Translate this page into:
Occupational health profile of workers employed in the manufacturing sector of India
Corresponding Author:
Shivali Suri
Department of Community Medicine, Lady Hardinge Medical College and Associated Hospitals, New Delhi
India
shivalisuridr@yahoo.co.in
| How to cite this article: Suri S, Das R. Occupational health profile of workers employed in the manufacturing sector of India . Natl Med J India 2016;29:277-281 |
Abstract
Background. The occupational health scenario of workers engaged in the manufacturing sector in India deserves attention for their safety and increasing productivity. We reviewed the status of the manufacturing sector, identified hazards faced by workers, and assessed the existing legislations and healthcare delivery mechanisms.Methods. From October 2014 to March 2015, we did a literature review by manual search of pre-identified journals, general electronic search, electronic search of dedicated websites/databases and personal communication with experts of occupational health.
Results. An estimated 115 million workers are engaged in the manufacturing sector, though the Labour Bureau takes into account only one-tenth of them who work in factories registered with the government. Most reports do not mention the human capital employed neither their quality of life, nor occupational health services available. The incidence of accidents were documented till 2011, and industry-wise break up of data is not available. Occupational hazards reported include hypertension, stress, liver disease, diabetes, tuberculosis, eye/ hearing problems, cancers, etc. We found no studies for manufacturing industries in glass, tobacco, computer and allied products, etc. The incidence of accidents is decreasing but the proportion of fatalities is increasing. Multiple legislations exist which cover occupational health, but most of these are old and have not been amended adequately to reflect the present situation. There is a shortage of manpower and occupational health statistics for dealing with surveillance, prevention and regulation in this sector.
Conclusion. There is an urgent need of a modern occupational health legislation and an effective machinery to enforce it, preferably through intersectoral coordination between the Employees' State Insurance Corporation, factories and state governments. Occupational health should be integrated with the general health services.
Introduction
The manufacturing sector contributed 15% to the gross domestic product (GDP) of India in 2014. The launch of ′Make in India′ and ′Skill India′ initiatives envisages establishment of high-class manufacturing facilities and enhancement of skills. [1] While these would contribute to increased output of the manufacturing sector, the human capital should also be looked after by improving the occupational health scenario.
The Constitution of India through its Directive Principles aims to secure the health and strength of its employees, provide just and humane working conditions and facilitate the establishment and provisioning of occupational health services. [2] Yet the occupational health scenario in the manufacturing sector in India leaves much to be desired. This could be attributed to the multitude of new industries and new units being added every year. [3],[4],[5] More importantly, if the health of workers who comprise about 10% of our population could be ensured, it would improve our GDP and contribute to achieving the goal of Health for All. [6]
We, therefore, reviewed the occupational health scenario of workers engaged in manufacturing in India. The specific objectives of our review were to: (i) present an overview of the manufacturing sector; (ii) identify industries facing greater health hazards and estimate the burden of the problem; and (iii) enlist existing legislations and briefly assess the delivery mechanisms for occupational health and safety.
Methods
A comprehensive literature review was conducted between October 2014 and March 2015; and published as well as unpublished papers were considered. A manual search of pre-identified journals, a general electronic search, specific search of dedicated websites/databases and personal communications with experts in the field were done.
An electronic search was done on PubMed, PLOS, Medline Plus and Index Copernicus using ′free-text′ and MESH keywords. The keywords searched were: occupational health, manufacturing sector, India, occupational diseases and workers in India. A manual search of journals, unpublished work, and personal communications also tracked citations by checking reference lists. A manual search was also done of the journals, books and other documents at the National Medical Library, and the library of Lady Hardinge Medical College, New Delhi. A ′search log′ was maintained to record the details of how the search was done including the list of journals, websites and databases. Cross-references of articles were also followed up, institutional websites visited and some of the authors were contacted in person, telephonically or by email. Experimental, quasi-experimental or observational studies pertaining to occupational health hazards of workers engaged in the manufacturing sector of India were considered for inclusion.
We prepared a database of all available studies, and assessed the ′value′ of each study by using a standardized form with explicit inclusion and exclusion criteria. Studies meeting a high level of agreement between two reviewers (Cohen′s kappa, 24 κ: 0.92) were included in the review. Data were extracted into a standardized data collection form that had been pilot tested on a random sample of studies.
Microsoft Access 2010 was used to store the information and for reference management in addition to manual notes. The journals searched included Indian Journal of Community Medicine, Indian Journal of Public Health, Indian Journal of Occupational Health, International Journal of Epidemiology and International Journal of Occupational Health and Safety. Grey literature included for the review primarily consisted of reports of the Ministry of Labour and Employment, Government of India; National Institute of Occupational Health, Ahmedabad; Indian Council of Medical Research, New Delhi; Central Labour Institute, Mumbai; and All India Institute of Hygiene and Public Health, Kolkata.
Results
Our search yielded 7865 articles of which 182 pertained to India but only 39 of these related to the manufacturing sector. These were included for more detailed analysis and review.
Overview of the manufacturing sector
The manufacturing sector in India is not only vast but also complex. A large number of industries and occupations are involved. Prominent among these are textile and apparels, leather, paper, chemicals and petrochemicals, rubber, glass, metals, pharmaceuticals, tobacco, food and beverages, computers and electricals, motor vehicles and machinery, mining (coal, ores, petrol and gas, etc.), etc. Different industries, owing to their using a diversified range of raw materials and processes, predispose workers to a variety of risks of differing severity. In the 270 294 manufacturing units, 4 303 000 workers were employed with men comprising 86.5% of the workforce. The proportions contributed by individual manufacturing industries were: textiles (12.5%), food products (12.3%), metals and their products (10.1%), chemicals (7.9%), metal products (7.7%), motor vehicles (5.7%) and rubber (4.2%). [4],[7]
Health hazards
We found 20 studies that reported the health hazards of workers engaged in manufacturing. Not all manufacturing industries have been studied/reported upon. The broad groups of industries that have been studied include chemical industry, metal and allied, plastic and rubber, leather, asbestos, textiles and allied, automobile and allied, and ship building. [Table - 1] lists the predominant type of health hazards in these manufacturing sectors. [8],[9],[10],[11],[12],[13],[14],[15],[16],[17],[18],[19],[20],[21],[22],[23],[24],[25],[26],[27]

Incidence of occupational injuries/accidents
The Directorate General of Factory Advice Service (DGFASLI) classifies accidents into fatal and total (i.e. fatal as well as non-fatal). The incidence of both categories has declined over the years from 65.59 per 1000 persons in 1980 to 2.41 in 2006 and 0.90 in 2011, but the proportion of fatal injuries has increased from 0.2% in 1980 to 5.4% in 2006 and 10% in 2011 ([Figure - 1]). [3],[4]
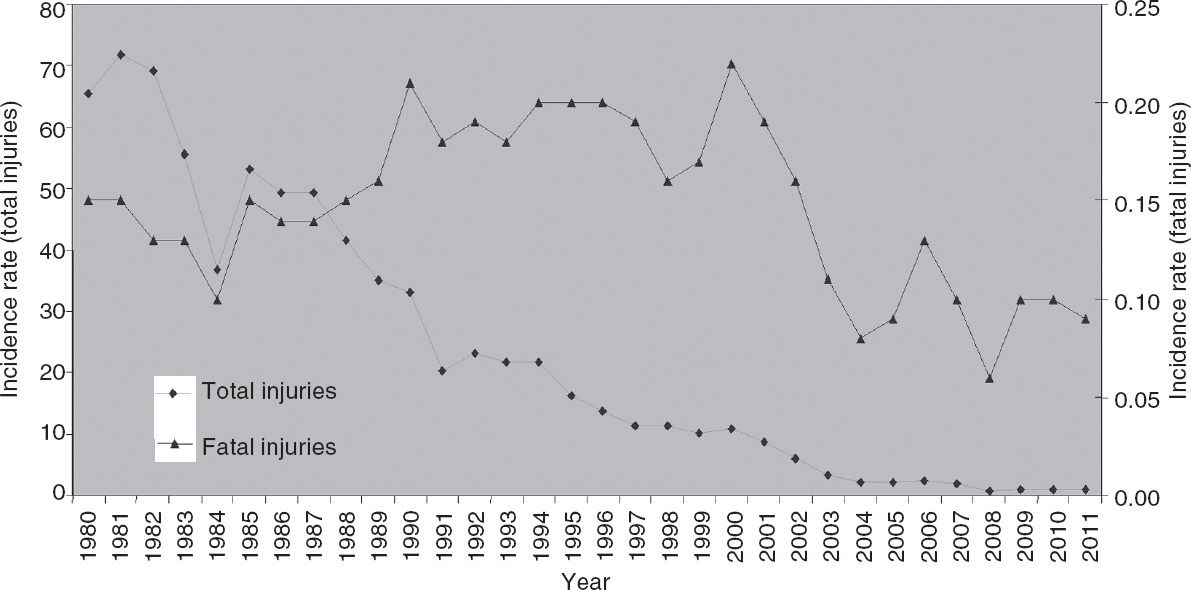 |
| Figure 1. Incidence of industrial injuries in the manufacturing sector (1980– 2011).3,4 The rates are per 1000 employees per year |
The highest incidence has been reported in the manufacture of transport equipment (5.42/1000/year), with intermediate rates in the textile and related industries (3.57/1000/year), machinery manufacturing (3.26/1000/year), metal and alloy industries (3.16/1000/year) ([Figure - 2]). It was 2.64 to 2.79/1000/year among workers involved in the manufacture of metal products, electricity and gas. The incidence rates were lower (1.63 to 1.97/1000/year) in industries involved in the manufacture of paper, chemicals and non-metallic mineral products. [7]
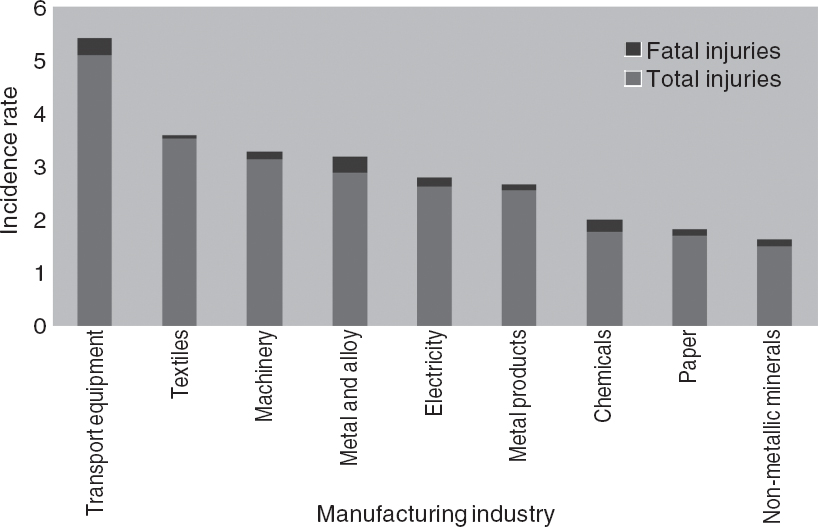 |
| Figure 2. Incidence of injuries in different manufacturing industries.7 The rates are per 1000 employees per year |
Notifiable occupational diseases
Twenty-nine conditions are notifiable according to the 3rd Schedule of the Factories Act, 1948. These include occupational lung diseases, poisonings, contact dermatitis, occupational cancers and noise-induced hearing loss. Few studies have reported statistics on notifiable diseases. Silicosis was the commonest offender with 38%-54.5% prevalence in slate pencil and precious/semi-precious stone manufacturing. The next commonest was byssinosis with a prevalence of 30%-48.8% in textile and jute manufacturing. The prevalence of asbestosis has been reported to be 3%-9% among workers involved in its manufacture. [3]
Vulnerable groups involved in manufacturing
Women and children employed in manufacturing are likely to face even greater adverse impact from occupational exposures because neither the tasks they perform nor the equipment they use are designed keeping in mind their build and physiology. [28] This is in addition to the lower wages, lesser control over decision-making and the risk of sexual harassment. [29],[30] Tiwari and Saha reported that children engaged in the manufacturing sector work for 6 hours or more per day. The work environment is also poorly ventilated and illuminated, unhygienic and often has respirable dust making it unsafe. [31] Workers from the informal sector form another important vulnerable group but in spite of their higher occupational as well as non-occupational morbidity, healthcare and social security for them is meagre, if not completely absent. [29]
Existing laws/programmes and their implementation
There are 44 labour-related laws/programmes in India for the welfare of workers; of these, 10 have provisions related to occupational health and safety. These are: the Factories Act 1948, the Employees′ State Insurance (ESI) Act 1948, the Child Labour (Prohibition and Regulation) Act 1986, the Maternity Benefit Act 1961, the Workmen′s Compensation Act 1923, the Contract Labour (Regulation and Abolition) Act 1970, the Unorganized Workers′ Social Security Act 2008, the Bonded Labour System (Abolition) Act 1976, the Fatal Accidents Act 1855, and the Personal Injuries (Compensation Insurance) Act 1963. [32] Only two of these, the Factories Act and the ESI Act are of direct relevance and have reasonable coverage of the workers.
The Factories Act covers the conduct of multidisciplinary surveys in industry, training of factory inspectors, etc. and is executed by DGFASLI under the Ministry of Labour. [33] The ESI Act, on the other hand, is an integrated social security scheme for workers and their dependants to cover for sickness, death or disablement, and maternity. It is administered through the ESI dispensaries and hospitals. [34]
Assessing the occupational safety in manufacturing units is the responsibility of DGFASLI, and is done by a team of inspectors and medical officers. Sharma et al. found that for 11.2 million manufacturing workers in 250 000 industries, there should be approximately 7000 factory medical officers and 2000 safety officers. [35] However, the sanctioned strength of DGFASLI is only 1400 safety officers, 1154 factory inspectors and 27 medical inspectors. Besides these, a few more posts are provided by various state governments, details of which we were not able to obtain. There is high non-incumbency and in 2009 even in the sanctioned posts the vacancy rate was 35.6% for factory inspectors, 46.2% for specialist inspectors of factories, 55.5% for medical inspectors and 33.3% for chemical and other inspectors. [29],[30] The required versus in-position manpower and infrastructure for catering to occupational health and safety for the year 2009 is shown in [Figure - 3]. [7]
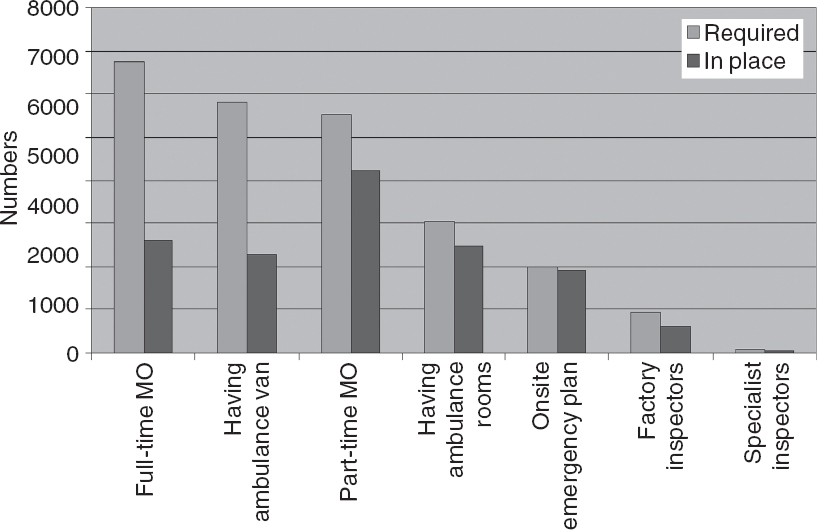 |
| Figure 3. Existing manpower and infrastructure for catering to occupational health and safety for the year 20097 MO medical officer |
The figure of 10.1 million as the manpower employed in the manufacturing sector is an underestimation by the Labour Bureau since only 10% of India′s total workforce is employed in the formal sector. [4] In 2011-12, the National Sample Survey Organization (NSSO) estimated that 115 million people were employed in the manufacturing sector. [36] For planning and implementation of occupational health services to be realistic and inclusive, it is pertinent that the non-organized sector should also be included. Even if complete enumeration is not feasible at least a representative sampling covering all regions of the country must be done. Even though human capital is the single most important resource for any industry, including the manufacturing sector, reports generated by most agencies focus only on the quantum of production, contribution to GDP, etc. with no mention of the estimated human capital involved, the quality of life the workers lead nor the quantum and quality of occupational health services available to them. [4],[36],[37] This trend needs to be corrected.
Of the thousands of papers published each year and tens of thousands over the past decade, only 39 papers reported on the occupational health and safety of workers from the manufacturing sector in India. We could not find any studies documenting health hazards arising from manufacturing industries such as glass, computers and allied products, food and beverages, tobacco, etc. Occupational health hazards of workers employed in these industries are not negligible. Even for those sectors for which studies were available, the number of workers studied was very small. Occupational health specialists in particular and the medical research community in general should generate more research data in this field.
While the annual incidence of injuries and accidents are available for India as a whole, the break-up according to the type of manufacturing industry is not available. [3] Availability of accurate figures through routine reporting and registering systems from few representative and identified manufacturing clusters needs to be developed on the lines of the Sample Registration System of NSSO under the Registrar General of India.
Most occupational health and safety legislations in force in India are about half a century old and while much has happened on the manufacturing front in these five decades, necessary amendments in our legislations and programmes have not been done. The ESI Corporation, which aims to deliver comprehensive occupational health services to all workers, including those in the manufacturing sector, should not only have a strong preventive component, but should also be integrated with the general health services. Both these components are lacking in the present scenario. [33],[34]
A manpower crunch is the single most crucial occupational health and safety issue at present. The sanctioned posts are far fewer than necessary, and even many sanctioned posts are lying vacant. This has a negative impact on surveillance, preventive and regulatory functions. [7] The 6809 full-time and part-time insurance medical officers available for the estimated 115 million manufacturing workforce yield a doctor-population ratio of 1:16 912 which is highly inadequate. Besides allocation of financial support, new posts should be created, and the ESI should be integrated with the general health services.
The information provided here pertains mostly to the organized sector, which constitutes only about 10% of the manufacturing sector; however, the completeness of reporting even for the organized sector cannot be ascertained. Hardly any information was found on children employed in hazardous manufacturing. Data regarding occupational injuries/accidents are based on government reports, which are available only up to 2011.
To sum up, a new and comprehensive occupational health legislation is necessary for a strong preventive care component and a robust delivery mechanism integrated with the general healthcare services. Such a programme should have adequate financial allocation, an effective hazard elimination component and an awareness programme for wide dissemination. [38],[39] These efforts would not only safeguard the health and interests of all workers, including those from the manufacturing sector, but also help achieve the goals of Health for All, Make in India and Skill India.
Conclusion
India has a large and complex manufacturing sector but with meagre occupational health services. Few studies have reported on occupational health hazards of workers engaged in manufacturing, and not all types of industries have been studied. While a gradual decrease in the incidence of accidents has been reported, the proportion of fatalities has increased. Though 44 legislations and programmes related to occupational health and safety of workers are in place, many of their provisions are left un-implemented. There is a major shortfall in manpower needed to assess and address occupational health and safety of workers. The vast majority of workers from the manufacturing sector are outside the purview of even the existing legislations/programmes. If India is to make its presence felt in manufacturing in a sustainable way, it can ill-afford to be negligent of the occupational health and safety issues of workers engaged in manufacturing.
| 1. | Make in India 2014. Department of Industrial Policy and Promotion, Ministry of Commerce and Industry, Government of India, 2014. Available at http://dipp.nic.in/English/Investor/makeinindia.aspx (accessed on 2 Dec 2016). [Google Scholar] |
| 2. | National Policy on Safety, Health and Environment at work place. Ministry of Labour and Employment, Government of India. Available at http://dgfasli.nic.in/npolicy/OSH-Policy.pdf (accessed on 16 Aug 2015). [Google Scholar] |
| 3. | Report of the working group on Occupational safety and health for the Twelfth Five-year Plan (2012-17). Ministry of Labour and Employment, Government of India, 2011. [Google Scholar] |
| 4. | Indian Labour Statistics, 2012 and 2013. Shimla:Labour Bureau, Ministry of Labour and Employment, Government of India; 2014. [Google Scholar] |
| 5. | Kulkarni GK. Implementation of occupational health legislation at work place, issues and concerns. Indian J Occup Environ Med 2008; 12: 51-2. [Google Scholar] |
| 6. | Annual Report 2014-15. Ministry of Labour and Employment, Government of India. Available at http://labour.nic.in/reportspublications/annual-report-2015-16 (accessed on 7 Aug 2015). [Google Scholar] |
| 7. | Standard Reference note 2010. Directorate General Factory Advice Service and Labour Institutes, Ministry of Labour and Employment, Government of India. Available at www.dgfasli.nic.in/std_ref/std_ref_2010.pdf (assessed on 7 Jul 2015). [Google Scholar] |
| 8. | Ambreen K, Khan FH, Bhadauria S, Kumar S. Genotoxicity and oxidative stress in chromium-exposed tannery workers in North India. Toxicol Ind Health 2014; 30: 405-14. [Google Scholar] |
| 9. | Khan FH, Ambreen K, Fatima G, Kumar S. Assessment of health risks with reference to oxidative stress and DNA damage in chromium exposed population. Sci Total Environ 2012; 430: 68-74. [Google Scholar] |
| 10. | Febriana SA, Jungbauer F, Soebono H, Coenraads PJ. Inventory of the chemicals and the exposure of the workers' skin to these at two leather factories in Indonesia. Int Arch Occup Environ Health 2012; 85: 517-26. Int Arch Occup Environ Health 2012; 85: 517-26.'>[Google Scholar] |
| 11. | Syed M, Saleem T, Shuja-ur-Rehman, Iqbal MA, Javed F, Khan MB, et al. Effects of leather industry on health and recommendations for improving the situation in Pakistan. Arch Environ Occup Health 2010; 65: 163-72. [Google Scholar] |
| 12. | Susheela AK, Mondal NK, Singh A. Exposure to fluoride in smelter workers in a primary aluminum industry in India. Int J Occup Environ Med 2013; 4: 61-72. [Google Scholar] |
| 13. | Murlidhar V, Kanhere V. Asbestosis in an asbestos composite mill at Mumbai: A prevalence study. Environ Health 2005; 4: 24. [Google Scholar] |
| 14. | Sam KG, Andrade HH, Pradhan L, Pradhan A, Sones SJ, Rao PG, et al. Effectiveness of an educational program to promote pesticide safety among pesticide handlers of South India. Int Arch Occup Environ Health 2008; 81: 787-95. [Google Scholar] |
| 15. | Singh S, Kumar V, Thakur S, Banerjee BD, Chandna S, Rautela RS, et al. DNA damage and cholinesterase activity in occupational workers exposed to pesticides. Environ Toxicol Pharmacol 2011; 31: 278-85. [Google Scholar] |
| 16. | Manjunatha R, Kiran D, Thankappan KR. Sickness absenteeism, morbidity and workplace injuries among iron and steel workers--a cross sectional study from Karnataka, Southern India. Australas Med J 2011; 4: 144-7. [Google Scholar] |
| 17. | Chauhan A, Anand T, Kishore J, Danielsen TE, Ingle GK. Occupational hazard exposure and general health profile of welders in rural Delhi. Indian J Occup Environ Med 2014; 18: 21-6. [Google Scholar] |
| 18. | Dongre NN, Suryakar AN, Patil AJ, Hundekari IA, Devarnavadagi BB. Biochemical effects of lead exposure on battery manufacture workers with reference to blood pressure, calcium metabolism and bone mineral density. Indian J Clin Biochem 2013; 28: 65-70. [Google Scholar] |
| 19. | Mazumdar I, Goswami K. Chronic exposure to lead: A cause of oxidative stress and altered liver function in plastic industry workers in Kolkata, India. Indian J Clin Biochem 2014; 29: 89�-92. [Google Scholar] |
| 20. | Sati PC, Khaliq F, Vaney N, Ahmed T, Tripathi AK, Banerjee BD. Pulmonary function and oxidative stress in workers exposed to styrene in plastic factory: Occupational hazards in styrene-exposed plastic factory workers. Hum Exp Toxicol 2011; 30: 1743-50. [Google Scholar] |
| 21. | Gemitha G, Sudha S. Assessment of genotoxicity among rubber industry workers occupationally exposed to toxic agents using micronucleus assay. Iran J Cancer Prev 2013; 6: 73-7. [Google Scholar] |
| 22. | Singh MB, Fotedar R, Lakshminarayana J. Occupational morbidities and their association with nutrition and environmental factors among textile workers of desert areas of Rajasthan, India. J Occup Health 2005; 47: 371-7. [Google Scholar] |
| 23. | Das PK, Shukla KP, Ory FG. An occupational health programme for adults and children in the carpet weaving industry, Mirzapur, India: A case study in the informal sector. Soc Sci Med 1992; 35: 1293-302. [Google Scholar] |
| 24. | Frank AL, Joshi TK. The global spread of asbestos. Ann Glob Health 2014; 80: 257-62. [Google Scholar] |
| 25. | Murlidhar V, Kanhere V. Asbestosis in an asbestos composite mill at Mumbai: A prevalence study. Environ Health 2005; 4: 24. [Google Scholar] |
| 26. | Ayyappan R, Sankar S, Rajkumar P, Balakrishnan K. Work-related heat stress concerns in automotive industries: A case study from Chennai, India. Glob Health Action 2009;2. [Google Scholar] |
| 27. | Lokhande VR. Health profile of workers in a ship building and repair industry. Indian J Occup Environ Med 2014; 18: 89-94. [Google Scholar] |
| 28. | Perera FP, Li TY, Lin C, Tang D, Gilbert SG, Kang SK, et al. Current needs and future directions of occupational safety and health in a globalized world. Neurotoxicology 2012; 33: 805-9. [Google Scholar] |
| 29. | Mandal AK. Strategies and policies deteriorate occupational health situation in India: A review based on social determinant framework. Indian J Occup Environ Med 2009; 13: 113-20. [Google Scholar] |
| 30. | Saiyed HN, Tiwari RR. Occupational health research in India. Ind Health 2004; 42: 141-8. [Google Scholar] |
| 31. | Tiwari RR, Saha A. Morbidity profile of child labor at gem polishing units of Jaipur, India. Int J Occup Environ Med 2014; 5: 125-9. [Google Scholar] |
| 32. | Annual Report 2012-13. Ministry of Labour and Employment, Government of India. Available at http://labour.gov.in/sites/default/files/ANNUAL%20REPORT%202012-2013_0.pdf (accessed on 7 Aug 2015) [Google Scholar] |
| 33. | The Factories Act,1948. Ministry of Labour and Employment, Government of India. Available at http://labour.gov.in/upload/uploadfiles/files/TheFactoriesAct1948.pdf (accessed on 15 Aug 2015). [Google Scholar] |
| 34. | The Employees' State Insurance Act, 1948. Ministry of Labour and Employment, Government of India. Available at http://esic.nic.in/backend/images/esic_act_file/f91b795b3a6ec0e381b824d4805f1d58.pdf (accessed on 15 Aug 2015). [Google Scholar] |
| 35. | Sharma K, Zodpey SP, Tiwari RR. Need and supply gap in occupational health manpower in India. Toxicol Ind Health 2013; 29: 483-9. [Google Scholar] |
| 36. | National Sample Survey Office (NSSO). Employment and unemployment situation in India (July 2011-June 2012), Vol. 554 of 68th round. National Sample Survey Office, Ministry of Statistics and Programme Implementation, Government of India, January 2014. [Google Scholar] |
| 37. | Annual Report 2013-14. New Delhi: Ministry of Chemical and Petrochemicals, Government of India. Available at http://chemicals.nic.in/sites/default/files/english%20annual%20report%20new%20%20file%201-84.pdf (accessed on 17 Dec 2015). [Google Scholar] |
| 38. | World Health Organization. Report of the meeting 'Universal health coverage for workers', 66th Session of the World Health Assembly, 22 May 2013. Geneva, Switzerland:WHO; 2013. [Google Scholar] |
| 39. | World Health Organization. WHO Global Plan of Action on Workers' Health (2008-2017): Baseline for implementation. Geneva:WHO; 2013. Geneva:WHO; 2013.'>[Google Scholar] |
Fulltext Views
7,344
PDF downloads
2,245




