Translate this page into:
Pneumopericardium, pneumomediastinum and surgical emphysema in spontaneous pneumothorax
Correspondence to M.K. SURESH; sureshmk303@gmail.com
To cite: Deshmukh A, Archana MP, Baalamurugan KT, Venugopal DR, Suresh MK. Pneumopericardium, pneumomediastinum and surgical emphysema in spontaneous pneumothorax. Natl Med J India 2022;35:17–18.
Abstract
Spontaneous pneumothorax leading to pneumomediastinum, pneumopericardium and surgical emphysema is a benign condition. Progression to the development of epidural pneumatosis is rare. We report a 19-year-old man who presented with dyspnoea and swelling of the chest wall following a bout of cough. Bilateral subcutaneous emphysema was palpated on the anterior chest wall from the sternum to the midaxillary regions. His chest X-ray revealed subcutaneous emphysema and pneumopericardium. His computed tomography of the thorax to rule out life-threatening conditions revealed bilateral subcutaneous emphysema, pneumomediastinum, pneumo-pericardium and pneumothorax. He was transferred to the intensive care unit. An intercostal drainage tube was inserted in the left pleural cavity. The patient was followed up with repeat chest X-rays. The patient’s symptom got relieved and was discharged after day 9. Diagnosis of pneumomedia-stinum may not be as lamentable as it is seen. Close cardio-pulmonary monitoring is mandatory for complications and accompanying conditions. Most patients with uncomplicated spontaneous pneumomediastinum respond well to oxygen and conservative management. In this case, the patient’s symptoms and severe tachypnoea prompted the insertion of an intercostal drainage tube.
INTRODUCTION
Spontaneous pneumomediastinum and pneumopericardium is the presence of free air in the mediastinal structures and pericardial sac without any precipitating cause.1 Although rare, it is seen in young adults presenting with dyspnoea and chest pain.2 It is usually self-limited unless tension pneumomediastinum, tension pneumothorax, air tamponade, cardiac herniation and oesophageal rupture occur.3,4 A 19-year-old man presented with spontaneous pneumothorax, pneumomediastinum, bilateral surgical emphysema and pneumopericardium without any identifiable cause.
THE CASE
A 19-year-old man in completely good health presented with sudden onset of breathlessness and chest pain with gradual swelling of the chest, neck, face and bilateral axilla. He had no history of fever with cough, weight loss, vomiting, dislodgement of foreign body, substance abuse or trauma in the past. He was a non-smoker and did not consume alcohol. On examination, the patient was afebrile, his pulse rate was 110/minute, respiratory rate 18/minute, blood pressure 130/86 mmHg and arterial saturation (SpO2) was 95% on room air. On palpation, the trachea was central and there was subcutaneous emphysema on the face, neck and chest. Auscultatory findings of the chest were greatly obscured in the presence of skin crepitations. Other clinical examination was normal. Electrocardiogram showed sinus tachycardia. Chest X-ray revealed pneumopericardium, subcutaneous emphysema and air around the paratracheal space conclusive of pneumomediastinum (Figs 1 and 2). His complete blood count and liver function tests were within normal limits. Fibreoptic bronchoscopy was normal. Computed tomography of the neck and thorax showed evidence of pneumomediastinum and pneumopericardium with extensive subcutaneous emphysema involving the neck, chest and abdominal wall and minimal pneumothorax bilaterally. Air pockets were seen in the left psoas and quadratus lumborum muscle. Air spaces were seen trapped around the nerve roots and vessels in the axillary region bilaterally which suggested future progression of air seeping along the nerve roots into the epidural space and causing epidural pneumatosis (Fig. 3).
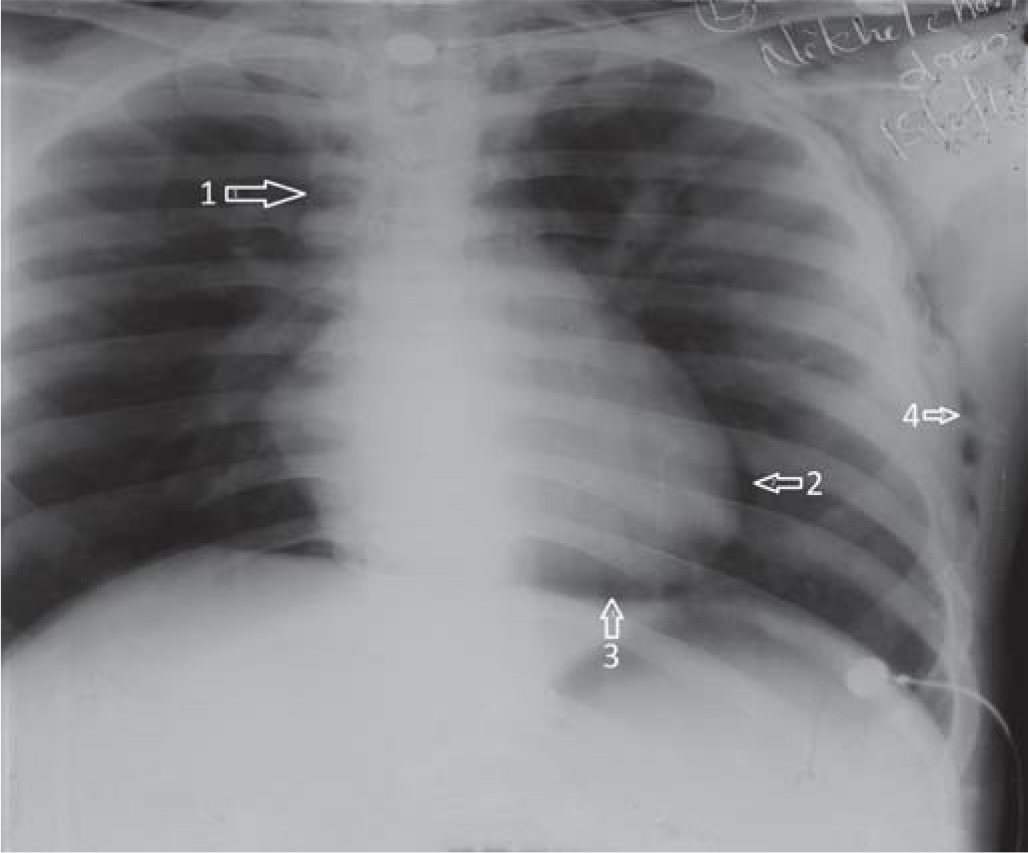
- Arrow (1) Paratracheal radioluscence suggestive of pneumomediastinum; (2) pneumopericardium; (3) pneumopericardium with air space between heart and diaphragm; (4) subcutaneous emphysema
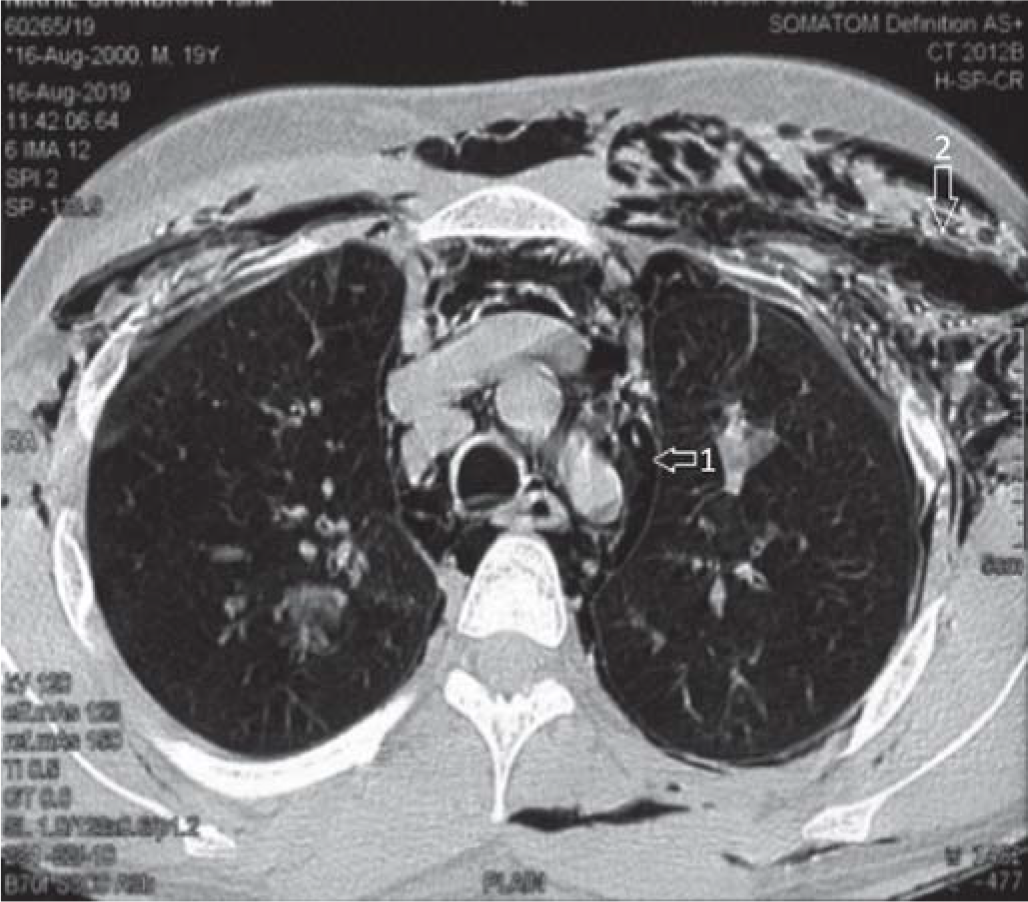
- Arrow (1) pneumomediastinum; (2) subcutaneous emphysema
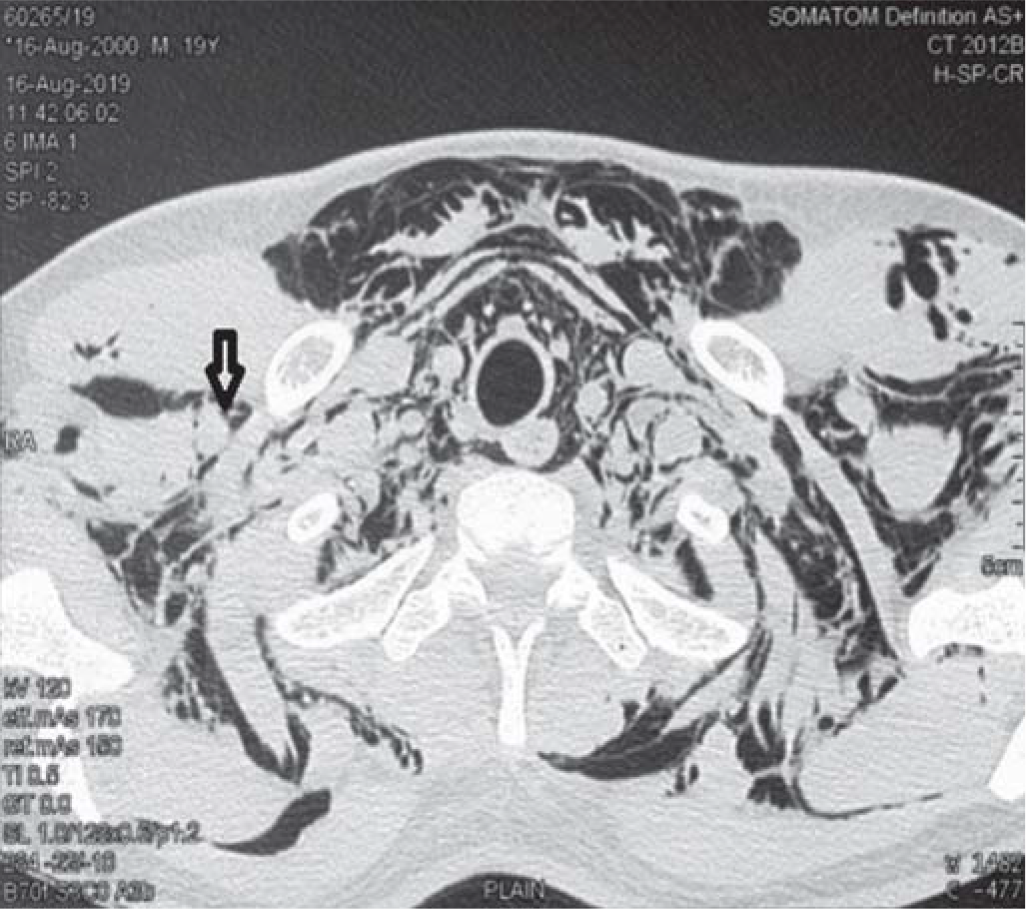
- Arrow depicting air void around the axillary nerve roots suggestive of impending occurrence of epidural pneumatosis
The patient was managed with 100% oxygen but the tachypnoea persisted and hence a left intercostal drainage tube was placed. He was managed conservatively with 100% oxygen inhalation, regular blood gas analysis, broad-spectrum prophylactic antibiotics, analgesic and bed rest in the intensive care unit. Progress was uneventful and the intercostal drainage tube was removed on day 9.
DISCUSSION
Spontaneous pneumomediastinum is a self-limiting benign condition that predominantly affects the age group of 17–25 years.5 The incidence is low at 1 in 30 000 hospital admissions.6 It is sometimes associated with conditions leading to increased intrathoracic pressure such as asthma, severe coughing, Valsalva manoeuvre,7 diabetic ketoacidosis, vomiting, childbirth and inhalational drug abuse.8 In these instances, it is thought that excessive intra-alveolar pressures lead to rupture of perivascular alveoli. The free air then dissects from the ruptured alveoli along the bronchovascular sheaths towards the mediastinum to produce spontaneous pneumomediastinum. This sequence of events is known as the ‘Macklin effect’.9
Spontaneous pneumomediastinum is rare, but its association with pneumothorax and pneumopericardium is even rarer. Epidural pneumatosis occurs when free air tracks through fascial planes in the brachial plexus, axillary arteries, intercostal nerves or intervertebral foramina.10 Air tamponade is similar in pathophysiology to cardiac tamponade. Cardiac herniation can also lead to cardiac pump dysfunction.4
Before making a diagnosis of spontaneous pneumothorax, other causes of pneumomediastenum have to be ruled out. Boerhaave syndrome, skin infection and soft-tissue infection caused by gas-producing organisms, trauma and foreign body are the other causes. CT scan is more sensitive than X-ray in detecting free air in the mediastinum. Air leaks from the oesophagus may be detected.
The treatment is conservative and consists of 100% oxygen inhalation, broad-spectrum antibiotics and avoiding Valsalva manoeuvre. Breathing of 100% oxygen will enhance reabsorption of free air by increasing the gradient of nitrogen between alveoli and tissue.6
Epidural pneumatosis occurring through seepage of air along the nerve sheaths can cause radiculopathy and paraplegia; hence, follow-up of this rarely seen entity is important.
Conclusion
The occurrence of spontaneous pneumomediastenum, subcutaneous emphysema, pneumopericardium and pneumothorax without any precipitating cause is a rare event, which can be diagnosed only with diligent clinical and radiological examination. Progression to epidural pneumatosis can be precluded with early intervention. Although the treatment is conservative in critical care settings, surgical intervention may be required with follow-up.
Conflicts of interest
None declared
References
- A case of spontaneous pneumomediastinum and pneumopericardium in a young adult. Korean J Intern Med. 2001;16:205-9.
- [Google Scholar]
- Spontaneous pneumomediastinum in an adolescent. Med J Armed Forces India. 2005;61:192-4.
- [Google Scholar]
- Blunt traumatic rupture of the heart and pericardium: A ten-year experience (1979–1989) J Trauma. 1991;31:167-72.
- [Google Scholar]
- Spontaneous pneumomediastinum following vocal effort: A case report. Radiol Bras. 2010;43:137-9.
- [Google Scholar]
- Association of spontaneous pneumomediastinum with substance abuse. West J Med. 1990;152:301-4.
- [Google Scholar]
- Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: An interpretation of the clinical literature in the light of laboratory experiment. Medicine (Baltimore). 1944;23:281-358.
- [Google Scholar]
- Epidural pneumatosis and diffuse soft tissue free air as a complication of diabetic ketoacidosis. Am J Respir Crit Care Med. 2012;185:e5.
- [Google Scholar]




