Translate this page into:
Preoperative cardiology referral practices at a tertiary care centre: A retrospective observational study
Correspondence to PRIYANKA PAVITHRAN, Anugraha, 2/756-B, Othayamangalam Road, Karaparamba, Calicut 673010, Kerala, India; priyanka.pavithran@gmail.com
To cite: Pavithran P, Arayullathil B. Preoperative cardiology referral practices at a tertiary care centre: A retrospective observational study. Natl Med J India 2022;35:11–13.
Abstract
Background
Preoperative consultations and testing add to healthcare costs. Unnecessary consultations lead to further testing and delay in surgery. Guidelines help us in clinical practice but are seldom followed. We studied the appropriateness of our preoperative cardiology referrals according to the guidelines and functional utility of the consultations.
Methods
We reviewed the records of patients who underwent elective non-cardiac surgery to identify those who had a preoperative cardiology consult. Appropriateness of the referral was assessed by comparing with the 2014 American College of Cardiology/American Heart Association guidelines. Any recommendations made, major adverse cardiac events and perioperative outcome were also noted.
Results
Only 71 (15.5%) referrals were appropriate according to the guidelines. A majority of them were for preoperative clearance. The most common recommendation was to withhold antiplatelet medications. None of the consultations made any change in the anaesthetic or surgical plan. Six patients had major perioperative adverse cardiac events.
Conclusion
The majority of consultations were by surgeons and were not indicated according to the guidelines and did not have any impact on patient outcome. A large proportion of these patients had low cardiac risk index. As anaesthesiologists, we are best equipped to quantify risk and optimize a patient and should be the leaders of the perioperative period.
INTRODUCTION
Preoperative evaluation of a cardiac patient for non-cardiac surgery is challenging. This task is often delegated to the cardiologist. Previous studies have shown that a preoperative cardiology consult is an overused resource with no proven benefit.1–3 Most of these studies were done in western countries.
Limited literature is available on the present-day scenario in India. We evaluated the appropriateness, variations, yield and impact of the preoperative cardiology referrals of patients posted for non-cardiac surgery at our centre.
METHODS
Approval of the institutional ethics committee was obtained. We conducted a retrospective observational study among patients who underwent elective non-cardiac surgery from January to August 2018. Patient consent was waived in view of the study being retrospective in nature. At our institution, all patients posted for surgery under general or regional anaesthesia undergo a pre-anaesthetic check-up. We have a fully functional anaesthesia outpatient clinic, which is not properly utilized by the surgeons. On average, 20%–40% of surgical patients are seen in this clinic, days before surgery, providing us opportunities to evaluate and optimize them. The majority of patients are seen at the bedside, on the night before or day of surgery. The surgeons perform the preoperative consultations as they deem necessary. The hospital information system was used to obtain the medical records. Data were collected by a single investigator. All patients above 20 years of age who underwent elective non-cardiac surgery were included. Obstetric, cardiac, transplant surgeries and those performed under local anaesthesia were excluded. The records were reviewed to identify the patients who underwent preoperative cardiology consultation. A predefined proforma including the patient demographics, comorbid conditions, functional capacity, surgery planned, any important perioperative cardiac event, length of hospital stay and perioperative outcome was used. The consultation request was examined to determine if it specified a particular question or just demanded ‘clearance for surgery’. The consultation notes were examined in detail to identify any new pathology diagnosed, recommendations made and any diagnostic or therapeutic intervention suggested. The consequences of the recommen-dations and patient outcome were also noted. Our primary objective was to evaluate the appropriateness of the consulta-tions and the tests as per the 2014 American College of Cardiology (ACC)/American Heart Association (AHA) guidelines for preoperative evaluation of cardiac patients for non-cardiac surgery. The secondary objectives were to explore the variations in these referrals along with the yield and impact of these preoperative consultations. Records of a total of 2956 patients were reviewed, and 473 (16%) patients were included. Of these, records of 16 patients were incomplete and were excluded.
Sample size calculation was done by the proportion method. A previous study by Aslanger et al.4 had shown that 25% of cardiology referrals were appropriate. With alpha error at 5% and precision at 4%, the calculated sample size was 450.
Statistical analysis was done using the Statistical Package for the Social Sciences version 21.0. Continuous data were represented as mean (standard deviation [SD]) and categorical data were represented as frequency with percentage.
RESULTS
A total of 457 patients were included in the final analysis. The demographics of the patients are shown in Table I. Nine patients had pacemakers and AHA advises a preoperative cardiology consult for such patients. The remaining referrals were evaluated for appropriateness by comparing with the 2014 ACC/AHA algorithm (Fig. 1). Only 71 (15.5%) of the cardiology consultations were appropriate according to the guidelines.
| Characteristic | n(%) |
|---|---|
| Mean (SD) age in years | 67.2 (10.24) |
| Age distribution (years) | |
| <40 | 9 (2) |
| 40–65 | 171 (37.4) |
| >65 | 277 (60.6) |
| Sex | |
| Men | 274 (60) |
| Women | 183 (40) |
| Comorbid conditions | |
| Coronary artery disease | 142 (31.1) |
| Cardiac intervention | 102 (22.3) |
| Hypertension | 265 (58) |
| Diabetes mellitus | 217 (47.5) |
| Chronic kidney disease | 30 (6.6) |
| Functional capacity | |
| <4 METS | 130 (28.4) |
| >4 METS | 327 (71.6) |
| ASA class | |
| 1 | 63 (13.8) |
| 2 | 373 (81.6) |
| 3 | 18 (3.9) |
| 4 | 3 (0.7) |
| RCRI | |
| 0 | 167 (36.5) |
| 1 | 225 (49.2) |
| 2 | 33 (7.2) |
| 3 | 26 (5.5) |
| 4 | 6 (1.2) |
| Cardiac risk proposed by cardiologist | |
| High | 26 (5.7) |
| Intermediate | 131 (28.7) |
| Mild | 300 (65.6) |
METS metabolic equivalents ASA American Society of Anaesthesiologists RCRI revised cardiac risk index
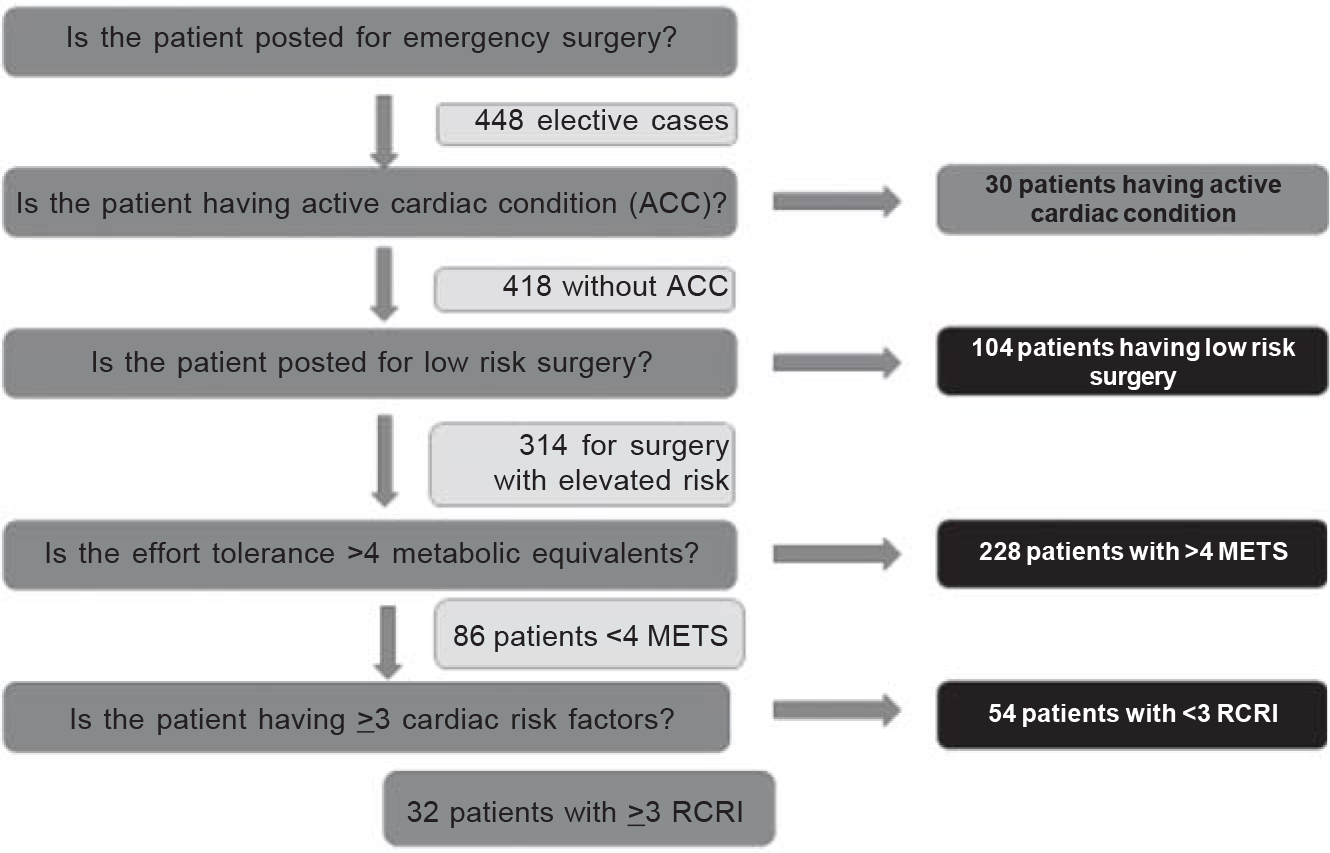
- Assessing the appropriateness of the cardiology referral
- METS Metabolic equivalents RCRI Revised Cardiac Risk Index ACC American College of Cardiology
The majority (94.5%) of referrals were by the surgeon. The detailed review of the consultation notes revealed that only 72 (15.8%) patients had a request posing a specific question for evaluation or management of an abnormality. The majority (84.2%) of patients were referred for preoperative clearance. Cardiologists made recommendations regarding drug modification in 158 (34.6%) patients, and the most common recommendation was to stop antiplatelet medication 5 days before surgery. Eighteen patients were suggested further evaluation and interventions. These tests did not reveal any abnormality in any patient. Four patients were postponed for 3 weeks. All the patients who underwent a cardiology consult had an echocardiogram done, which was normal in 87 (41.2%). In the remaining patients, 32 had regional wall motion abnormality (15%), 82 had age-related diastolic dysfunction (38.9%), 7 had concentric left ventricular hypertrophy (3.3%) and 3 had valvular anomalies (1.4%).
Six patients had perioperative major adverse cardiac events including acute coronary syndrome (3), atrial fibrillation (1) and cardiac arrest (2), of which three patients died in the postoperative period.
Orthopaedic surgeons sent the most number of referrals (41.3%). No change in anaesthetic or surgical plan was made after the cardiology consultations in any of the patients. The median length of hospital stay was 5 (4–7) days.
DISCUSSION
Our study revealed that a majority of the preoperative cardiology consultations were unindicated as per the AHA guidelines. Even patients posted for low-risk surgery, who had no risk factors, had been referred. In general, the cardiology consultations did not provide any additional prognostic guidance leading to change in anaesthetic or surgical plan, proving the futility of such referrals.
The ACC/AHA guidelines are based on the theme that a person who did not need a cardiology evaluation otherwise does not need one merely because he is a surgical candidate.5 The three drivers for a preoperative consult quoted by Park are presence of risk factors, risk of surgery and functional status of the patient.6 Kleinman states that other than for management of active cardiac condition, there is little the cardiologist can do that an anaesthesiologist cannot do.7
Surgeons asked for the majority of referrals. Ideally, patients should be evaluated weeks to days before surgery in an outpatient clinic conducted by anaesthesiologists for risk stratification and optimization. It has been shown that implementation of preoperative anaesthesia clinics can improve patient care and reduce costs.8 Fear of medicolegal litigations is one reason surgeons request these referrals, but blanket consultations cannot afford protection in the face of a litigation.
Studies identify unnecessary preoperative testing and consults as a major contributor to healthcare costs.9,10 It has been shown that random preoperative consults and testing have no positive impact on perioperative outcome.11,12 Cardiology was identified to be the most sought after specialty. Paucity of robust audit data keeps us ignorant on the deficiencies of our perioperative care.
The retrospective nature of our study itself is a limitation. It was done in a single centre, and the results show the referral patterns unique to our institute, which cannot be generalized. Follow-up was limited till the patient was discharged from the hospital.
Conclusion
Preoperative cardiology consultation is often performed in unindicated situations. Our study shows the futility of such unnecessary testing and referrals. Implementing outpatient anaesthesia clinics and following guidelines can help improve perioperative outcome. From being intraoperative physicians, anaesthesiologists need to become leaders of the perioperative period and take over perioperative medicine.
Conflicts of interest
None declared
References
- Impact of preoperative cardiology consultation prior to intermediate-risk surgical procedures. Eur J Clin Invest. 2018;48:e12794.
- [Google Scholar]
- Preoperative cardiac evaluation does not improve or predict perioperative or late survival in asymptomatic diabetic patients undergoing elective infrainguinal arterial reconstruction. J Vasc Surg. 2005;41:38-45.
- [Google Scholar]
- The preoperative cardiology consultation: Indications and risk modification. Neth Heart J. 2017;25:629-33.
- [Google Scholar]
- The preoperative cardiology consultation: Goal settings and great expectations. Acta Cardiol. 2011;66:447-52.
- [Google Scholar]
- ; American College of Cardiology; American Heart Association 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64:e77-137.
- [Google Scholar]
- Preoperative cardiology consultation: How helpful is it? Anesthesiology. 2003;99:1240.
- [Google Scholar]
- The effect of alterations in a preoperative assessment clinic on reducing the number and improving the yield of cardiology consultations. Anesth Analg. 2002;95:1563-8.
- [Google Scholar]
- International comparison of preoperative testing and assessment protocols and best practices to reduce surgical care costs: A systematic literature review. Adv Health Care Manag. 2015;17:161-94.
- [Google Scholar]
- An observational cohort study on pre operative investigations and referrals: How far are we following recommendations? Indian J Anaesthesiol. 2016;60:552-9.
- [Google Scholar]
- Effectiveness of preoperative medical consultations by internal medicine physicians: A systematic review. BMJ Open. 2017;7:e018632.
- [Google Scholar]
- Patterns of preoperative consultation and surgical specialty in an integrated healthcare system. Anesthesiology. 2013;118:1028-37.
- [Google Scholar]




