either neuropathic or neuro-ischaemic (2 [3%] among patients and 3 [5%] among controls; [Table - 2]),.
Indices of types 1 and 2 diabetes. Vasculopathies were found only among people with type 2 diabetes. Loss of vibration perception threshold was high in both types of diabetes ranging from 77.9% to 93% [Table - 4]. People with type 1 diabetes with FFU had a higher prevalence of comorbid conditions than those with type 2 diabetes. Also the blood sugar levels in both types 1 and 2 diabetes were high at presentation.
Cross-sectional study
First foot ulcers. Of the 4800 people with diabetes, 345 (7.2%) had FFU. Among these 301 met the inclusion criteria, with footwear being the direct cause of the FFU in one-fifth of the 335 limbs studied; all of them had a unilateral ulcer [Table - 5]. Prolonged low pressure exerted by the footwear was the cause for two-thirds of the ulcers and the remaining one-third occurred due to high-pressure injury caused by a sharp foreign body penetrating through the soft outer sole of the footwear.
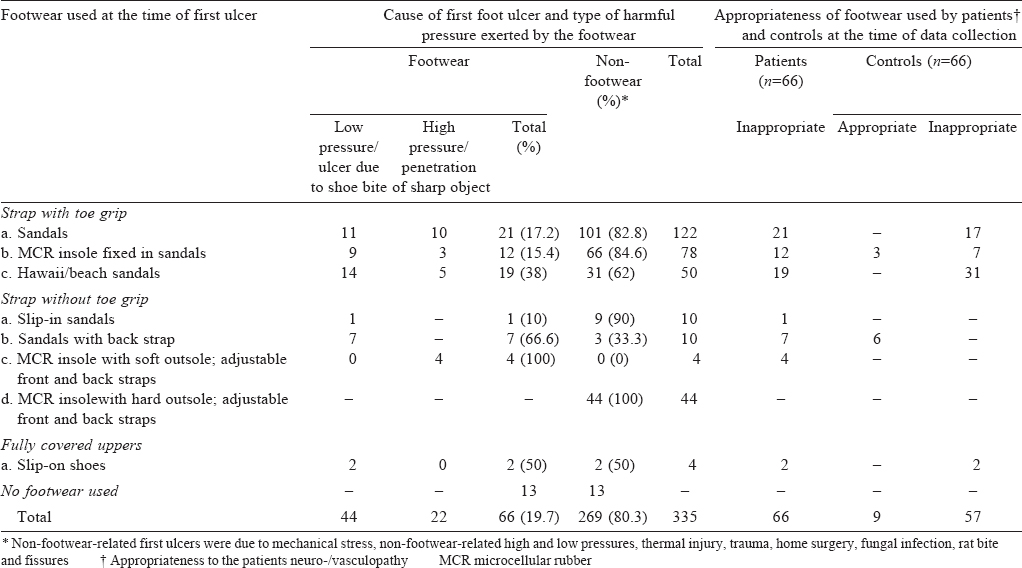
Role of footwear in the occurrence of FFU. Seven models of footwear [Figure - 2]: [Figure - 1]a to [Figure - 1]c, [Figure - 2]a to [Figure - 2]c and [Figure - 3]a were used by patients while the controls used five models [Figure - 2]: [Figure - 1]a to [Figure - 1]c, [Figure - 2]b and [Figure - 3]a. Inappropriate use of footwear was seen in 86.4% of non-FFU patients with neuro-/vasculopathy, and was 100% among those who developed FFU.
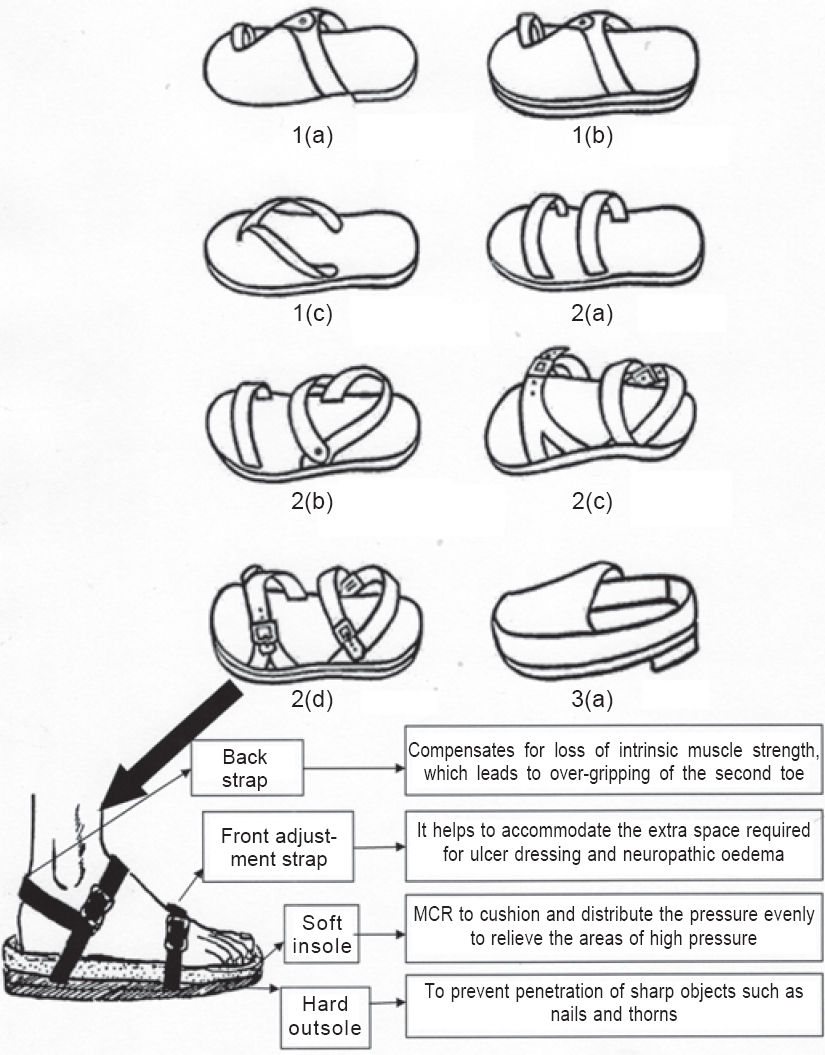 |
| Figure 2: Footwear models used by the study participants. The lowermost enlarged illustration is the ideal footwear for people with diabetes and neuro-/vasulopathy—1. Footwear with toegrip strap: a. sandals, b. Microcellular rubber (MCR) insole fixed in sandals, c. Hawaii/beach sandals; 2. Footwear without toe-grip strap: a. Slip-in sandals, b. Sandals with back strap, c. MCR insole with soft outsole, adjustable front and back straps, d. MCR insole with hard outsole, adjustable front and back straps; 3a. Fully covered uppers, slip-on shoes. |
 |
| Figure 3: A thorn penetrating a soft outer sole of the footwear caused an injury in a person with a neuropathic foot |
Role of components of footwear in FFU. The three components assessed were: (i) inner sole, (ii) outer sole, and (iii) shoe-uppers/ sandal straps.
Inner and outer soles. All inner and outer soles were made from either hard materials, soft materials or a combination. Hard inner soles were either leather or synthetic materials. The outer soles were either fitted to a soft or a hard inner sole, or both the outer and inner sole were made from the same soft material, as in Hawaii/beach sandals [Figure - 2]: [Figure - 1]c or the same hard material as in sandals [Figure - 2]: [Figure - 1]a.
One-third of footwear inj uries observed were due to penetration of sharp objects through the footwear, where its outer layer was not sufficiently hard [Figure - 3]. Only 13.6% of injuries were as a result of not using soft inner soles [Table - 6].
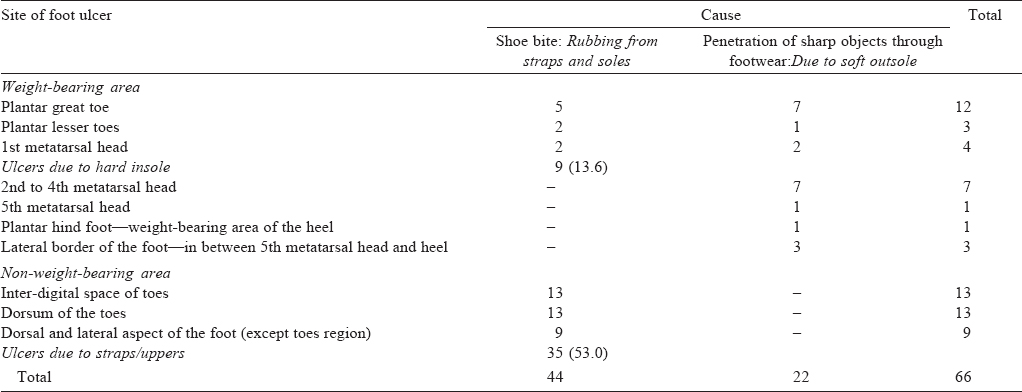
Straps. Just over half (53%) of the ulcers were formed on non-weight-bearing area caused by straps of the footwear [Table - 6]. Three different types of straps were used. These are described below:
- Footwear with toe grip. Three models of sandals were used by both the patients and controls and had a toe grip fitment in the first web space [Figure - 2]: [Figure - 1]a to [Figure - 1]c. These models were used by nearly 80% (52 of 66) of patients who developed FFU [Table - 5]. These three models were inappropriate for the patients, especially if they had loss of protective sensation combined with intrinsic muscle paralysis. They tend to exert pressure for longer duration over the toe grip and this can cause ulceration [Figure - 4]. If loss of protective sensation was present without intrinsic muscle paralysis, the use of sandals with a soft inner sole [Figure - 2]: [Figure - 1]b was found to be appropriate.
- Footwear without toe grip. Three types of sandals used by patients with FFU had straps without a toe grip fitment [Figure - 2] : [Figure - 2]a to [Figure - 2]c. Nearly one-fifth of those who developed an ulcer (12 of 66) used one of three such upper strap models without a toe grip fitment [Table - 3]. Of these, only one model was used by the controls [Figure - 2]: [Figure - 2]b.
- Slip-on shoes: In other instances slip-on shoes with fully covered uppers shown in [Figure - 2]: 3(a) were used by both patients and controls. This model too was inappropriate.
 |
| Figure 4: A plantar ulcer (common site) because of gripping the footwear's toe-grip strap tightly for a long time |
Acceptable footwear models
Among the seven models of footwear used by patients with FFU, none were acceptable, except the model with MCR insole, hard outsole, and adjustable front and back straps. The common footwear used by our patients had buckles of iron or steel [Figure - 2]d. This is considered ‘acceptable’ and not ‘appropriate’, as generally footwear with buckles is not recommended for people with diabetes. However, this was the most acceptable model that even a poor person could purchase in any footwear store. Among all controls who had diabetic neuropathy and/or neurovasculopathy but no FFUs, the above model and sandals with back strap [Figure - 2]b were appropriate.
Discussion
The cause of a diabetic foot ulcer is both complex and multifactorial. Multiple factors contribute to the pathogenesis of foot ulceration including peripheral neuropathy, foot deformity, peripheral vascular disease, foot oedema and calluses.[16] Any one of these factors is usually insufficient to cause an ulcer and it is usually a combination of factors which lead to ulceration.[17] We have shown that the use of inappropriate footwear in the neuropathic and/or neuro-ischaemic foot is an important cause of FFU in one-fifth of our study population. Thus, improper footwear is a major contributing factor to ulceration. The use of four types of inappropriate footwear was seen among controls who had neuro-/vasculopathy with no history of ulceration, but a high risk of developing future ulcers. Other studies from developed countries have also shown that approximately half of diabetes-related amputations are attributable to poorly fitting footwear causing foot ulcers.[18],[19]
Ulceration by upper straps with low-pressure shoe bite
A low pressure, defined as 1-5 pascals, over a long period of time can cause ischaemic necrotic ulceration.[20] We found that two-thirds of footwear-related ulcers were caused by low-pressure shoe bite either by straps/uppers (53%) or the hard inner sole ( 13. 6%) of the footwear [Table - 3]. A diabetic foot with neuropathy that suffers sustained impairment of blood supply due to footwear straps or hard inner soles could result in pressure necrosis and ulceration. A study examining diabetic foot disease in Europe found more ulcers on non-weight-bearing (52%) than on plantar surface of feet, perhaps due to improperly fitting straps/uppers on the shoe.[1] Our study corroborates this finding.
Normal intrinsic muscle function is required to grip the footwear between the first and second toes while walking. Patients with diabetic neuropathy tend to buy poorly fitting footwear to stimulate some sensory feedback, thus prevents slipping of footwear.[21]
We postulate that footwear straps could produce a low-pressure ulcer by one of two mechanisms: (i) people with neuropathic feet tend to use a tight-fitting non-adjustable strap to prevent footwear from slipping off. This is likely to produce a low-pressure ulcer on the dorsum of the foot due to neuropathic numbness. Such pressure and ulceration may become further aggravated if the patient has oedema; and/or (ii) both the toe-grip strap and the hard inner sole of footwear can cause low-pressure ulcers because patients with neuropathy tend to hold the toe-grip strap of sandals tightly in their first web space to prevent footwear slipping off. Such low pressure exerted on the web space and tip of the toes for a prolonged period, especially if the insole of the footwear is hard, results in ischaemic necrosis, particularly if vascular degeneration is present.[22] [Figure - 4] depicts a FFU caused by such a mechanism.
Toe-grip sandals are popular among the Indian population, as illustrated in this study with 52 of 66 of presenting FFU cases wearing this model.
Ulcers caused by penetrating injuries through the outer sole
High pressure, if >1000 pascals, can cause skin breakdown.[20] A soft outer sole was the second most common component to contribute to ulceration. In our study, a soft outer sole contributed to one-third of footwear-related ulcers. In a number of footwear models used by people with diabetes with and without ulceration, the same material (either soft or hard) was used to construct the inner and outer components of the footwear. For example, the Hawaii/beach sandals had the same soft consistency in both upper and lower rubber soles. Sharp objects such as nails and thorns could easily penetrate such a soft sole and cause injury by a foreign body to a neuropathic foot. An example of this is depicted in [Figure - 3], which shows that a thorn penetrated the soft outer sole causing an injury resulted in ulcer and infection. A harder outer sole may prevent such high-pressure injuries.
Soft inner sole to prevent FFUs
Characteristics of an ideal footwear for diabetic patients is available in the literature.[8] The lowermost illustration in [Figure - 2] diagrammatically shows the midsole which is a part of an ideal diabetic footwear. A midsole helps in providing stability to the feet. However, the more cushioned the midsole, the less stability to the feet. This can cause postural instability in patients with diabetic neuropathy.[23] On the other hand, a rigid midsole prevents footwear bending and gives a rocker effect to footwear. Rocker soles generally off load pressure from the anterior part of the foot and help prevent forefoot ulcer formation.[24] Clinics for people with diabetes emphasize the use of soft insoles to prevent ulcers. However, we found that a hard insole was associated with only 13.6% of ulcers in our patients. Almost all ulcers that occurred in patients using hard inner soles were in the forefoot region. Sun et al. reported that plantar tissues over the forefoot area tend to be stiffer in patients with diabetic neuropathy.[25] This can interfere with their natural function as shock absorbers during weight-bearing activities. This will reduce normal ability to dissipate abnormal plantar pressures on the plantar forefoot region, contributing to ulceration.
In summary, FFUs can probably be reduced in patients with neuro-/vasculopathy if they use a hard outer sole, soft inner sole and a midsole with adjustable front and back straps.
| 1. | Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K, et al. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe: Baseline results from the Eurodiale study. Diabetologia 2007;50:18-25. [Google Scholar] |
| 2. | Jaysinghe SA, Atukorala I, Gunethilleke B, Siriwardena V, Herath SC, De Abrew K. Is walking barefoot a risk factor for diabetic foot disease in developing countries? Rural Remote Health 2007;7:692. Available at www.rrh.org.au (accessed on 12 Nov 2014). [Google Scholar] |
| 3. | Shankhdhar K, Shankhdhar LK, Shankhdhar U. Diabetic foot problems in India: An overview and potential simple approaches in a developing country. C’urr Diab Rep 2008;8:452-7. [Google Scholar] |
| 4. | Pendsey S, Abbas ZG. The step-by-step program for reducing diabetic foot problems: A model for the developing world. Curr Diab Rep 2007;7:425-8. [Google Scholar] |
| 5. | Fryberg RG, Bailey LF, Matz A, Panthel LA, Ruesch G. Off loading properties of a rocker insole: A preliminary study. J Am Podiatric Med Assoc 2002;92:48-53. [Google Scholar] |
| 6. | Buschk S, Chantelau E. Effectiveness of a new brand of stock ‘diabetic’ shoes to protect against diabetic foot ulcer relapse: A prospective cohort study. Diabet Med 2003;20:665-9. [Google Scholar] |
| 7. | Litzelman DK, Marriott DJ, Vinicor F. The role of footwear in the prevention of foot lesions in patients with NIDDM. Conventional wisdom or evidence based practice. Diabetes care 1997;20:156-62. [Google Scholar] |
| 8. | John JA, Bobeena RC, Rajan P, Premkumar R. Therapeutic footwear. In: Thomas N, Jeyaraman K (eds). A practical guide to diabetes mellitus. 7th ed. New Delhi:Jaypee Brothers Medical Publishers; 2016:220-44. [Google Scholar] |
| 9. | Macfarlane RM, Jeffcoate WJ. Factors contributing to the presentation of diabetic foot ulcers. Diabet Med 1997;14:867-70. [Google Scholar] |
| 10. | Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA 2005;293:217-26. [Google Scholar] |
| 11. | Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, et al.; Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003;26:3160-7. [Google Scholar] |
| 12. | Little RR, Rohlfing CL, Sacks DB. The National Glycohemoglobin Standardization Program Steering Committee. Status of hemoglobin A1c measurement and goals for improvement: From chaos to order for improving diabetes care. Clin Chem 2011;57:205-14. [Google Scholar] |
| 13. | The Criteria Committee of the New York Heart Association. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9 th ed. Boston:Little, Brown and Co; 1994:253-6. [Google Scholar] |
| 14. | Schaper NC. Diabetic foot ulcer classification system for research purposes: A progress report on criteria for including patients in research studies. Diabetes/Metab Res Rev 2004;20 (Suppl 1):S90-S95. [Google Scholar] |
| 15. | Schaper NC, Andros G, Apelqvist J, Bakker K, Lammer J, Lepantalo M, et al. Specific guidelines for the diagnosis and treatment of peripheral arterial disease in a patient with diabetes and ulceration of the foot. DiabetesMetab Res Res 2012;28 (Suppl 1):236-7. [Google Scholar] |
| 16. | Lavery LA, Peters EJ, Armstrong DG. What are the most effective interventions in preventing diabetic foot ulcers? Int Wound J 2008;5:425-33. [Google Scholar] |
| 17. | Reiber GE, Vileikyte L, Boyko EJ, Del Aguila M, Smith DG, Lavery LA, et al. Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings. Diabetes Care 1999;22:157-62. [Google Scholar] |
| 18. | Crausaz FM, Clavel S, Lininger C, Albeanu A, Assal JP. Additional factors associated with plantar ulcers in diabetic neuropathy. Diabet Med 1988;5:771-5. [Google Scholar] |
| 19. | Pecoraro RE, Reiber GE, Burgers EM. Pathways to diabetic limb amputations: Basis for prevention. Diabetes care 1990;13:513-21. [Google Scholar] |
| 20. | Birke JA, Novick A, Hawkins ES, Patout C. A review of causes of foot ulceration in patients with diabetes mellitus. Am Acad Orthosis Prosthesis 1991;4:13-22. [Google Scholar] |
| 21. | Cavanagh PR. Therapeutic footwear for people with diabetes. Diabetes Metab Res Rev 2004;20 (Suppl 1):S51-S55. [Google Scholar] |
| 22. | Bevans JS. Biomechanics and plantar ulcers in diabetes. The Foot 1992;2:166-72. [Google Scholar] |
| 23. | Perry SD, Radtke A, Goodwin CR. Influence of footwear midsole material hardness on dynamic balance control during unexpected gait termination. Gait Posture 2007;25:94-8. [Google Scholar] |
| 24. | Brown D, Wertsch JJ, Harris GF, Klein J, Jannisse DJ. Effects of rocker soles on plantar pressures and lower extremity biomechanics. Arch Phy Med Rehabil 2004;85:81-6. [Google Scholar] |
| 25. | Sun JH, Cheng BK, Zheng YP, Huang YP, Leung JY, Cheing GL. Changes in the thickness and stiffness of plantar soft tissues in people with diabetic peripheral neuropathy. Arch PhysMedRehabil 2011;92:1484-9. [Google Scholar] |
Fulltext Views
10,428
PDF downloads
2,564




