Translate this page into:
Public health challenges for the 21st century: Convergence of demography, economics, environment and biology: Nalanda distinguished lecture
Corresponding Author:
K M Venkat Narayan
1518 Clifton Road NE, CNR Room 7043, Atlanta, GA 30329
USA
knaraya@emory.edu
| How to cite this article: Narayan K M. Public health challenges for the 21st century: Convergence of demography, economics, environment and biology: Nalanda distinguished lecture. Natl Med J India 2017;30:219-223 |
Abstract
The rapidly changing and interdependent world under the mega-force of globalization presents unique challenges and opportunities for public health. Focusing on the example of type 2 diabetes, I argue that an appreciation for the evolution of demographic and economic contexts is essential to appropriately address today's dynamic and complex health challenges.
For the vast majority of the past 2000 years, India and China were the world's largest economies until the rise of western European nations in the 18th century and later the USA. In the case of India, inflation-adjusted per capita income remained flat between 1700 and 1950, while in the same period that of the UK grew more than 7-fold, although the population of the UK relatively grew 3-times faster than that of India in the same period. This 250-year gap in industrial and economic development may be central to understanding the large burden of diabetes among individuals of Indian descent, and should be taken into account in a wider context to understand the divergence in health development between India and parts of the world which benefited from early industrial progress and accompanying improvements in food supply, hygiene and living conditions.
Lessons from high-income countries support a strong emphasis on public health to achieve important populationwide health gains, and offer insights into the broader determinants of health such as economic and food security, equity, urban infrastructure, health-promoting environments, and access to high-quality health systems. Critical to contemporary public health is also strong data systems and evidence-based decision-making.
Introduction
Globalization has always been part of humanity. Until about 70 000 years ago human beings inhabited only Africa. It was around that time that a small number of our ancestors, according to genetic and paleontological data, started to leave Africa, probably to escape from the Ice Age that had set on that continent.[1],[2],[3],[4] A small group migrated along the coast to Southern India and some reached as far as Australia. Slightly later, a second group appears to have migrated by land to head to the Middle East and southern Central Asia. These two migrations have since expanded and populated our entire planet. And so on it goes, and we continue as a global family, always migrating, meeting, mixing, interacting and expanding. Although globalization is nothing new, there are several differences today that introduce considerable complexity in ways our ancestors never experienced, and this introduces new challenges to how we might conceptualize and address global health. The rate of social, cultural, economic, political and environmental change now is unprecedented, driven largely by wireless connectivity, television, radio, social media, modern travel and migration. News travels rapidly today, and all events anywhere are instantly visible everywhere. Furthermore, we are faced with an exponential growth of information, with doubling time of about two years or less,[5],[6] and as I argue below, history is forcing us to recognize our interdependence, and also to acknowledge that our strongest force for change is information and knowledge.
It is the context of today's knowledge-driven global world that makes Nalanda so important. This venerable global centre of learning and education started as a Buddhist monastery during the lifetime of the Buddha in the 6th century BC. It slowly evolved into a full-fledged residential university by the 5th and 6th century AD, funded by public finances, flourishing as an international centre of higher learning, boasting 10 000 students and 2000 faculty from over 90 countries at its peak before being destroyed in the 1190s.[7],[8],[9] At the time Nalanda fell, after reigning for 800 years, Bologna University, the oldest in Europe, and Oxford University had just about started, and Cambridge University had not even opened. Now, thanks to the efforts of people like Late President Abdul Kalam, Nobel Laureate Amartya Sen, former Finance Minister of Singapore George Yeo, and to the vision and support of the Government of India and collaboration from nine east Asian countries, a modern Nalanda University has been started close to the ruins of the prior ancient centre of learning.
Shantarakshita, the Abbot of the ancient Nalanda University in the 8th century, said: ‘Always investigate, always argue, always reason.‘ This simple but profound idea is increasingly relevant to the complex world of today and of the future, which is what makes the revival of Nalanda so pertinent. Reflecting on Shantarakshita's words and the revival of the 2000-year-old world centre of learning allows me the unique pleasure and privilege to take stock of how economics, demography, environment and biology have interacted over 2000 years, and what that might foretell for public health priorities for the next, say 30 or 50 years.
Economy and demography set the context
Economy and demography are powerful influences, and shape the environment in which we live, and thus structure population and individual health. For most of the past 2000 years, and right until the 18th century, India and China were the world's largest economies.[10],[11],[12] Even until 1750, India contributed to nearly a quarter of the world's economy, then under colonial rule and missing the fruits of the industrial revolution, India's contribution declined to as low as 3.8% by 1950 when the modern Indian republic was founded.[10],[13]
Starting at comparable levels, the inflation-adjusted per capita income in the UK grew more than 7-fold between 1700 and 1950, coinciding with East India Company and British colonial rule of India, while the per capita income of India stayed almost flat [Figure - 1].[10],[13],[14] Interestingly, during this period, the populations of UK grew relatively three times as fast as that of India; the population ratio of UK to India was 5.2:100 in 1700 AD and 14:100 in 1950 AD. Therefore, in relative terms the total gross domestic product (GDP) of UK grew more than 21 times while that of India's stayed flat during those 250 years. These data contradict the oft-held notion that India became poor due to its population explosion, as UK was able to grow its per capita income 7-fold, compared to India, despite its population growing three times as fast in the same period.
 |
| Figure 1: Economy and demography of India and UK, 1700–1950 (reproduced from references 10, 13 and 14) GDP gross domestic product |
India was not alone in this unfortunate experience. Except for a handful of countries (mainly nations of western Europe, north America and Australasia), the vast majority of the world was not only left out from the industrial revolution but also subject to resource depletion that fuelled economic development elsewhere. A huge gap in economy and standard of living thus resulted over 250 years between the few countries that enjoyed the benefits of the industrial revolution from the vast majority that did not. The gap between the world's poorest and richest country in 1700 was about 1 in 3 or 1 in 4, but now approaches 1 in 400.[15] Therefore, any understanding of lifestyle or health status differences today between, say a high-income country such as the UK, and a low- and middle-income country (LMIC) such as India, cannot ignore the numerous confounding factors introduced by this 250-year period that dramatically separated the two populations in terms of economic development.
These differential economic development patterns are intimately linked with the tale of population growth and health globally. The population of human beings on this planet has been rather small for the overwhelming part of human history. Human population on earth reached its first billion only in around 1800, and the second billion in the early part of the 20th century, and has since grown rapidly, reaching 7 billion people in 2011.[16],[17] Industrialization, and accompanying improvements in food production and distribution, sanitation and hygiene have been major players in reducing mortality rates and extending life expectancy. Thomas McKeown in his classic work analysed the reduction in mortality rates in England and Wales in the 19th century, showing the decline in mortality rates from six major infectious diseases between 1770 and 1900.[18],[19] He concluded that the population growth and improved health in England and Wales in that period was overwhelmingly due to improved food production and nutrition, and due to environmental factors. Much of the decline antedated major medical breakthroughs (e.g. immunization, antibiotics), allowing McKeown to also conclude that the role of medicine in improving the health of the population of England and Wales in the 19th century, when that country was also rapidly growing industrially and economically, was negligible.[19]
The majority of the world, including India, did not benefit from the kind of improvements in health in the 19th and early 20th centuries seen in countries such as the UK, other parts of western Europe and north America, as they had missed out on the exponential economic development ushered in by the industrial revolution, and thus also the accompanying improvements in food production, nutrition, sanitation and hygiene. For example, during the time of the industrial revolution, economic growth in India was virtually stagnant.
Even in the post-independence period from 1950 to the late 1980s, India's total GDP grew very slowly, remaining almost flat during the first three decades, while the population more than doubled from around 360 million in 1950 to 780 million in 1985.[14],[20] India has, however, experienced rapid growth of its economy since the 1990s, when market liberalization began. Compared with the period before liberalization, India's GDP has expanded at a considerable pace, with per capita GDP (PPP) growing from US$ 1275 in 1985 to US$ 6746 in 2015. Currently, India is the fastest growing large economy in the world, and several projections indicate that India may emerge as the world's third largest economy, behind China and the USA, by around 2030, and continue to grow at a robust pace for the most part of this century.[21],[22],[23] There is also a major and growing shift in the size of the sectors contributing to India's economy: services have grown from contributing 30% to the economy in 1950 to 59% in 2012, while agriculture has declined from 50% in 1950 to 14% in 2012.[14]
With these modern economic changes, the picture with respect to health has also changed in India and elsewhere. In the past 50 years, life expectancy has been growing in all but a few of the world's countries, and countries that lagged behind have been gaining life expectancy at a much faster rate than happened in today's high-income countries in the 19th and early 20th century. For example, while life expectancy has grown in the USA from 68.9 years in 1950 to a projected 81.2 years in 2030 (+12.3 years), India's will have grown from 37.4 years to 72.6 years (+25.2 years) in the same period.[24] This pattern of rapid recent improvement in life expectancy is also true for the majority of LMICs, coinciding with the active economic growth and development witnessed in many of these countries.
Changing pattern of health
The past two decades have witnessed major declines in childhood and maternal mortality, and in deaths from infectious diseases, especially in LMICs.[25],[26],[27],[28] This has meant a major change in pattern of disease, with shift away from communicable disease risks in children toward non-communicable disease (NCD) risks in adults.[26],[29] For example, while in 1990, the leading causes of death worldwide, including India, was largely dominated by communicable diseases and under-nutrition, by 2010, the leading causes of death are from NCDs (e.g. ischaemic heart disease, stroke, chronic obstructive pulmonary disease, cancers, diabetes). Yet many LMICs, including India, also have an unfinished agenda of under-nutrition, child and maternal mortality and communicable diseases, and have the daunting challenge of dealing with the ‘dual burdens’ (under-nutrition and overweight/obesity, communicable diseases and NCDs coexisting in large numbers).
With NCDs now as the leading cause of death across the world, six of the top ten risk factors for mortality worldwide are cardio-metabolic risk factors (high blood pressure, tobacco use, high blood glucose, physical inactivity, overweight and obesity, high cholesterol), and are related to lifestyles and behaviours associated with economic development;[30] these risk factors along with unhealthy diet, excess alcohol and substance use, are also the leading cause of disability, as measured by disability-adjusted life years (DALYs).[31] With advancing economic development, there is a convergence between causes of death in high- and low-income countries In addition to causing premature deaths, NCDs also impact quality of life and economics.[32] NCDs disproportionately strike young people in LMICs and consequently adversely impact the workforce and the country's economic potential. By virtue of being chronic, most NCDs are lifelong and are costly for the individual and society to treat. The World Economic Forum considers NCDs among the highest likely risks and most severe for global economic development, and therefore, need to be prevented and controlled.[30]
Interaction of Economics, Demography, Environment and Biology
The example of type 2 diabetes in India and other LMICs
As a prototypical NCD, type 2 diabetes offers a contemporary example of a major global health threat that emerged alongside modern globalization and is very much at the intersection of economics, demography, environment and biology. Moreover, type 2 diabetes also offers a sobering example of how disease patterns and presentations may vary across the world due to historical differences in the timing and intensity of industrial and post-industrial economic development. For example, the pattern and presentations of type 2 diabetes in LMICs, which missed major industrialization and economic development for two centuries or more, may be different than that established in the high-income countries that benefited from industrialization in this historical time period.[33],[34]
While the unprecedented increase in diabetes globally is new, the disease itself is not new, and has been described in ancient times by the Greeks, the Romans, the Arabs and Indians. For example, the 6th century Ayurveda textbook, Charaka Samhita, had this to say: ‘There are two forms of diabetes (Madhu Meha); one associated with emaciation, dehydration, polyuria and lassitude, and the other with stout build, gluttony, obesity and sleepiness.’[35] There are, at least, 25 words in the Sanskrit language associated with diabetes.[36] This indicates that the disease was present many centuries ago, albeit rarely and possibly affecting only some groups. What brought the modern epidemic of type 2 diabetes to the forefront of public health research was the sudden explosion of the disease in the second half of the 20th century in Pima Indians of Arizona. The Pima Indians comprise one of the pre-Columbian migrations to the Americas, probably from Central Asia, about 35 000 years ago.[37],[38],[39] A group of them had settled on the banks of the Gila river, and had a small but stable agricultural economy. The Pimas had a physically active lifestyle and largely ate traditional foods, and there is documented evidence supporting that there was very little diabetes in the population right until 1937. Data from a survey of the Pima population in Arizona in the early 1960s, however, shocked the world when it was found that 50% of them had diabetes by 45 years of age, and that all of the diabetes in Pimas was what we today call type 2.[40] Furthermore, the population had become very obese, and children as young as 7 years were developing type 2 diabetes.[41] It is believed that the driving factor for the growth of diabetes in the Pimas was the change in the environment and in the Pima way of life brought on by the building of the Roosevelt dam, which dried up local agriculture. The end of indigenous agriculture, in turn, caused the population to become physically inactive and reliant on federally subsidized modern foods from the neighbouring metropolis of Phoenix.
Little did the world suspect that what was happening in the Pima Indians was a forecast of what would happen the world over in the next 50–70 years with modernization and industrialization spreading, and universally changing the environment and traditional ways of life in agrarian communities. Over the past few decades, the majority of countries across the world have seen increases in average population body mass index (BMI), a rise in obesity, and alongside this, also increases in average population glucose levels and a rise in type 2 diabetes.[42] This increase in type 2 diabetes is now universal and affects all countries of the world, regardless of income level, and affects urban and rural parts, rich and poor. By current estimates, there are 387 million people with diabetes worldwide, and by conservative projections, there will be an additional 205 million affected by 2035.[43]
While all regions of the world are affected, the Indian subcontinent has a disproportionate and rapidly growing diabetes burden, and people living in or from this region of the world have an especially heightened risk, often at younger ages and at lower BMIs.[44],[45],[46] There has been a phenomenal rise in diabetes in India and other South Asian countries during the past decades. In the city of Chennai in South India, for example, the population prevalence (proportion of people with diabetes) has grown from 2.3% in 1971 to 14.1% in 2004, and 22.8% in 2015.[47],[48],[49],[50],[51]
Furthermore, migrants from the Indian subcontinent have the highest diabetes prevalence among all migrant ethnic groups in the USA, and even normal weight migrants from the Indian subcontinent have as high or higher diabetes prevalence than obese migrants from Europe.[44] Recent data indicate the prevalence of type 2 diabetes even in underweight residents of Chennai is strikingly high. Comparison studies between Chennai Indians and Pima Indians indicate that by 55 years of age, the prevalence of diabetes is 50% in both groups, but the Pima Indians are relatively far more obese and insulin-resistant, while the Chennai Indians experience diabetes risk even at lower BMIs and may have relatively lower insulin secretion to begin with.[33]
The high risk of diabetes in Indians, and the differences in the pattern of type 2 diabetes presentation (i.e. occurring even in thin people, and possibly related to poor insulin secretion in addition to a propensity to insulin resistance) may have to do with historical differences in terms of differential timing in the introduction of modernization and industrialization, and biological adaptation to the centuries of maternal and childhood under-nutrition that the populations of the Indian subcontinent have been exposed to. Several investigations, including the New Delhi Birth Cohort Study, support the idea that poor early nutrition increases fat deposition, poor insulin secretion and heightened risk of diabetes in later life.[52],[53] This becomes important in the context of the Indian subcontinent, where levels of nutrition, especially maternal and childhood, which were perhaps among the best in the Mesolithic period,[54] have since been increasingly poor for centuries, and now the environment and lifestyles are changing rapidly to promote physical inactivity and processed foods, high in refined carbohydrates and saturated fats, and low in protein, creating a toxic diabetogenic situation.
While biological susceptibility probably conferred by adaptation to thrifty nutrition for centuries may set the context to diabetes and other NCD risk, the drivers of modern shifts in lifestyle towards physical inactivity and poor diet are important to address. These operate at several levels: (i) globalization and trade policies favour production and consumption of processed unhealthy calorie-dense foods, increased food diversity, a proliferation of unhealthy locally made fast foods, sweetened beverages, alcohol and tobacco, while costs of healthy foods (fruits and vegetables, high-fibre breads, monosaturated fats, proteins) are prohibitive; (ii) national and regional subsidies preferentially support refined carbohydrates, notably polished white rice; (iii) popular culture combined with modern technology promotes sedentary behaviours (e.g. television watching, computer games); (iv) traditional cultural norms favour consumption of fried and refried foods, unhealthy amounts of salt added to cooking; (v) unplanned urban development inhibits physical activity, contributes to air pollution and to major stresses in daily living.
Reflections on public health achievements and looming priorities ahead
When one examines the major gains in health of populations and of individuals in industrialized countries in the 19th and 20th centuries, the major drivers have been improvements in economy (both national and per capita) and accompanying better nutrition and hygiene, and healthier living environments. The Centers for Disease Control and Prevention (CDC) identified 10 major 20th century public health achievements [Table - 1],[55] and most of these have been driven by policies and organized efforts to improve nutrition, reduce exposure to unsafe products and environments, and effective delivery of high-quality preventive care (e.g. immunization, control of cardiovascular risk factors).
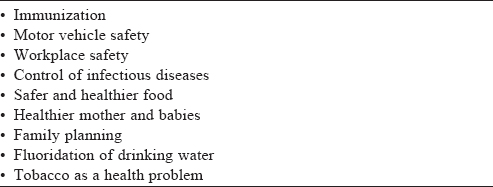
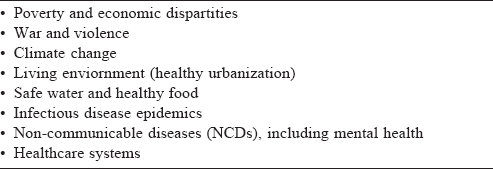
Many of these public health successes in industrialized countries can be replicated in LMICs like India, and even speeded up, given the right conditions—e.g. good policies and governance, good public health infrastructure and active community involvement— as was seen with the eradication of smallpox and now the elimination of polio, and the major improvements in maternal and child health in the past few decades. Yet, as LMICs like India try to bridge and leapfrog the 250-year industrial gap, and the major gaps in health status that have resulted from it, many contemporary challenges at a broad level need to be addressed [Table - 2]. Foremost among these are attention to poverty and economic security, peace, climate change and healthy environment, planned urban infrastructure, safe water and food security, dealing with the dual challenges of infectious and non-communicable diseases, and health systems. All of these are complex interconnected issues needing strong global cooperation and committed local action, as in an interdependent world, global and local are two sides of the same coin. Some examples of such global collaboration are evident—notably, the global fight against HIV, the efforts to reduce child mortality and, more recently, the Paris accord on climate change.
The biggest drivers of change in today's fast-paced and interconnected global world are high-quality information (in terms of disease burdens, risk, distribution, causes and evidence on effective interventions) and the spread of it through networking to implement evidence-based programmes in scale and rapidly. Yet, the current picture suggests that the regions of the world with the biggest disease burdens have scant investments in information and research, and often borrow knowledge from studies conducted in high-income countries.[33] This may not always work, as disease patterns, response to prevention and treatment, and nuances of clinical and public health policy may vary, depending on historical and current socioeconomic contexts.
Conclusion
Health is very much a product of the interaction between biology and the environment, and the larger context of public health is set by major societal factors, notably economics and demography. Public health has delivered major, often unsung, benefits over the past two centuries, especially in high-income countries, and is now very much at the intersection of many of the issues confronting a globalizing world—trade and economics, environment, poverty, human rights and health. Inherent to public health is its interdisciplinary orientation, and the need for a perspective beyond medicine, encompassing all factors that nurture a healthy environment.
Acknowledgements
I thank the leadership of Nalanda University for inviting me to give a Nalanda Distinguished Lecture, and my colleagues, Shivani Patel and Rebecca Jones for their critical inputs to this manuscript.
| 1. | Gugliotta G. The great human migration: Why humans left their African homeland 80,000 years ago to colonize the world. Smithsonian Magazine July 2008. Available at www.smithsonianmag.com/history/the-great-human-migration-13561/?all (accessed on 25 Feb 2017). [Google Scholar] |
| 2. | Before the exodus. The Economist 24 Apr 2008. Available at www.economist.com/ node/11088535 (accessed on 25 Feb 2017). [Google Scholar] |
| 3. | Culotta E, Gibbons A. Almost all living people outside of Africa trace back to a single migration more than 50,000 years ago. Science: Archaeology, Asia/Pacific, Evolution, Social Sciences, Human Evolution 21 Sept 2016. Available at www.sciencemag. org/news/2016/09/almost-all-living-people-outside-a2frica-trace-back-single-migration-more-50000-years (accessed on 25 Feb 2017). [Google Scholar] |
| 4. | The Genographic Project. Map of human migration. National Geographic [updated in 2016]. Available at https://genographic.nationalgeographic.com/human-journey/ (accessed on 25 Feb 2017) [Google Scholar] |
| 5. | Schilling DR. Knowledge doubling every 12 months, soon to be every 12 hours. Industry tap into news, 19 April 2013. Available at www.industrytap.com/knowledge-doubling-every-12-months-soon-to-be-every-12-hours/3950 (accessed on 25 Feb 2017). [Google Scholar] |
| 6. | Densen P. Challenges and opportunities facing medical education. Trans Am Clin Climatol Assoc 2011;122:48-58. [Google Scholar] |
| 7. | Nâlandâ University. History and revival. Available at www.nalandauniv.edu.in/ about-nalanda/history-and-revival/ (accessed on 25 Feb 2017). [Google Scholar] |
| 8. | Garten JE. Really old school. The New York Times, Section: The opinion pages, 9 December 2006. Available at www.nytimes.com/2006/12/09/opinion/09garten.html (accessed on 25 Feb 2017). [Google Scholar] |
| 9. | Najar N. Indians plan rebirth for 5th-century university. The New York Times, Section: The chronicle of higher education, 23 Mar 2014. Available at www. nytimes. com/2014/03/24/world/asia/indians-plan-rebirth-for-5th-century-university.html?mcubz=3 (accessed on 20 Sep 2017) [Google Scholar] |
| 10. | Maddison A. The world economy: A millennial perspective. Paris:Organisation for Economic Co-operation and Development (OECD); 2001:384 pp. [Google Scholar] |
| 11. | Maddison A. Contours of the world economy, I—2030 AD: Essays in macro-economic history. Oxford: Oxford University Press; 2007. Available at www.ggdc.net/ maddison/oriindex.htm (accessed on 25 Feb 2017). [Google Scholar] |
| 12. | Cowen T. Lesson from old India: When an economy just doesn’t get better. Section: Economic view. The New York Times 22 Aug 2014. Available at https:// www.nytimes.com/2014/08/24/upshot/lesson-from-old-india-when-an-economy-just-doesnt-get-better.html?mcubz=3 (accessed on 25 Feb 2017). [Google Scholar] |
| 13. | Dharma K, Desai M (ed). The Cambridge economic history of India, Volume II: c.1757–1970. Cambridge:Cambridge University Press; 1983. [Google Scholar] |
| 14. | Wikipedia. Economy of India. Available at https://en.wikipedia.org/wiki/ Economy_of_India (accessed on 25 Feb 2017). [Google Scholar] |
| 15. | Piketty T, Zucman G. Capital is back: Wealth-income ratios in rich countries 1700– 2010. Washington, DC:Center for Economic and Policy Research (CEPR); 2013. [Google Scholar] |
| 16. | World population: Historical estimates of world. Washington, D.C.:United States Census Bureau; 2017. Available at www.census.gov/population/international/data/ worldpop/table_history.php (accessed on 25 Feb 2017). [Google Scholar] |
| 17. | Manning S. Year-by-year world population estimates: 10,000 BC to 2007 AD. Historian on the warpath, 12 Jan 2008. Available at www.scottmanning.com/ content/year-by-year-world-population-estimates/ (accessed on 25 Feb 2017) [Google Scholar] |
| 18. | McKeown T. The modern rise of population. New York:Academic Press; 1976. [Google Scholar] |
| 19. | McKeown T. The role of medicine:Dream, mirage, or nemesis? Princeton:Princeton Legacy Library; 1980. [Google Scholar] |
| 20. | Wikipedia. Demographics of India. Available at https://en.wikipedia.org/wiki/ Demographics_of_India (accessed on 25 Feb 2017). [Google Scholar] |
| 21. | PwC. The world in 2050: Will the shift in global economic power continue? Available at https://www.pwc.com/gx/en/issues/the-economy/assets/world-in-2050-february-2015.pdf (accessed on 20 Sep 2017). [Google Scholar] |
| 22. | Wilson D, Purushothaman R. Dreaming with BRICS: The path to 2050. In: G S Global Economics Website Economic Research from the G S Finance Workbench. Global economics, Paper no 99: Goldman Sachs; 2003. Available at www.goldmansachs.com/our-thinking/archive/brics-dream.html (accessed on 25 Feb 2017). [Google Scholar] |
| 23. | The Guardian. Developing economies to eclipse west by 2060, OECD forecasts [updated in 2012]. Available at www.theguardian.com/global-development/datablog/ 2012/nov/09/developing-economies-overtake-west-2050-oecd-forecasts (accessed on 25 Feb 2017). [Google Scholar] |
| 24. | United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2006 Revision, Highlights, Working Paper No. ESA/P/WP.202. New York:United Nations; 2007. Available at www.un.org/esa/ population/publications/wpp2006/WPP2006_Highlights_rev.pdf (accessed on 25 Feb 2017). [Google Scholar] |
| 25. | Hogan MC, Foreman KJ, Naghabi M, Ahn SY, Wang M, Makela SM, et al. Maternal mortality for 181 countries, 1980–2008 : A systematic analysis of progress towards Millennium Development Goal 5. Lancet 2010;375:1609-23. [Google Scholar] |
| 26. | GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117-71. [Google Scholar] |
| 27. | You D, Hug L, Ejdemyr S, Idele P, Hogan D, Mathers C, et al. United Nations Inter-agency Group for Child Mortality Estimation (UN IGME). Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: A systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. Lancet 2015;386:2275-86. [Google Scholar] |
| 28. | Byass P. Child mortality is (estimated to be) falling. Lancet 2016;388:2965-67. [Google Scholar] |
| 29. | Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006;3:e442. [Google Scholar] |
| 30. | Narayan KMV, Ali MK, Koplan JP. Global noncommunicable diseases: Where worlds meet. N Engl J Med 2010;363:1196-8. [Google Scholar] |
| 31. | GBD 2013 DALYs and HALE collaborators. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: Quantifying the epidemiological transition. Lancet 2015;386:2145-91. [Google Scholar] |
| 32. | Bloom DE, Cafiero ET, Jané-Llopis E, Abrahams-Gessel S, Bloom LR, Fathima S, et al. The global economic burden of noncommunicable diseases. Geneva:World Economic Forum; 2011. [Google Scholar] |
| 33. | Narayan KM. Type 2 diabetes: Why we are winning the battle but losing the war? 2015 Kelly West Award Lecture. Diabetes Care 2016;39:653-63. [Google Scholar] |
| 34. | Narayan KMV. The mysteries of type 2 diabetes in developing countries. Bull World Health Organ 2016;94:233-308. [Google Scholar] |
| 35. | McFarlane I, Bliss M, Jackson J, Williams G. Diabetes in its historical and social context. In: Pickup JC, Williams G (eds). Textbook of diabetes. 2nd ed. Victoria, Australia:Blackwell Scientific; 1997. [Google Scholar] |
| 36. | Weaver LJ, Narayan KMV. Reconsidering the history of type 2 diabetes in India: Emerging or re-emerging disease? Natl Med J India 2008;21:288-91. [Google Scholar] |
| 37. | Knowler WC, Pettitt DJ, Saad MF, Bennett PH. Diabetes mellitus in the Pima Indians: Incidence, risk factors and pathogenesis. Diabetes Metab Rev 1990;6:1-27. [Google Scholar] |
| 38. | Narayan KMV. Diabetes in Native Americans: The problems and its implications. In: National Research Council (US) Committee on Population; Sandefur G, Rindfuss RR, Cohen B (eds). Changing numbers, changing needs: American Indian demography and public health. Washington DC :National Academies Press; 1996:262-88. [Google Scholar] |
| 39. | Narayan KMV. Diabetes in Native Americans: The problems and its implications. Population Health Policy Res 1997;16:169-92. [Google Scholar] |
| 40. | Bennett PH, Burch TA, Miller M. Diabetes mellitus in American (Pima) Indians. Lancet 1971;2:125-8. [Google Scholar] |
| 41. | Savage PJ, Bennett PH, Senter RG, Miller M. High prevalence of diabetes in young Pima Indians: Evidence of phenotypic variation in a genetically isolated population. Diabetes 1979;28:937-42. [Google Scholar] |
| 42. | Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al.; for the Global Burden of Metabolic Risk Factor of Chronic Diseases Collaborating Group (Body Mass Index). National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 2011;377: 557-67. [Google Scholar] |
| 43. | International Diabetes Federation. IDF Diabetes Atlas. 7th ed. Brussells:IDF; 2015. [Google Scholar] |
| 44. | Oza-Frank R, Narayan KM. Overweight and diabetes prevalence among US immigrants. Am J Public Health 2010;100: 661-8. [Google Scholar] |
| 45. | Gujral UP, Pradeepa R, Weber MB, Narayan KM, Mohan V. Type 2 diabetes in South Asians: Similarities and differences with white Caucasian and other populations. Ann NY Acad Sci 2013;1281:51-63. [Google Scholar] |
| 46. | Staimez LR, Weber MB, Narayan KM, Oza-Frank R. A systematic review of overweight, obesity, and type 2 diabetes among Asian American subgroups. Curr Diabetes Rev 2013;9:312-31. [Google Scholar] |
| 47. | Ramachandran A, Snehalatha C, Dharmaraj D, Viswanathan M. Prevalence of glucose intolerance in Asian Indians. Urban–rural difference and significance of upper body adiposity. Diabetes Care 1992;15:1348-55. [Google Scholar] |
| 48. | Ramachandran A, Snehalatha C, Latha E, Vijay V, Mohan V. Rising prevalence of NIDDM in an urban population in India. Diabetologia 1997;40:232-7. [Google Scholar] |
| 49. | Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al.; Diabetes Epidemiological Study Group in India (DESI). High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia 2001;44:1094-101. [Google Scholar] |
| 50. | Mohan V, Deepa M, Deepa R, Shanthirani CS, Farooq S, Ganesan A, et al. Secular trends in the prevalence of diabetes and impaired glucose tolerance in urban South India—the Chennai Urban Rural Epidemiology Study (CURES-17). Diabetologia 2006;49:1175-8. [Google Scholar] |
| 51. | Deepa M, Grace M, Binukumar B, Pradeepa R, Roopa S, Khan HM, et al.; CARRS Surveillance Research Group. High burden of prediabetes and diabetes in three large cities in South Asia: The Center for cArdio-metabolic Risk Reduction in South Asia (CARRS) Study. Diabetes Res Clin Pract 2015;110:172-82. [Google Scholar] |
| 52. | Bhargava SK, Sachdev HS, Fall CH, Osmond C, Lakshmy R, Barker DJ, et al. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med 2004;350:865-75. [Google Scholar] |
| 53. | Wells JC, Pomeroy E, Walimbe SR, Popkin BM, Yajnik CS. The elevated susceptibility to diabetes in India: An evolutionary perspective. Front Public Health 2016;4:145. [Google Scholar] |
| 54. | Lukacs JR, Pal JN. Skeletal variation among Mesolithic people of the Ganga plains: New evidence of habitual activity and adaptation to climate. Asian Perspect 2003;42:329-51. [Google Scholar] |
| 55. | Center for Disease Control and Prevention. Ten great public health achievements in the 20th century. 26 April 2013. Available at www.cdc.gov/about/history/tengpha.htm (accessed on 25 Feb 2017). [Google Scholar] |
Fulltext Views
3,584
PDF downloads
437




