Translate this page into:
Identifying core competency areas to assess communication skills among interns at a tertiary teaching hospital in southern India
2 Department of Microbiology, Government Medical College, Kozhikode, Kerala 673008, India
3 Department of Paediatrics, Government Medical College, Kozhikode, Kerala 673008, India
4 Department of Pharmacology, Government Medical College, Kozhikode, Kerala 673008, India
Corresponding Author:
Asma A Rahim
Department of Community Medicine, Government Medical College, Kozhikode, Kerala 673008
India
rahmaniyas@gmail.com
| How to cite this article: Rahim AA, Anitha P M, Govindaraj GM, Laila K V. Identifying core competency areas to assess communication skills among interns at a tertiary teaching hospital in southern India. Natl Med J India 2017;30:332-336 |
Abstract
Background. We aimed to develop a teaching–learning and evaluation programme on communication skills for interns. Core competency areas for focused communication skills training and assessment were identified to achieve the obective. We then assessed the identified competencies among interns using objective structured clinical examination (OSCE), before the start of internship.Methods. Five core areas for focused training and evaluation were identified on the basis of responses of practising physicians in local settings. OSCE stations were developed for evaluation based on the identified competency areas. A pre-test OSCE was administered to 30 interns.
Results. Five core areas selected for training and evaluation were: (i) communicating with a parent resistant to immunization; (ii) interacting with a patient who has psychosomatic complaints; (iii) explaining risks and procedures; (iv) breaking bad news; and (v) communicating with patients and bystanders in a casualty setting. Thirty of 160 interns were selected to participate in the OSCE before the training (pre-test). The lowest score was for breaking bad news. Scores indicated that explaining risks and procedures, communicating in a busy casualty setting and dealing with psychosomatic complaints were areas that required extensive training and practice.
Conclusions. We were able to identify core competency areas for focused training and evaluation of communication skills suited to the local context and used OSCE to evaluate the skills before the start of internship.
Introduction
Communication skills play a key role in healthcare and are a core aspect of clinical competence. In traditional medical teaching this skill is acquired through experience. However, with experience one tends to adopt certain behaviours and adhere to one's own model of communication without realizing the drawbacks of the ‘traditional models’.[1] Communication skills are not taught in most Indian undergraduate or postgraduate medical courses, and it is considered that in a busy outpatient department, such skills may not be optimally applied.[2] Though it is simple to incorporate sessions on communication skills in the teaching schedule, hardly any attempt is made to do so.[3] Evidence from western countries suggests that communication skills can be taught during undergraduate and postgraduate courses, are learnt, but are easily forgotten, if not practised regularly. The teaching method should be experiential since it has been shown that instructional methods do not give the desired results. ‘The contents of communication skills courses should primarily be problem defining’.[4]
The training in communication skills needs to start at the undergraduate level and continued till internship to ensure competency of a doctor. The curriculum on communication skills focuses on ‘breaking bad news’ while neglecting more crucial and commonly encountered issues related to patient compliance and education in the ambulatory setting. The Medical Council of India's Vision 2015 document emphasizes the need to include communication skills in the medical curriculum.[5] If this is to become a requirement in Indian medical schools, a context-sensitive curriculum needs to be developed. Patients in Indian outpatient clinics often come from varied backgrounds, with differences in the spoken language, culture, education and social context. A doctor is therefore required to individualize the information depending on the background of the patient.[6]
A systematic approach needs to be adopted for developing an effective curriculum for communication skills. This can be done by designing a teaching–learning methodology with emphasis on the content and process of communication skills training relevant to the local context using a mix of experiential, problem-based and didactic methods—the three complementary approaches to maximize learning.[1],[7],[8]
It is well known that assessment drives learning and ‘assessment is the curriculum as far as the students are concerned’.[9],[10] Objective structured clinical examination (OSCE) was introduced in medicine in the late 1970s as a tool for ensuring standardization and psychometric stability in the assessment of clinical skills. This method has been found to add to ward-based teaching. Students require more opportunities to practise in a controlled environment, before being exposed to a clinical setting.[11],[12]
A review of the literature shows that OSCE has increasingly become an acceptable format to assess objective clinical competencies in medical education, as well as to examine some isolated skills and providing immediate feedback.[12],[13] Professional actors have been trained to play the role of patients and this practice is common in assessments of health professionals.[14]
A systematic review of 109 published articles by Hauer et al. suggests that students learn behaviour change consultation through active, realistic career and feedback systems within authentic clinical work settings.[15] Yedidia et al. used a 10-station OSCE with standardized patients (SPs) to quantify improvement or deterioration in communication skills after a group of students participated in formal teaching sessions that focused on these skills.[16]
Since the publication of the Calgary Cambridge guidelines in 1998 and developments over the past two decades, many organizations at all levels of medical education and across a wide range of specialties have adopted the guidelines to underpin their communication skills programmes. Institutions throughout the world have used this guide as a primary teaching resource, an assessment tool or research instrument.[1]
Traditional models practised by many at present focus entirely on diagnosis and management plans that are doctor- centred and paternalistic. Though long lists of communication skills models with emphasis on ‘Evidence-based communication’ are being used in clinical practice, we selected the Calgary Cambridge model for this study since it recognizes content skills separately from the process and perceptive skills. We aimed at assessing the process and perceptive skills of residents through observations during communication.
A communication skills teaching programme was introduced for interns with no prior training during their undergraduate years, at the start of the internship. Since the interns had no formal training we had to find out to what extent they had imbibed the scientific principles of communication in traditional teaching. Evaluation was done using OSCE stations with checklists based on the Calgary Cambridge guidelines modified to the local setting with simulated patient encounters based on identified difficult-to-communicate scenarios.
Methods
Identifying core competency areas to assess communication skills of interns relevant to the local context was the first step. We also assessed the communication skills of interns using OSCE stations on the basis of scenarios identified before a structured training in communication skills.
Identifying core competency areas
We administered a semi-structured questionnaire to 45 doctors working in peripheral healthcare settings (district hospital, community health centres and primary health centres). Along with feedback on their perception on the need for training in communication skills, they were also asked to make a list of difficult-to-communicate situations in routine doctor–patient interactions in our local healthcare setting. Responses were grouped under different themes. Based on this, five major areas were identified for training and evaluation.
Developing OSCE stations based on identified scenarios An expert panel of faculty from the medical education unit was consulted and OSCE was decided as a tool to evaluate skills before the start of training.
Each station theme was thoroughly discussed and a clinical scenario created towards an OSCE [Table - 1] by following the widely accepted basic framework of communication skills, ‘Calgary Cambridge guidelines’. Checklists were developed for each scenario to address possible cultural bias and cultural specificities that may need to be accounted for in applying it in different contexts. These were revised according to suggestions relevant to the clinical and cultural context. Items in each checklist were examined rigorously. All faculty members agreed upon the final checklist items, thereby ensuring good face validity.
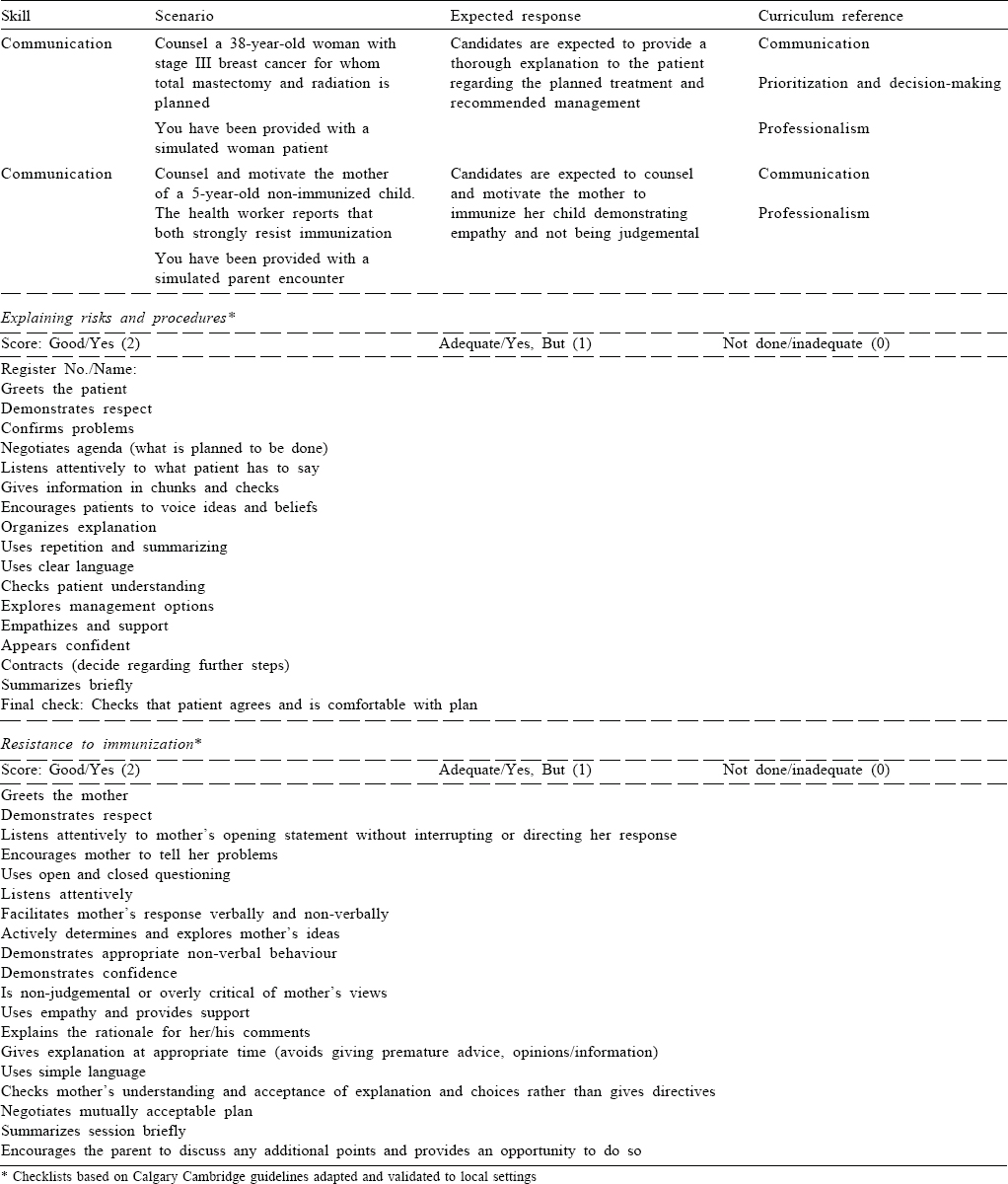
Rating scales consisted of scores assigned to each item based on performance consisting of Good/yes (2), Adequate/ yes but (1), and Not done/inadequate (0) for each item. ‘Simulated patients’ were trained on enacting the clinical situation under supervision of the expert panel. Senior residents from five clinical departments (e.g. physical medicine, surgery, paediatrics, community medicine and medicine) acted as simulated patients. Examiners were 10 experts from clinical departments who were well versed with the checklist. Each station was allotted 10 minutes.
Each OSCE station was pilot-tested (for construct validity) using examinees who were junior residents from clinical departments and had undergone training in communication skills at their induction. Ten experts watched the residents' performance at each station. Internal consistency of the checklist items and inter-rater reliability of the OSCE stations were assessed.
Assessing interns' communication skills Of the 160 interns enrolled for the communication skills training for pre-test assessment of communication skills, 30 were selected by systematic random sampling. Before the training, these 30 interns were assessed using OSCE and their scores were noted.
Data analysis
Data were compiled and analysed using SPSS Version 16. Pretest OSCE scores were calculated.
Results
The five core areas selected for OSCE station development based on practising physicians' responses were: (i) communicating with a parent resistant to immunization; (ii) interacting with a patient who has psychosomatic complaints; (iii) explaining risks and procedures; (iv) breaking bad news; and (v) communicating with patients and bystanders in a casualty setting. The majority of practising physicians suggested that breaking bad news was a communication skill that needed to be focused on.
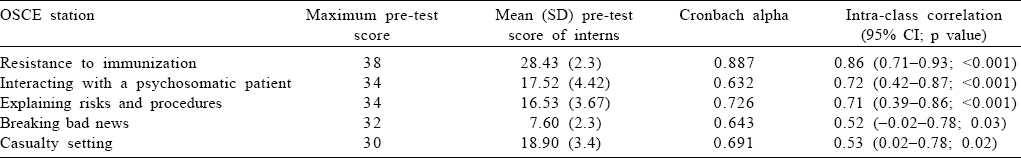
Based on the core competency areas, five OSCE stations were developed. All the OSCE stations had a Cronbach alpha of >0.5 in relation to the checklist items. Inter-rater reliability of each station was over 0.5 on calculating the intra-class correlation (ICC) scores.
The 30 interns then participated in the pre-test OSCE. The lowest score was for breaking bad news [Table - 2]. Scores indicated that explaining about risks and procedures, communicating in a casualty setting and interacting with patients who had psychosomatic complaints were areas that needed emphasis as well as extensive practice.
Discussion
The success of physician–patient relationships is predicated on effective communication. A common scenario, irrespective of the cultural context, is when a physician must deliver bad news to a patient or family, deal with patients who are angry or seeking drugs, or handle patients who do not adhere to treatment due to financial concerns.[17],[18] Over the years, practitioners have attempted to discover more successful and empathic responses to address the needs of the ‘difficult’ patient. Recently, it has been recognized and generally accepted that the ‘difficulty’ in caring for patients frequently arises out of an interactional process between the patient and the caregiver. This understanding requires self-awareness among practitioners as well as reflection about motivations and responses to difficult clinical encounters.[19],[20],[21] Based on this principle, we identified five core areas towards improving communication of interns. Though one may criticize that skills developed in a western setting are unsuitable to our cultural context, we realized in the process of constructing the checklists that we do practise most skills in our day-to-day practice and almost all skills are essential in any culture. Our experience of using the Calgary Cambridge guidelines is that key core skills in patient-centred medicine need to be modified slightly to work effectively within our social context. One of the objectives of our study was to identify challenging situations in communication that doctors face daily in the Indian cultural context. Though the argument would be that the context and content of communication changes in different situations, the process skills remain the same and need to be applied with sensitivity and consideration in different circumstances.
In most OSCEs, communication skills are assessed as an ‘addon’ to history-taking stations, rather than in stations designed to assess communication skills in the broadest sense. Several studies have shown the feasibility of creating communication OSCE stations with acceptable reliability including difficult cases that address communication skills beyond history-taking. Physician–patient communication including empathy, which is a highly complex process, can be tested by OSCE as noted in several studies.[22],[23],[24]
Measurement errors have been identified for case specificity, candidate–simulated patient interaction and case–candidate interaction.[25],[26] Inter-rater reliability of each station was >0.5 on calculating the ICC scores. Cronbachs alpha of >0.5 in relation to OSCE checklists indicated good internal consistency of the items, emphasizing the applicability of the Calgary Cambridge checklist items to the local context.
The performance scores of interns were lowest for breaking bad news probably due to absence of formal training in this aspect. Complex communication can sometimes lead to serious miscommunication such as patient misunderstanding the prognosis of the illness or mode of care.[27],[28],[29] Poor communication may also thwart the goal of understanding patient expectations of treatment or involving the patient in treatment planning. This requires rigorous systematic training. Higher scores in the station on resistance to immunization counselling may be because the paediatrics department uses OSCEs for assessment as part of their formative and summative evaluation, which underlines that assessment drives learning.[30]
We did not use global rating scales in our assessment and our sample size was small. Also a larger number of stations should be used in further studies.
This exercise has helped us identify the key areas to be focused in communication skills training to interns in our setting, as well as identify the appropriate teaching–learning and evaluation methods to achieve the objectives. Our study is in agreement with other researchers that OSCE stations on communication can be created with acceptable reliability.[22],[31],[32]
Acknowledgements
We thank Thomas V. Chacko, Director, PSG-FAIMER South Asia Regional Institute for the support and assistance provided. This was part of the curriculum innovation project done by the first author as a requirement of the FAIMER Fellowship programme.
We are grateful to Dr C. Ravindran, Principal and Chairperson of the Medical Education Unit, Government Medical College, Kozhikode for supporting us in this project.
Conflicts of interest. None
| 1. | Kurtz S, Silverman J, Draper J. Teaching and learning communication skills in medicine. 2nd ed. Oxford:Radcliffe Medical Press; 2005. [Google Scholar] |
| 2. | Chatterjee S, Choudhury N. Medical communication skills training in the Indian setting: Need of the hour. Asian J Transfus Sci 2011 ;5:8-10. [Google Scholar] |
| 3. | Rajashree K. Training programs in communication skills for health care professionals and volunteers. Indian J Palliative Care 2011;17:12-13. [Google Scholar] |
| 4. | Aspegren K. BEME Guide No. 2: Teaching and learning communication skills in medicine—a review with quality grading of articles. Med Teach 1999;21: 563-70. [Google Scholar] |
| 5. | Vision 2015. Available at www.mciindia.org/tools/announcement/MCI_booklet.pdf (accessed on 20 Dec 2015). [Google Scholar] |
| 6. | Stewart MA, McWhinney IR, Buck CW. The doctor/patient relationship and its effect upon outcome. J R Coll Gen Pract 1979;29:77-81. [Google Scholar] |
| 7. | Pocinki AG. Dialogue: A core clinical skill. Ann Intern Med 1998;129:253-4. [Google Scholar] |
| 8. | Biggs J, Tang C. Teaching for quality learning at university. Maidenhead: McGraw-Hill/Society for Research into Higher Education/Open University Press; 2011. [Google Scholar] |
| 9. | Marton F, Hounsell D, Entwistle N. The experience of learning. Edinburgh: Scottish Academic Press; 1984. [Google Scholar] |
| 10. | Harden R, Gleeson F. Assessment of clinical competence using an objective structured clinical examination (OSCE). Med Educ 1979;13:39-54. [Google Scholar] |
| 11. | Robb KV, Rothman A. The assessment of history-taking and physical examination skills in general internal medicine residents using a checklist. Ann R Coll Physicians Surgeons Canada 1985;20:45-8. [Google Scholar] |
| 12. | Pierre RB, Wierenga A, Barton M, Thame K, Branday JM, Christie CD. Student self-assessment in a paediatric objective structured clinical examination. West Indian Med J 2005;54:144-8. [Google Scholar] |
| 13. | Keely E, Myers K, Dojeiji S. Can written communication skills be tested in an objective structured clinical examination format? Acad Med 2002;77:82-6. [Google Scholar] |
| 14. | Bokken L, Linssen T, Scherpbier A, van der Vleuten C, Rethans JJ. Feedback by simulated patients in undergraduate medical education: A systematic review of the literature. Med Educ 2009;43:202-10. doi: 10.1111/j.1365-2923.2008.03268.x. [Google Scholar] |
| 15. | Hauer KE, Carney PA, Chang A, Satterfield J. Behavior change counseling curricula for medical trainees: A systematic review. Acad Med 2012;87:956-68. doi: 10.1097/ACM.0b013e31825837be. [Google Scholar] |
| 16. | Yedidia MJ, Gillespie CC, Kachur E, Schwartz MD, Ockene J, Chepaitis AE, et al Effect of communications training on medical student performance. JAMA 2003; 290:1157-65. [Google Scholar] |
| 17. | Leahy M. Communication strategies for difficult physician–patient interactions. Am Association Ortho Surgeries 2015:29. [Google Scholar] |
| 18. | Batchelor J, Freeman MS. Spectrum: The clinician and the “difficult” patient. SDJ Med 2001;54:453-6. [Google Scholar] |
| 19. | Breuner CC, Moreno MA. Approaches to the difficult patient/parent encounter. Pediatrics 2011;127:163-9. doi: 10.1542/peds.2010-0072. [Google Scholar] |
| 20. | Brown JB, Weston WW, Stewart MA. Patient-centred interviewing. Part II: Finding common ground. Can Fam Physician 1989;35:153-7. [Google Scholar] |
| 21. | Hodges B, Turnbull J, Cohen R, Bienenstock A, Norman G. Evaluating communication skills in the OSCE format: Reliability and generalizability. Med Educ 1996;30:38-43. [Google Scholar] |
| 22. | Schwartzman E, Hsu DI, Law AV, Chung EP. Assessment of patient communication skills during OSCE: Examining effectiveness of a training program in minimizing inter-grader variability. Patient Educ Couns 2011;83:472-7. [Google Scholar] |
| 23. | Fischbeck S, Mauch M, Leschnik E, Beutel ME, Laubach W. [Assessment of communication skills with an OSCE among first year medical students]. Psychother Psychosom Med Psychol 2011;61:465-71. doi: 10.1055/s-0031-1291277. [Google Scholar] |
| 24. | Guiton G, Hodgson CS, Delandshere G, Wilkerson L. Communication skills in standardized-patient assessment of final-year medical students: A psychometric clinical examination (OSCE) stations for communication skills training study. Adv Health Sci Educ Theory Pract 2004;9:179-87. [Google Scholar] |
| 25. | Regehr G, Freeman R, Robb A, Missiha N, Heisey R. OSCE performance evaluations made by standardized patients: Comparing checklist and global rating scores. Acad Med 1999;74 (10 Suppl):S135-S137. [Google Scholar] |
| 26. | Hodges B, Turnbull J, Cohen R, Bienenstock A, Norman G. Evaluating communication skills in the OSCE format: Reliability and generalizability. Med Educ 1996;30:38-43. [Google Scholar] |
| 27. | Lind SE, DelVecchio Good MJ, Seidel S, Csordas T, Good BJ. Telling the diagnosis of cancer. J Clin Oncol 1989;7:583-9. [Google Scholar] |
| 28. | Eidinger RN, Schapira DV. Cancer patients' insight into their treatment, prognosis, and unconventional therapies. Cancer 1984;53:2736-40. [Google Scholar] |
| 29. | Mackillop WJ, Stewart WE, Ginsburg AD, Stewart SS. Cancer patients' perceptions of their disease and its treatment. Br J Cancer 1988;58:355-8. [Google Scholar] |
| 30. | Wood T. Assessment not only drives learning, it may also help learning. Med Educ 2009;43:5-6. doi: 10.1111/j.1365-2923.2008.03237.x. [Google Scholar] |
| 31. | Collins LG, Schrimmer A, Diamond J, Burke J. Evaluating verbal and non-verbal communication skills, in an ethnogeriatric OSCE. Patient Educ Couns 2011 ;83: 158-62. doi: 10.1016/j.pec.2010.05.012. [Google Scholar] |
| 32. | Khan A, Qureshý R, Acemo$$ölu H, Shabi-ul-Hassan S. Comparison of assessment scores of candidates for communication skills in an OSCE, by examiners, candidates and simulated patients. Creative Educ 2012;3:931-6. [Google Scholar] |
Fulltext Views
1,388
PDF downloads
789




