Translate this page into:
Prevalence of psychological morbidity and its correlates among school-going adolescents of urban Puducherry, India
Correspondence to K.C. PREMARAJAN; kcpremarajan@yahoo.com
To cite: Srinivasan M, Premarajan KC, Reddy MM, Menon V, Kumar SG. Prevalence of psychological morbidity and its correlates among school-children of urban Puducherry, India. Natl Med J India 2022;35:88–92.
Abstract
Background
Experiencing poor mental health during adolescence predisposes an individual to psychiatric morbid conditions in adulthood. We estimated the prevalence of psychological morbidity and its associated factors, among school-going adolescents in higher secondary schools of urban Puducherry.
Methods
We did this cross-sectional study among adolescents studying in classes 11 and 12 from selected schools of urban Puducherry, including one government and three private schools. Study tools used were the General Health Questionnaire-12 and Perceived Stress Scale-10 to assess psychological morbidity and perceived psychological stress in adolescents, respectively. Risk factors in academic, environmental, personal and health-related domains were captured using a structured questionnaire. Study questionnaires were self-administered by the participants in classrooms. Bivariate and multivariate analyses were done to identify risk factors for psychological morbidity.
Results
Of the 820 adolescents surveyed, the prevalence of psychological morbidity was 25.4% (95% CI 22.4– 28.5). Academic factors such as reporting peer pressure for academic performance and lack of extracurricular activities at school were associated with psychological morbidity. Among health-related factors, adolescents who reported having difficulty in coping with pubertal changes, being worried about their physical appearance, reporting substance abuse and experiencing sleep disturbances had greater chances of having screened with psychological morbidity. Of note, adolescents with psychological stress had 2.5 times higher chances of having psychological morbidity.
Conclusions
We estimated that 1 in 4 school-going adolescents in urban Puducherry suffered psychological morbidity. Reducing the academic burden and advocating health promotion through a life skills approach may improve mental wellness in Indian adolescents.
INTRODUCTION
Adolescence—a phase of transition from childhood to adulthood is marked with changes that individuals must endure in spheres of physical, emotional and societal aspects of their life.1 Supportive parenting, encouraging school environment and strong community support smoothens this transition and helps to attain good well-being in adolescents.2 Ensuring adolescent well-being is important, as it enhances self-esteem, academic achievement, problem-solving skills and social connectedness in later adulthood.1 Fortunately, the adolescent phase is uneventful in many, leaving out a subset of them who would succumb to adverse life experiences and experience poor mental health.
In the global context, studies have estimated that 1 in every 4 to 5 adolescents experience any form of mental disorder in a given year.1 Further, it has been studied in high-income settings that most of the mental disorders that manifest in early adulthood had their onset as early as 12–24 years of age.1 In India, depression and anxiety, being part of the spectrum of common mental disorders (CMD), contributed to 34% and 19%, respectively, of the total disability-adjusted life years lost due to mental disorders in 2017.3 Thus, it is important to do research focusing on the burden of CMDs and their predictors from a public health perspective.
Important predictors of CMDs in adolescents are: residing in an urban city, having to face emotional abuse and/or neglect from parents or caregivers.4,5 The prevailing school environment has a considerable role to play in mental well-being, where adolescents with difficulty in coping with academic pressure and lacking supportive relationships with peers undergo considerable psychological stress.6 The background stress accentuates in adolescents, particularly during their higher secondary education, given the existing bottleneck for opportunities to pursue higher education in India, further lowering the threshold for suffering psychological morbidity. Since schools are a better platform for delivering mental health interventions, having school-based estimates of psychological morbidity and risk profiles is important to decide on context-specific interventions. With this background, we estimated the burden of psychological morbidity in school-going adolescents in classes 11 and 12 in schools of urban Puducherry, along with its correlates such as academic, personal and health-related, with a special focus on perceived psychological stress.
METHODS
Study setting
We conducted this school-based cross-sectional study during 2014–15 in the Union Territory of Puducherry, which comprised two municipalities—Ozhukarai and Pondicherry. The study area chosen was Ozhukarai municipality due to its proximity to our institute where this research was carried out. The study area had a total of 31 schools (22 private and 9 government) offering higher secondary education and of these, 23 schools (20 private and 3 government) had a co-educational system in place. Adolescents studying in classes 11 and 12 from the 23 coeducational schools formed our study population. Our sampling frame consisted of 4516 school-going adolescents from 23 schools, with 3575 (79%) and 941 (21%) of these, belonging to private and government schools, respectively.
Sampling strategy
We estimated a sample size of 700 participants, based on the reported prevalence of psychological morbidity of 9% among adolescents from urban Goa,4 with an absolute precision of 3%, α-error of 5%, and a design effect of 2. A stratified sampling approach was used considering the possible confounding effect by type of school in estimating psychological burden. Hence, participants were selected from both private and government schools (strata). To arrive at the number of participants to be chosen under these categories, we used a proportionate-to-size sample method where we applied the proportions—79% (private) and 21% (government) derived from our sampling frame to the sample size, and planned to recruit at least 553 (79% of 700) and 147 (21% of 700) from private and government schools, respectively. Based on the number of participants enrolled in each school, we chose three private and one government school, on a convenient basis, to meet the sample size.
Data collection
Data were collected using a structured proforma to collect sociodemographic details, a General Health Questionnaire (GHQ-12) to measure psychological morbidity, a stress factor questionnaire to capture risk factors for psychological morbidity, and a Perceived Stress Scale (PSS-10) to measure psychological stress. The GHQ-12 designed by Goldberg and Williams has demonstrated good internal consistency, with a Cronbach alpha value of 0.83 and has been widely studied among adolescents from diverse Indian settings.7 We used the Tamil version of GHQ-12, which has been validated in southern India.8 There are 12 items in the questionnaire and the responses were coded in a binary fashion as 0-0-1-1.9 The total score ranges between 0 and 12 and participants who scored 6 and above met the case definition for psychological morbidity.9 While filling the questionnaires, participants were requested to consider the past 1 month as the reference period.
To identify risk factors associated with psychological morbidity, a semi-structured stress factor questionnaire was designed under the categories—academic, environmental factors related to school, personal and health-related factors. This questionnaire was prepared based on the list of probable stressors noted down by 50 school-going adolescents sampled from 3 schools of urban Puducherry that are different from those schools selected for the main study. The responses were pile-sorted and the most frequently reported factors were included in the questionnaire, in addition to other factors that were noted down by the investigators of this study following the literature review.
In addition to health-related factors reported by the participants, we screened for perceived psychological stress in participants using a PSS-10 scale, developed by Cohen et al.10 The scale has 10 questions, with responses being marked in a 5-point Likert scale ranging from never (0) to always (4). For items 4, 5, 7 and 8, which were worded positively, we reversed the scores obtained (i.e.) 0=4, 1=3, 2=2 and summed up to arrive at net scores. The total score of the scale ranged between 0 and 40, and participants who scored above the median value met the case definition for perceived psychological stress.11 The median score was used as the cut-off for the PSS scale, as there is limited evidence in the literature providing a cut-off score, which is validated in the Indian population.12 The test–retest correlation of PSS-10 was reported as 0.85, by the previous studies done among Indian college students.13 Using bilingual experts, we did a translation of the English version of PSS-10 and stress factors questionnaire into Tamil followed by a back translation into English. The original version and back-translated version of the questionnaire was compared by the investigator to ensure content validity.
This study was approved by the Institute Scientific Advisory and Ethics Committee (PGMR/CM/04/2014). We obtained permission from the Directorate of School Education, Puducherry and the principals of participating schools for conducting the study. On the day of the survey, the study investigator read out the questionnaire in the classroom and explained the sections of the questionnaire with real-life situations for better understanding. All participants who were present on the day of the survey and provided their written assent for participation were included. Participants self-administered the questionnaires in the presence of the investigator, and class teachers were requested to wait outside the classroom until the end of the survey, to make participants feel comfortable while filling the questionnaire, without fear of being observed. We collected anonymized data as we felt that incorporating data identifiers would bias the responses.
Statistical analysis
Categorical variables including demographic details and variables in the stress factor questionnaire were expressed as percentages. Distribution of age, GHQ and PSS scores were represented using mean (standard deviation [SD]) or median (interquartile range [IQR]) based on the normality. To measure the association between probable stress factors and psychological morbidity, bivariate and multivariate analysis was considered using generalized linear models and reported prevalence rate ratios (PRR) with 95% confidence intervals. Multivariate analysis was conducted after ruling out collinearity between outcome and independent variables. Data were single-entered using EpiData Entry software version 3.1 (EpiData Association, Odense, Denmark). All analysis was done using Stata version 13 (StataCorp. 2013. Stata Statistical Software. Release 13. College Station, TX: StataCorp LP).
RESULTS
A total of 820 school-going adolescents in classes 11 and 12 of the selected schools were surveyed, with 627 participants chosen from 3 private and 193 participants from 1 government school. The mean (SD) age of the participants was 16.1 (0.8) years. The survey included 417 (50.9%) males and 415 (50.6%) were studying in class 11. The median (IQR) GHQ scores obtained by the participants was 3 (1–6).
The prevalence of psychological morbidity measured using GHQ-12 was 25.4% (95% CI 22.4–28.5). Psychological morbidity did not vary significantly within the subgroups of gender, type of school and current class of study. Considering academic factors, adolescents reporting peer pressure for academic performance (PRR 1.3; 95% CI 1.0–1.6) and lack of extracurricular activities at school (PRR 1.5; 95% CI 1.1–1.8) had higher chances of having psychological morbidity (Table I).
| Factor | n | Psychological morbidity | 95% CI | ||
|---|---|---|---|---|---|
| Present (n=208), n (%) | Absent (n=612), n (%) | Unadjusted PRR | Adjusted PRR | ||
|
Demographic characteristics Gender Male |
417 | 118 (28.3) | 299 (71.7) | 1 | 1 |
| Female | 403 | 90 (22.3) | 313 (77.7) | 0.8 (0.6-1.0) | 1.0 (0.8-1.3) |
| Class | |||||
| 11 | 415 | 101 (24.3) | 314 (75.7) | 0.9 (0.7-1.2) | 1 (0.9-1.3) |
| 12 | 405 | 107 (26.4) | 298 (73.6) | 1 | 1 |
|
Type of school Private |
627 | 159 (25.4) | 468 (74.6) | 1.0 (0.7-1.3) | 1 |
| Government | 193 | 49 (25.4) | 144 (74.6) | 1 | 0.9 (0.7-1.1) |
|
Academic factors Getting worried when the examinations are near Yes |
653 | 175 (26.8) | 478 (73.2) | 1.4 (1.0-1.9) | 1.0 (0.8-1.4) |
| No | 167 | 33 (19.8) | 134 (80.2) | 1 | 1 |
|
Burdened with home-work given at the school Yes |
451 | 138 (30.6) | 313 (69.4) | 1.6 (1.3-2.1) | 1.3 (1.0-1.6) |
| No | 369 | 70 (19) | 299 (81) | 1 | 1 |
|
Being pressurized by peer performance in examinations Yes |
336 | 114 (33.9) | 222 (66.1) | 1.8 (1.4-2.2) | 1.3 (1.0-1.6) |
| No | 484 | 94 (19.4) | 390 (80.6) | 1 | 1 |
|
Lack of extracurricular activities at school Yes |
324 | 119 (36.7) | 205 (63.3) | 2.1 (1.6-2.6) | 1.5 (1.1-1.8) |
| No | 496 | 89 (17.9) | 407 (82.1) | 1 | 1 |
|
Environmental factors Poor infrastructure in the school Yes |
383 | 110 (28.7) | 273 (71.3) | 1.3 (1.0-1.6) | |
| No | 437 | 98 (22.4) | 339 (77.6) | 1 | - |
|
Bullied by friends Yes |
223 | 82 (36.8) | 141 (63.2) | 1.7 (1.4-2.2) | 1.2 (0.9-1.5) |
| No | 597 | 126 (21.1) | 471 (78.9) | 1 | 1 |
|
Personal factors Parental conflicts/separation Yes |
125 | 52 (41.6) | 73 (58.4) | 1.9 (1.4-2.4) | 0.8 (0.6-1.0) |
| No | 695 | 156 (22.5) | 539 (77.6) | 1 | 1 |
|
Financial problems in the family Yes |
370 | 111 (30) | 259 (70) | 1.4 (1.1-1.8) | - |
| No | 450 | 97 (21.6) | 353 (78.4) | 1 | - |
|
Parental pressure in choosing the career Yes |
402 | 120 (29.9) | 282 (70.2) | 1.4 (1.1-1.8) | 1.0 (0.8-1.3) |
| No | 418 | 88 (22.1) | 330 (79.0) | 1 | 1 |
|
Worried by the habit of substance abuse in father Yes |
205 | 70 (34.2) | 135 (65.9) | 1.5 (1.2-1.9) | 0.9 (0.7-1.2) |
| No | 615 | 138 (22.4) | 477 (77.6) | 1 | 1 |
|
Subjected to parental torture Yes |
90 | 42 (46.7) | 48 (53.3) | 2.1 (1.6-2.7) | 0.9 (0.7-1.1) |
| No | 730 | 166 (22.7) | 564 (77.3) | 1 | 1 |
|
Health-related factors Unable to cope with pubertal changes Yes |
356 | 106 (29.8) | 250 (70.2) | 1.4 (1.1-1.7) | 1.3 (1.1-1.7) |
| No | 464 | 102 (22)1 | 362 (78)1 | 1 | 1 |
|
Worried about physical appearance Yes |
396 | 128 (32.3) | 268 (67.7) | 1.7 (1.3-2.2) | 1.3 (1.0-1.6) |
| No | 424 | 80 (18.9) | 344 (81.1) | 1 | 1 |
|
Having the habit of substance abuse Yes |
23 | 14 (60.9) | 9 (39.1) | 2.5 (1.8-3.6) | 1.8 (1.2-2.6) |
| No | 796 | 194 (24.3) | 603 (75.7) | 1 | 1 |
|
Experiencing sleep difficulties Yes |
224 | 100 (44.6) | 124 (55.4) | 2.5 (2.0-3.1) | 1.8 (1.4-2.3) |
| No | 596 | 108 (18.1) | 488 (81.9) | 1 | 1 |
|
Presence of perceived psychological stress Yes |
433 | 166 (38.3) | 267 (61.7) | 3.5 (2.6-4.8) | 2.4 (1.8-3.4) |
| No | 387 | 42 (10.9) | 345 (89.2) | 1 | 1 |
CI confidence interval PRR prevalence rate ratio
Personal factors such as having parental conflicts, being subjected to torture by parents and reporting substance abuse by the father had a significant association with psychological morbidity only in univariate analysis and not in multivariate analysis. Among health-related factors, adolescents who reported that they had difficulty in coping with pubertal changes (PRR 1.3; 95% CI 1.1–1.7), being worried about their physical appearance (PRR 1.3; 95% CI 1.0-1.6), reporting substance abuse (PRR 1.8; 95% CI 1.2–2.6) and experiencing sleep disturbances (PRR 1.8; 95% CI 1.4–2.3) had greater chances of being screened with psychological morbidity (Table I).
A total of 384 (46.8%) school-going adolescents were screened to have psychological stress using PSS-10. Median (IQR) PSS scores obtained by the participants were 19 (13–25). Participants with psychological morbidity had a higher median (IQR) PSS scores (26 [20–30]) than those without psychological morbidity (17 [12–22]; Fig. 1). In the multivariate model, participants with psychological stress had 2.4 times higher chances of having psychological morbidity (PRR 2.4; 95% CI 1.8–3.4; Table I).
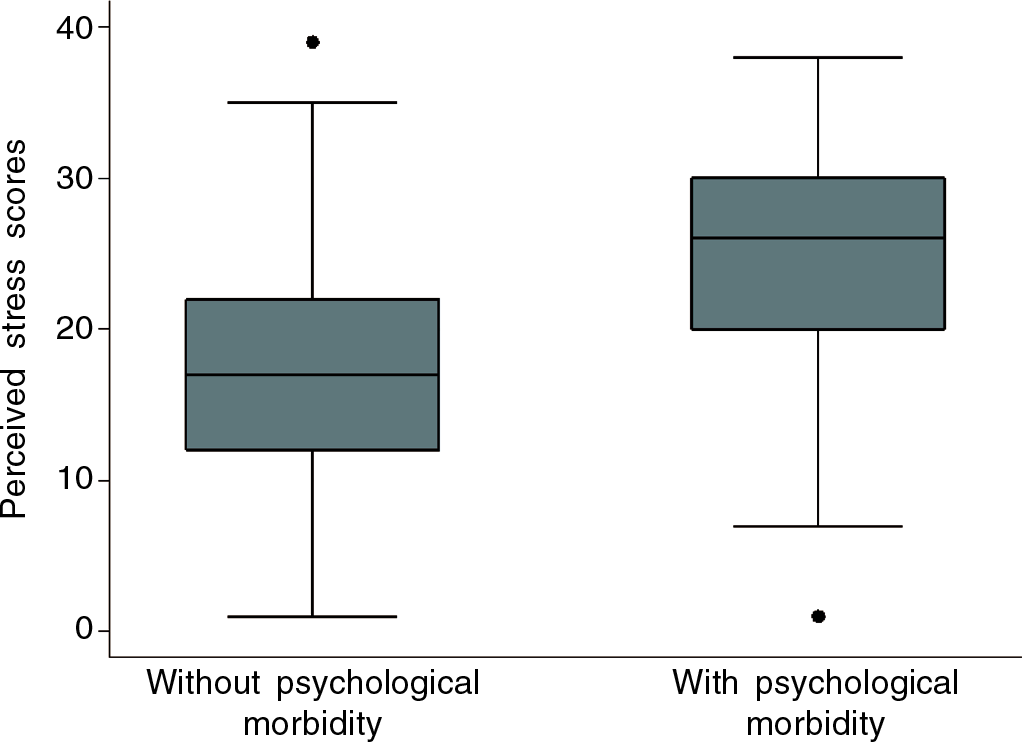
- Distribution of scores of perceived stress scale-10 among school-going adolescents with or without psychological morbidity
DISCUSSION
This cross-sectional survey conducted in school-going adolescents in higher secondary schools of urban Puducherry showed the prevalence of psychological morbidity of about 25%, using the GHQ-12 questionnaire. Our estimate is comparable to the pooled estimates of psychological morbidity, ranging between 25% and 31%, generated from a meta-analysis of studies done among adolescents using GHQ-12 in global settings.14 However, the fact that this meta-analysis had a lesser representation of studies from low- and middle-income countries (LMICs) limits the comparability of its estimates to our study and also highlights the need to generate more evidence on burden estimates of psychological morbidity from LMICs, particularly in the Indian setting.14 In 2015, the population-level estimates of overall mental disorders, from the National Mental Health Survey in India (NMHS), was shown to be 7.3% (5.8–8.7) among Indian adolescents, with depression, anxiety and stress-related disorders contributing to the maximum.15 Compared to NMHS, our study estimated psychological morbidity almost three times that of the NMHS survey and this difference could be because of having a community-based sampling approach and using a different study tool, the MINI-Kid questionnaire in the NMHS survey.
While looking at various Indian studies on adolescent mental health, as summarized in a recent narrative review, we found heterogeneity in the estimation of psychological morbidity across the Indian study settings.16 This review highlighted that the study setting, either school-based or community-based, could be a determinant for variation in burden estimates. Further, school-based studies provided a wider estimate of depression ranging between 2% and 80%, compared to community-based studies, which provided more conservative estimates, ranging between 0% and 16%.16 The probable explanation for having higher estimates of psychological morbidity in school settings could be the clustering effect of risk factors and outcomes, at the level of school. On the contrary, community-based sampling offers scope for a representative sample by eliminating the cluster effect brought in by the schools. Also noted was that the Indian studies based on screening tools such as GHQ or PHQ have estimated psychological morbidity in adolescents on a higher side compared to those studies using tools constructed based on DSM-IV and/or ICD-10 criteria such as Development and Well-being assessment or MINI-KID, which reported a conservative estimate of psychological morbidity ranging between 1.8% and 7.3%.15,17 Therefore, varied estimates of psychological morbidity in studies included in the review would be due to the use of different tools for evaluation across these studies, application of different cut-offs in classifying caseness even among studies that used the same tools and the set objectives of these studies, to either screen or establish a clinical diagnosis for psychological morbidity, in the population being studied.16
The significant risk factors for psychological morbidity reported by our study can be broadly categorized under academic factors including peer pressure for academic performance and lack of extracurricular activities and, health-related factors such as unable to cope with pubertal changes, perceived body image, substance abuse, sleep disturbances and perceived psychological stress. In line with our findings, studies from Gujarat and Goa have reported factors such as facing difficulties with education, abnormal sleep patterns, history of physical or verbal abuse and substance abuse to be associated with psychological morbidity in adolescents.4,17,18 Considering the profile of risk factors identified in this study as well as from other Indian studies, we can infer that there is an interplay of academic and health-related factors in determining mental wellness in adolescents. Thus, strategies for risk prevention and mental health promotion should be incorporated both at school as well as the family level to bring about a decrease in mental morbidity.5,19
Although there is limited evidence to establish the positive effect of mental health promotive interventions in adolescents from Indian settings, studies from high-income settings have shown that incorporating life skills education in the school curriculum is effective in reducing mental morbidity.5 A life skills approach comprising of physical activity, stress management techniques, interpersonal skills and effective communication can mitigate the risk factors noted in our study such as lack of extracurricular activity, perceived psychological stress and difficulty to cope with pubertal changes.5,19 In addition, a supportive family environment provides a window of opportunity for adolescents to discuss health-related and sensitive issues.5 Complementary to these initiatives at the school and family level for promoting adolescent mental health, there is a need to strengthen the existing adolescent-friendly clinics under ‘Rashtriya Kishore Swasthya Karyakram’, a Government of India initiative to address diverse issues on adolescent health and well-being.20
The strengths of this study are a larger sample size, the use of validated instruments such as GHQ and PSS, which have been widely used across Indian settings and having these questionnaires self-administered by participants, thereby avoiding social desirability while responding. The potential limitation with this study would be establishing causality of risk factors to psychological morbidity, as the ascertainment of risk factors and the outcome was made at the same time point.
Conclusions
Our study estimated that one-fourth of school-going adolescents in urban Puducherry suffered psychological morbidity. Factors related to academics and health were attributable to the considerable burden of psychological morbidity in school-going adolescents. This study highlights the need to address these issues through the provision of a supportive school environment and adolescent-friendly health initiatives to reduce the psychological disease burden.
Conflicts of interest
None declared
References
- Mental health of young people: A global public-health challenge. Lancet. 2007;369:1302-13.
- [CrossRef] [Google Scholar]
- Our future: A Lancet Commission on Adolescent Health and Wellbeing. Lancet. 2016;387:2423-78.
- [CrossRef] [Google Scholar]
- The burden of mental disorders across the states of India: The Global Burden of Disease Study 1990-2017. Lancet Psychiatry. 2020;7:148-61.
- [Google Scholar]
- Abuse and other correlates of common mental disorders in youth: A cross-sectional study in Goa, India. Soc Psychiatry Psychiatr Epidemiol. 2013;48:515-23.
- [CrossRef] [PubMed] [Google Scholar]
- Promoting child and adolescent mental health in low and middle income countries. J Child Psychol Psychiatry. 2008;49:313-34.
- [CrossRef] [PubMed] [Google Scholar]
- School, peer and family relationships and adolescent substance use, subjective wellbeing and mental health symptoms in Wales: A cross sectional study. Child Indic Res. 2018;11:1951-65.
- [CrossRef] [PubMed] [Google Scholar]
- Detecting common mental disorders in primary care in India: A comparison of five screening questionnaires. Psychol Med. 2008;38:221-8.
- [CrossRef] [PubMed] [Google Scholar]
- The validation of the Tamil version of the 12 item general health questionnaire. Indian J Psychiatry. 1999;41:217-21.
- [Google Scholar]
- Violence, psychological distress and the risk of suicidal behaviour in young people in India. Int J Epidemiol. 2009;38:459-69.
- [CrossRef] [PubMed] [Google Scholar]
- A global measure of perceived stress. J Health Soc Behav. 1983;24:385-96.
- [CrossRef] [PubMed] [Google Scholar]
- Perceived stress, sources and severity of stress among medical undergraduates in a Pakistani medical school. BMC Med Educ. 2010;10:2.
- [CrossRef] [PubMed] [Google Scholar]
- Perceived stress and its epidemiological and behavioral correlates in an urban area of Delhi, India: A community-based cross-sectional study. Indian J Psychol Med. 2020;42:80-6.
- [CrossRef] [PubMed] [Google Scholar]
- Perceived stress, life events & coping among higher secondary students of Hyderabad, India: A pilot study. Indian J Med Res. 2011;134:61-8.
- [Google Scholar]
- Common mental disorders prevalence in adolescents: A systematic review and meta-analyses. PLoS One. 2020;15:e0232007.
- [CrossRef] [PubMed] [Google Scholar]
- National Mental Health Survey of India 2015-2016. Indian J Psychiatry. 2017;59:21-6.
- [CrossRef] [PubMed] [Google Scholar]
- Depression in children and adolescents: A review of Indian studies. Indian J Psychol Med. 2019;41:216-27.
- [CrossRef] [PubMed] [Google Scholar]
- Non-traditional lifestyles and prevalence of mental disorders in adolescents in Goa, India. Br J Psychiatry. 2008;192:45-51.
- [CrossRef] [PubMed] [Google Scholar]
- Screening for common mental health problems and their determinants among school-going adolescent girls in Gujarat, India. J Fam Med Prim Care. 2020;9:264-70.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment and prevention of mental disorders in low-income and middle-income countries. Lancet. 2007;370:991-1005.
- [CrossRef] [Google Scholar]
- National Health Mission. Available at https://nhm.gov.in/index1.php?lang=1&level=3&sublinkid=1247&lid=421 (accessed on 21 Nov, 2020)
- [Google Scholar]




