Translate this page into:
Pattern and profile of children using substances in India: Insights and recommendations
2 National Commission for Protection of Child Rights (NCPCR), India and Working Group on Substance Abuse among Children, New Delhi, India
3 Society for Promotion of Youth and Masses (SPYM), Vasant Kunj, New Delhi, India
Corresponding Author:
Anju Dhawan
Department of Psychiatry, National Drug Dependence Treatment Centre, All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110029
India
anjudh@hotmail.com
| How to cite this article: Dhawan A, Pattanayak RD, Chopra A, Tikoo V K, Kumar R. Pattern and profile of children using substances in India: Insights and recommendations. Natl Med J India 2017;30:224-229 |
Abstract
India has one of the largest proportion of children and adolescents in the world, but the threat posed by child substance use remains under-researched. Only recently a large study, the first of its kind in India, was carried out with a sample of nearly 4000 children using substances (school-going, out-of-school as well as street children) across more than a hundred cities/towns. We discuss (i) the existing knowledge on the prevalence of child substance abuse in India; (ii) perspectives and insights gained from the recent nation-wide study on its pattern and profile; and (iii) recommendations for substance use prevention and treatment among children in the Indian context. A multipronged approach involving all stakeholders is required to address the issues of prevention and treatment.
Introduction
Substance use among children and adolescents is a public health concern in several parts of the world.[1] Onset of substance abuse during the formative years interferes with academic, social and life skills development, and warrants both primary and secondary prevention.[2] Globally, India has one of the highest proportions of children and adolescents (aged <18 years: 45% of the population; 5–19 years: 35.3% of the population).[3],[4] In spite of a serious threat posed by child substance use and presence of a large proportion of the young, substance use among children has remained grossly under-researched in India, limited to sporadic studies at a local or regional level. Substance use among youth is uniquely associated with an increased risk of psychiatric disorders, e.g. depressive disorders, anxiety disorders, attention deficit hyperactivity disorder and conduct disorders. The relationship between mental and substance use disorders in youth seems to be bi-directional. Early onset is also associated with higher comorbid conditions and more chronic course and poorer outcome.[1],[2] Further, behavioural addictions, e.g. internet gaming disorder, are also increasing in this age group as reported from western settings.
A recent large study on the pattern, profile and correlates of child substance use is the first of its kind in India with a sample of nearly 4000 school-going, out-of-school as well as street children across over 100 cities and towns in various states.[5]
We discuss (i) the existing knowledge on prevalence of child substance use in India; (ii) perspectives on pattern and profile of child substance use gained from the recent nation-wide study; and (iii) recommendations for substance use prevention and treatment among children in the Indian context.
Young Population in India: Sociodemographic Profile
Children aged between 10 and 19 years constitute 22.8% of the population (243 million approximately) and those aged between 5 and 9 years constitute 12.5% of the population.[3],[4] The ratio of female per 1000 male adolescents is 882. Nearly 65%–70% of children are enrolled for primary school. Attrition in the education system is huge with 30% drop-out rates in classes I to V, increasing to 50% by class X. The formal education system has little to offer to the drop-outs and out-of-school adolescents. Out-of-school boys often join the unskilled workforce. Nearly 9% of children in urban areas and 13% in rural areas perform paid or unpaid work.[3],[4],[6]
Prevalence of Substance Use Among Indian Children
Earlier, substance use was considered as a problem associated mainly with street children but is now increasingly being seen across various subpopulations of children (i.e. school-going students and out-of-school children living at home). Further, anecdotal reports suggest a gradual increase in substance use among the younger population, across all socioeconomic groups, from cities to small towns and rural areas, with multiple substance use also being documented. Several cultural and regional factors play a part, e.g. tobacco is used as a dentrifice in many parts of India.
In India, no countrywide or large survey has focused on prevalence of substance use in children and adolescents. Available studies have small-to-medium samples, mostly conducted at a single setting or at a local or regional level.
Nationwide Studies
The only large, national household survey on prevalence and pattern of substance use in males (12–60 years) was done in 2001, which incorporated some information on prevalence among males in the 12–18 years age group (n=8587; current use: 3% for cannabis and 0.1% for opioid use).[7] The pattern was surprisingly similar to that of the 19–30 years age group. As part of this, a rapid assessment survey was also done at 14 sites, which found that nearly three-fourths of substance users had initiated their first substance use before completing 20 years of age.
Another nationwide survey of various health and family welfare indices in a representative household sample across India was the National Family Health Survey 2005–06 (NFHS-3).[8] Of the boys aged 15–19 years (n=13.099), 28.6% reported tobacco use and 11% reported alcohol use. Countrywide findings are not yet available for the adolescent subgroup from the more recent NFHS-4 (2015–16) survey.
School surveys
A systematic review of 15 such epidemiological studies published between 1991 and 2007 on Indian high-school students (classes VI to XII) found the median prevalence of ‘ever tobacco use’ to be 18% (interquartile range [IQR]: 9.4%–53.9%).[9] Some of the school surveys have examined tobacco and other substance use.[10],[11],[12],[13],[14],[15]
Studies on street children
An estimated 18 million children live and work on streets in India. Use of substances appear to be particularly high in this vulnerable population, with Indian studies reporting that 40%–70% of street children use substances.[16] Inhalant use has been found to be especially common among street children, in addition to tobacco, alcohol and cannabis.[17] Poverty, urbanization, breakdown of families and domestic violence are the most immediate causes of this growing phenomenon. There is a close relationship between child labour and substance use disorders. Substance use may be even more common in the marginalized populations such as trafficked or abused children.
Treatment-Seeking and Clinical Profile in Indian Specialty Settings
Most individuals start their substance use during adolescence, but treatment is usually sought after a few years when health or other psychosocial complications begin to emerge. The data on treatment- seekers from the Drug Abuse Monitoring System suggest that most persons who sought treatment at the drug dependence treatment centres across India initiated use during adolescence (9%–10% at <15 years of age and 25%–32% during 16–20 years of age). However, only 5% of treatment-seekers are actually adolescents.[7] Some reasons for low treatment-seeking in adolescents could be low motivation, perceived stigma attached to receiving treatment or lack of specialized adolescent treatment programmes, or even mere lack of awareness of facilities available.
The pattern of substance use in treatment-seeking adolescents in clinical settings appears to differ from that in the community.[18],[19],[20] Treatment-seeking child/adolescent sample is largely represented by inhalants, opioids and cannabis users (and not by tobacco or alcohol use as seen more often in the community). The majority are school drop-outs and from the lower socioeconomic status. Duration of inhalant use ranges from as low as 1 month to several years.[19] About one-fifth of treatment-seekers indulged in high-risk behaviour such as having multiple sexual partners.[20] The early onset of substance use is often associated with comorbid psychiatric or behavioural psychopathology, including hyperactivity/ inattention or conduct symptoms, which may make this age group more vulnerable to engage in high-risk behaviours. There is also a greater likelihood of later development of non-communicable and lifestyle diseases among early-onset substance users.
Gaps in Knowledge: Need to Document Pattern of Child Substance Use in the Indian Context
Overall, there was insufficient data on the profile of drug using children/adolescents and pattern and correlates of drug use in India. A need was increasingly felt for a nationwide study on child substance use in view of following gaps in existing knowledge:
- Substance use was undoubtedly high among street children, but was also found in the school as well as community surveys. There was a need to document substance use pattern and profile among children across various settings in the community.
- There was also a need to document the differences, if any, in the patterns of substance use (licit and illicit) across school- going, out-of-school and street children.
- There were likely to be regional variations in the prevalence and pattern of substance use.
- There was a need to document its presence in such cities and towns where the problem was often under-reported or dismissed as a ‘big-city’ phenomenon.
- There was a need to assess the psychological factors as well as the family and peers.
- Treatment-seeking behaviour and access to treatment also needed to be studied.
Assessment of Pattern and Profile of Children Using Substance a Nationwide Study
The study was planned by the National Commission for Prevention of Child Rights (NCPCR, Ministry for Women and Child, Government of India, in collaboration and with technical support from the National Drug Dependence and Treatment Centre, Department of Psychiatry, All India Institute of Medical Sciences, New Delhi).[5]
Children were selected, after assent/written guardian consent, using a combination of random and convenience sampling strategy and were included if they were aged ≤18 years and had used at least one substance (besides tobacco) in the past year. They were assessed by trained interviewers (graduate/postgraduate with field experience) using a 95-item questionnaire (English and Hindi, translated into eight local languages).
Data was collected through 117 NGOs (working in substance abuse or street children) across India selected in unison with the National Institute of Social Defence (NISD) and Federation of Indian Non-Governmental Organizations (NGOs) in Drug Abuse Prevention (FINGODAP) using a purposive sampling framework. Each NGO was considered as a study site, with a target sample of 30 children per site (with an estimated sample of 4000). Further details are available from the report at www.ncpcr.gov.in/view_f1le.php?f1d=17.[5]
Insights and observations from the study
- The first observation is that, in a relatively short time, without much difficulty, a big sample of children using substances could be collected (approximately 30 per site; <1 month to 3 months maximum).
- Though lack of data leads to a denial of the problem among Indian policy-makers, the study reveals that drug use exists in children in all regions, cities and smaller towns across all states.
- That the problem of substance use among children is not confined to metropolitan areas as is often perceived.
- The sample is fairly representative as it includes children from all regions (north, south, east, west and north-east) of the country, with a total of 29 states/union territories, and more than 100 cities and towns, giving some information on regional variations.
- The study enhances the understanding of progression of drug use in the Indian context, since it covers children till 18 years of age, while no lower age cut-off was kept. The youngest child in the sample was 5 years of age. The study provides information across all age groups of childhood and adolescence, especially on pattern and progression of use from early years till onset of adulthood.
- Girls constituted about 4.3% of the total sample, which has remained a hidden population. This study adds substantially to the little existing information on the girl child using substances in India.
- Little was known about the children who are ‘out-of-school and living at home’. It was not known whether their pattern of substance use is similar or dissimilar to the school-going children. Reaching out to this subgroup is another important aspect of the study, which can help in planning preventive and treatment services.
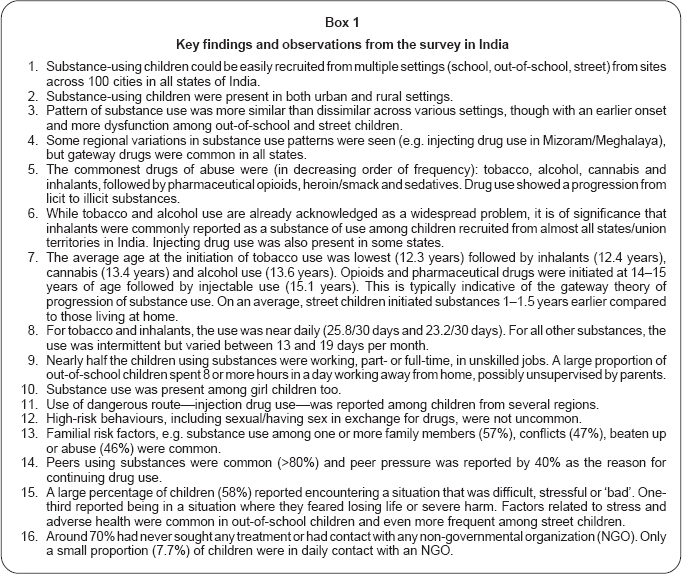
The key findings of the study are summarized in [Box 1]. This study cannot give an estimate of prevalence of substance use among children but gives useful information on the pattern and correlates of substance use. Certain limitations are acknowledged and the following methodological considerations may be kept in mind while interpreting the results: the sampling was done by snow-balling and other such techniques, technically limiting the generalizability of the findings. However, an effort was made to represent almost all states of India. As the sample was recruited mostly by NGOs working with substance users and street children, it may have represented the severe end of the spectrum. Though the survey questionnaire was translated into multiple languages with due precautions to ensure accuracy and context, the backtranslations could not be done. The study does not emphasize on the presence or absence of a dependence syndrome. Rather, it focuses on factors and complications related to or pattern of substance use. Further, inclusion of a diagnostic exercise/ instrument may have posed time constraints and burden in terms of more intensive training of the lay interviewers.
The girl sample was recruited from a few states; a large number of sites either did not send any data for girl users or had recruited <5 girls per site. Therefore, the findings from girl substance users have only a limited generalizability as they are likely to represent more severe users. On the other hand, it may be deduced that girls using substances continue to remain a largely hidden population, which is difficult to reach. The monitoring exercise was largely qualitative.
Available treatment services in India
Specialized drug treatment services for children or adolescents are confined to a few centres. In many areas these centres are not even functional. Only 122 drug de-addiction centres are run by the Ministry of Health and Family Welfare and 438 treatment-cum- rehabilitation and counselling centres are supported by the Ministry of Social Justice and Empowerment (MSJE).[21] Many of these centres lack infrastructure, staff and are not optimally functional. Even in areas where such services are available, treatment- seeking by child substance users is poor probably due to lack of motivation, perceived stigma or lack of understanding about the nature of substance use disorders. There is a need to raise community awareness for substance use among children and efforts made to facilitate treatment-seeking in a younger population.
Prevention and Treatment of Child Substance Use
The way forward in the Indian context
The problem of substance use among children needs to be addressed from multiple perspectives. The key ministries to be involved in a joint effort to prevent and treat substance use among children are the ministries of Social Justice and Empowerment, Health, Women and Child Development, Human Resource Development, Youth Affairs and Sports, Labour and Employment, and the Department of AIDS Control. The need for effective coordination between the different ministries cannot be over-emphasized for dealing with the problem of child substance use.
Recommendations
Prevention-related
- The study highlights the urgent need for national programmes addressing prevention and treatment of substance use among children in India. The preventive issues can be integrated in the existing programmes. For example, the preventive aspects of substance use are included in the Rashtriya Kishor Swasthya Karyakram or National Adolescent Health Policy launched in 2014 by the Ministry of Health and Family Welfare for adolescents aged 10–19 years.[22] The National Policy for Drug Demand Reduction, 2014 states that the preventive programme needs to focus on children, both in and outside educational institutions.[23] The high-risk groups such as commercial sex workers, the mobile population such as tourists and truck drivers, the children of alcoholics and drug addicts, children of HIV-affected parents, street children, prisoners and school drop-outs, should be specifically addressed. While prevention is a welcome step, provision of treatment services and reducing barriers to treatment among adolescent drug users also need to be prioritized.
- Prevention programmes must be designed to target multiple settings (school, community, street) and multiple risk factors particularly vulnerable children such as working children, out- of-school children, etc.
- Preventive efforts must target reduction in supply. Appropriate action should be taken by the relevant departments (viz. excise department for tobacco and alcohol control, Narcotic Control Bureau for illicit substances, Drug Controller General of India for pharmaceutical drugs). The ban on availability of tobacco and alcohol near schools and residential areas should be strongly enforced. It is worth mentioning that correction fluid (used as an inhalant) has been banned for sale since 2012 via a Gazette notification by the Central Government. Another recent phenomenon is the growing use of e-cigarettes among children and adolescents. They have the potential to lead to initiation of smoking forms of tobacco as well as other substances among the young population. The government must take a stand on these newer nicotine delivery systems, which are controversial and have not been proven to be safe in the long term. Similarly, rave parties with increasing use of synthetic drugs, e.g. ecstasy, lysergic acid diethylamide (LSD), etc. is a growing problem as indicated by anecdotal reports from metropolitan cities. The preventive efforts and policy framework must be comprehensive enough to include the traditional as well as newer forms of substances in youth. Prevention programmes must focus on the initiation of tobacco, alcohol, cannabis and inhalants (gateway drugs). Since the usual age of start of tobacco is about 12 years, the interventions must be directed towards younger age groups. The cannabis legalization debate in the international forums will have an influence on our vulnerable youth and India-specific policy issues. Prevention programmes in schools should focus on providing life skills education and teach methods to handle stress as well as peer pressure as a universal intervention, besides creating awareness of knowledge about harm. Life skill programmes should be developed/adapted and evaluated in the cultural context for substance use prevention and then widely disseminated. Conflicting findings from some studies show that the interventions focusing only on substance use aspects may not be effective and at times, may arouse curiosity and experimentation. Rather focus should be on development of life-skills and other primordial prevention.
- School-going children using substances should have access to professional counselling in the school setting. The Ministry/ Departments of Human Resource Development must provide at least one full-time trained psychologist in schools. Training of school counsellors to identify and manage children at risk needs to be imparted as has been done in Delhi. School counsellors should reach out to school-going children with risk factors in the family, substance using peers and history of stressful events.
- Educating teachers may be a welcome intervention for schoolchildren—with a focus not only on substance use but also on other behaviours such as conduct problems—as it is unlikely that even in the near future all schools will have counsellors.
- Efforts to reduce the rates of school drop-outs should continue, including by making school environments more child- and education-friendly. At the same time, vocational training centres and safe places should be available for out-of-school children, especially as two-thirds of out-of-school children were working part-/full-time. These vocational training centres could be the sites for interventions using life skills-based education and other strategies. Counselling services for children should be available in such places through trained professional counsellors.
- Prevention programmes must target the risk factors in the families, and parenting education should be available in schools, vocational training centres and communities.
- Secondary prevention—early detection and preventing progression-is another important aspect to be utilized in the context of child-onset substance use. Interventions should also focus on early, intermittent users so that they do not progress to daily use or the use of other illicit substances. Involvement of the community at Panchayat levels, Gram sabha/Mohalla sabha in raising awareness on the implicit hazards of substance use by children and its implications on the development of the child as a positive and productive member of society. We may need to gear up to control the technology addictions/internet gaming, etc. among the younger population (for a small but emerging group of users).
Treatment-related
- There is a need for availability and better access of specialized treatment services for children substance users. These services should be available in government hospitals; NGOs funded by the Ministry of Social Justice and also by NGOs that provide services to street children.
- General practitioners and paediatricians need to be appropriately sensitized to deal with this problem.
- Treatment programmes must try to involve the families and address their issues.
- In the study, more than two-thirds of children had never sought any help for substance use problems and were not in contact with any NGO working in their area, which points to the need to address treatment barriers, beginning with service provisions.
- Rehabilitation efforts focusing on skill building and vocational training should be provided by NGOs.
- Juvenile homes and children homes under the Ministry of Women and Child Welfare should have service provision for substance using children.
- The Targeted Interventions (TI) NGOs run by the Department of AIDS Control (DAC; earlier known as NACO), presently do not provide the entire range of services for adolescent intravenous drug users (IDUs). For example, needle syringe exchange programme is offered only to adults, and the same is true for harm reduction interventions for those involved in sex work due to ethical/legal concerns. However, buprenorphine substitution can now be considered for IDUs below 18 years of age, as per the 2014 revised guidelines.[24] Similarly, there is a need for appropriate, diverse range of services to sub-sets of younger IDUs, whose presence cannot be overlooked anymore in India.
- Prevention of harm/risks occurring as a consequence of drug use is another area to target in children using substances. This would include greater awareness about harm minimization with regards to risky behaviours such as drunken driving, unprotected sexual relationships under influence of the substance, etc.
Policy-related and service development
- There is a need to sensitize state governments and key stakeholders about the problem of child substance use in India so that appropriate policies and action plans can be formulated. The problem has usually been minimized in administrative circles to be a ‘big-city phenomenon’ only, an observation not supported by this nationwide study.
- Prevalence studies in a representative sample, size estimation of substance using children should be done in specific high- risk areas to be able to plan effective services and coverage. Appropriate budgetary allocations need to be made to deal with child substance use, for large-scale preventive interventions as well as for development of specialized services.
- Integration with other central/state programmes for adolescents: Information, awareness and preventive interventions directed at child/adolescent substance use must be integrated as far as possible with other programmes aimed at adolescent health in India (reproductive health, education, mental health, etc.). For example, the National Youth Policy (Ministry of Youth Affairs and Sports, Government of India, 2014)[25] stresses on the need for education, skills development, sports and healthy recreational activities and promotion of social values in youth, which may be protective factors for substance use. The National Adolescent Health Policy focuses on five key areas: nutrition, mental health, sexual and reproductive health, injuries and violence and substance misuse. Many of these key areas are related to substance abuse either as a risk factor (e.g. mental health issues) or as a consequence (e.g. injuries and violence).
- The cannabis legalization debate in the international forums may have influence on our vulnerable youth. We need to have our own policy with consensus among experts, literature support and other India-specific factors.
- Training manpower and capacity building can be enhanced through short-term training, long-term training and skill-based workshops, etc. to succeed in our prevention and treatment efforts.
- Cost-effective, culturally relevant interventions should be developed separately for children in school, at home or on the streets, which have acceptability for children-using substances and can be delivered through trained manpower.
- Child welfare systems need to be strengthened, especially for homeless children, children with history of abuse in family, etc. as these should be effective safe spaces for children. Effective counselling services in these centres could reduce the risk of substance use.
- Services for children should be provided through facilities that are separate in time/space from that for adults, and should be child-sensitive and safe.
Conclusion
Substance abuse among children has received attention only recently in India and much work needs to be done to address the issue. The first step is to acknowledge this emerging problem that needs to be proactively addressed. It is important to bring stakeholders together to address the issue through a multipronged approach with an equal focus on prevention as well as treatment efforts.
| 1. | CASA. Adolescent substance use: America's #1 public health concern. The National Center on Addiction and Substance Abuse. New York:Columbia University; 2011. Available at www.casacolumbia.org/upload/2011/20110629adolescentsub stanceuse.pdf (accessed on 15 Mar 2016). [Google Scholar] |
| 2. | Squeglia LM, Jacobus J, Tapert SF. The influence of substance use on adolescent brain development. Clin EEG Neurosci 2009;40:31-8. [Google Scholar] |
| 3. | Census of India 2011. New Delhi:Office of Registrar General and Census Commissioner, Ministry of Home Affairs, Government of India; 2011. [Google Scholar] |
| 4. | Planning commission. Draft final. Report of the working group on adolescents for 11th Five Year Plan (2007–2012). New Delhi:Government of India; March 2007 Available at http://planningcommission. nic. in/aboutus/committee/wrkgrp11/ wg11_adoldev.pdf (accessed on 20 Sep 2017). [Google Scholar] |
| 5. | Tikoo VK, Dhawan A, Pattanayak RD, Chopra A. Assessment of pattern, profile and profile of substance use among children in India. New Delhi: National Commission for Protection of Child Rights (NCPCR) and All India Institute of Medical Sciences (AIIMS); 2013. Available at www.ncpcr.gov.in/view_file.php?fid=17 (accessed on 15 Mar 2016). [Google Scholar] |
| 6. | NIPCCD. Child in India. A statistical profile. New Delhi:National Institute of Public Cooperation and Child Development (NIPCCD); 2013. [Google Scholar] |
| 7. | Ray R. National survey on extent, pattern and trends of drug abuse in India. New Delhi:Ministry of Social Justice and Empowerment and United Nations Office on Drug and Crime Regional Office for South Asia; 2004. [Google Scholar] |
| 8. | National Family Health Survey-3. International Institute for Population Sciences (IIPS) and Macro International, 2007. National Family Health Survey (NFHS-3), 2005–06, India: Key Findings. Mumbai: IIPS. [Google Scholar] |
| 9. | Pal R, Tsering D. Tobacco use in Indian high-school students. Int J Green Pharm 2009;3:319-23. [Google Scholar] |
| 10. | India (ages 13–15) 2009. Fact Sheet. Global Youth Tobacco Survey. Available at www.who.int/fctc/reporting/Annexoneindia.pdf (accessed on 19 May 2013). [Google Scholar] |
| 11. | Tsering D, Pal R, Dasgupta A. Licit and illicit substance use by adolescent students in eastern India: Prevalence and associated risk factors. J Neurosci Rural Pract 2010;1:76-81. [Google Scholar] |
| 12. | Ningombam S, Hutin Y, Murhekar MV. Prevalence and pattern of substance use among the higher secondary school students of Imphal, Manipur, India. Natl Med J India 2011;24:11-15. [Google Scholar] |
| 13. | Saxena V, Saxena Y, Kishore G, Kumar P. A study on substance abuse among school going male adolescents of Doiwala Block, District Dehradun. Indian J Public Health 2010;54:197-200. [Google Scholar] |
| 14. | Qadri S, Goel RKD, Singh J, Ahluwalia S, Pathak R, Bashir H. Prevalence and pattern of substance abuse among school children in northern India: A rapid assessment study. Int J Med Sci Pub Health; 2013. doi: 10.5455/ijmsph.2013.2.271-80. [Google Scholar] |
| 15. | Baba T, Ganai A, Qadri S, Margoob M, Iqbal Q, Khan Z. An epidemiological study on substance abuse among college students of North India (Kashmir valley). Int J Med Sci Pub Health 2013;2:562-3. doi: 10.5455/ijmsph.2013.080420131. [Google Scholar] |
| 16. | Sharma N, Joshi S. Preventing substance abuse among street children in India: A literature review. Health Sci J 2013;7:137-8. [Google Scholar] |
| 17. | Ray R, Dhawan A, Ambekar A, Yadav D, Chopra A. Inhalant use among street children in Delhi: A situation assessment. New Delhi:National Drug Dependence Treatment Centre, All India Institute of Medical Sciences; 2009. [Google Scholar] |
| 18. | Pawar A, Dhawan A, Aarya KR, Varshney M. Profile of patients presenting to the child and adolescent substance use clinic at a tertiary care de-addiction centre. Indian J Psychiatry 2013;55:s42. [Google Scholar] |
| 19. | Quraishi R, Pattanayak RD, Jain R, Dhawan A. A descriptive study of clinical, haematological, and biochemical parameters of inhalant users seeking treatment at a tertiary care centre in India. Indian J Psychol Med 2013;35:174-9. [Google Scholar] |
| 20. | Saluja BS, Grover S, Irpati AS, Mattoo SK, Basu D. Drug dependence in adolescents 1978–2003 : A clinic-based observation from North India. Indian J Pediatr 2007;74: 455-8. [Google Scholar] |
| 21. | Ministry of Social Justice and Empowerment, Government of India. Available at socialjustice.nic.in/pdf/NPDDR-2014.pdf (accessed on 15 Mar 2016). [Google Scholar] |
| 22. | Rashtriya Kishor Swasthya Karyakram (RKSK). Ministry of Health and Family Welfare, Government of India, draft 2015 Available at http://nhm.gov. in/rashtriya-kishor-swasthya-karyakram.html (accessed on 7 April 2016). [Google Scholar] |
| 23. | National Policy for Drug Demand Reduction. New Delhi: Ministry of Social Justice and Empowerment, Government of India, 2014. Available at http://socialjustice.nic.in/pdfNPDDR-2014.pdf (accessed on 15 Mar 2016). [Google Scholar] |
| 24. | Rao R, Agrawal A, Ambekar A. Opioid substitution therapy under National AIDS Control Programme: Clinical practice guidelines for treatment with buprenorphine. New Delhi: Department of AIDS Control, Ministry of Health and Family Welfare, Government of India; 2014. [Google Scholar] |
| 25. | National Youth Policy 2014. New Delhi:Ministry of Youth Affairs and Sports, Government of India, 2014. Available at www.rgniyd.gov.in/sites/default/files/pdfs/ scheme/nyp_2014.pdf (accessed on 15 Mar 2016). [Google Scholar] |
Fulltext Views
3,760
PDF downloads
613




