Translate this page into:
Respectful maternity care in the achievement of universal health coverage
How to cite this article: ANSARI H, YERAVDEKAR R. Respectful maternity care in the achievement of universal health coverage. Natl Med J India 34:2021;174-76.
Abstract
The attainment of universal health coverage (UHC) is incomplete without achieving respectful maternity care (RMC). While planning for UHC, the need and importance of RMC should be considered. In India, the government has started a health scheme on UHC, namely the Ayushman Bharat Scheme. RMC being an important component of UHC, if not achieved, will result in failure to achieve UHC in the true sense.
INTRODUCTION
The 2030 Agenda for Sustainable Development mentions that all countries should be able to achieve the universal health coverage (UHC) to meet the Sustainable Development Goal (SDG) targets. However, the achievement of UHC without a focus on the quality of care has detrimental rather than beneficial effects.1 UHC includes care for all including childbearing women. Maternal health is an important component of UHC. The White Ribbon Alliance mentions safeguarding the rights of women while providing them with maternal health services. Thus, provision of care is determined by quality and the human rights approach. This is known as respectful maternity care (RMC).2
Every childbearing woman is entitled to RMC. This includes ‘respect for women’s autonomy, empathy, dignity, privacy, confidentiality, choices, feelings and preferences, including companionship during labour and continuous care during labour and childbirth’. A woman should not be subjected to harm or any form of ill treatment.2 This shows that RMC is an essential component of UHC, without which a country cannot state a claim to be achieving UHC.
RESPECTFUL MATERNITY CARE
A necessary condition for UHC
Globally, in developed as well as developing countries, women face disrespect, abuse, lack of privacy, confidentiality, discrimination, neglect and threats. Women, therefore, hesitate to attend health facilities to seek treatment. Fear of embarrassment due to a certain caste, tribe or economic status delays the arrival of women at healthcare facilities. Women do not wish to extend the stay at the facility even if there are complications contributing to maternal mortality and morbidity, highlighting the importance of RMC.2
Studies have shown that healthcare providers insult and humiliate women.3 Passing of sexual remarks, being laughed at and nobody to help and provide care at the hospital make them feel that care at home will be better and more respectful. Focus on institutional delivery has diverted our attention from respectful care. Timely care, an important component of UHC, is not available to women. Demand of informal payments, detainment and not providing services if the payment is not received are barriers to seeking care.3
Women and their families not only face financial stress but also emotional stress. This has an effect on the health of the mother and the newborn. Studies show that lack of respectful care is a healthcare system failure and an important barrier for institutional delivery.3 This also leads to bitter relations between the users and the healthcare providers, having an impact on the capabilities of both the user and provider and thus leading to reduction in confidence and self-esteem. A statement of a focus group discussion done in Uganda among men, ‘poor cannot deliver at the hospital’, points to the fact that RMC is a necessary condition for UHC.4
Maternity care is not limited to labour or childbirth. It starts from the antenatal period and extends to the postnatal period. Lack of RMC at any stage may result in not seeking care at health facilities in the future, negative impact on mother and child and compromise of breastfeeding and immunization. Decision of future deliveries is also dependent on the experience of the mother at the healthcare facility. If women and their families are not confident in the health system, access to care will be limited when it is most essential and likely to be effective. Therefore, woman-centred and context-specific maternity care should be the focus to not only achieve RMC but also UHC and finally the SDGs. Figure 1 shows the consequences of lack of RMC and how the provision of RMC will help in achieving UHC.
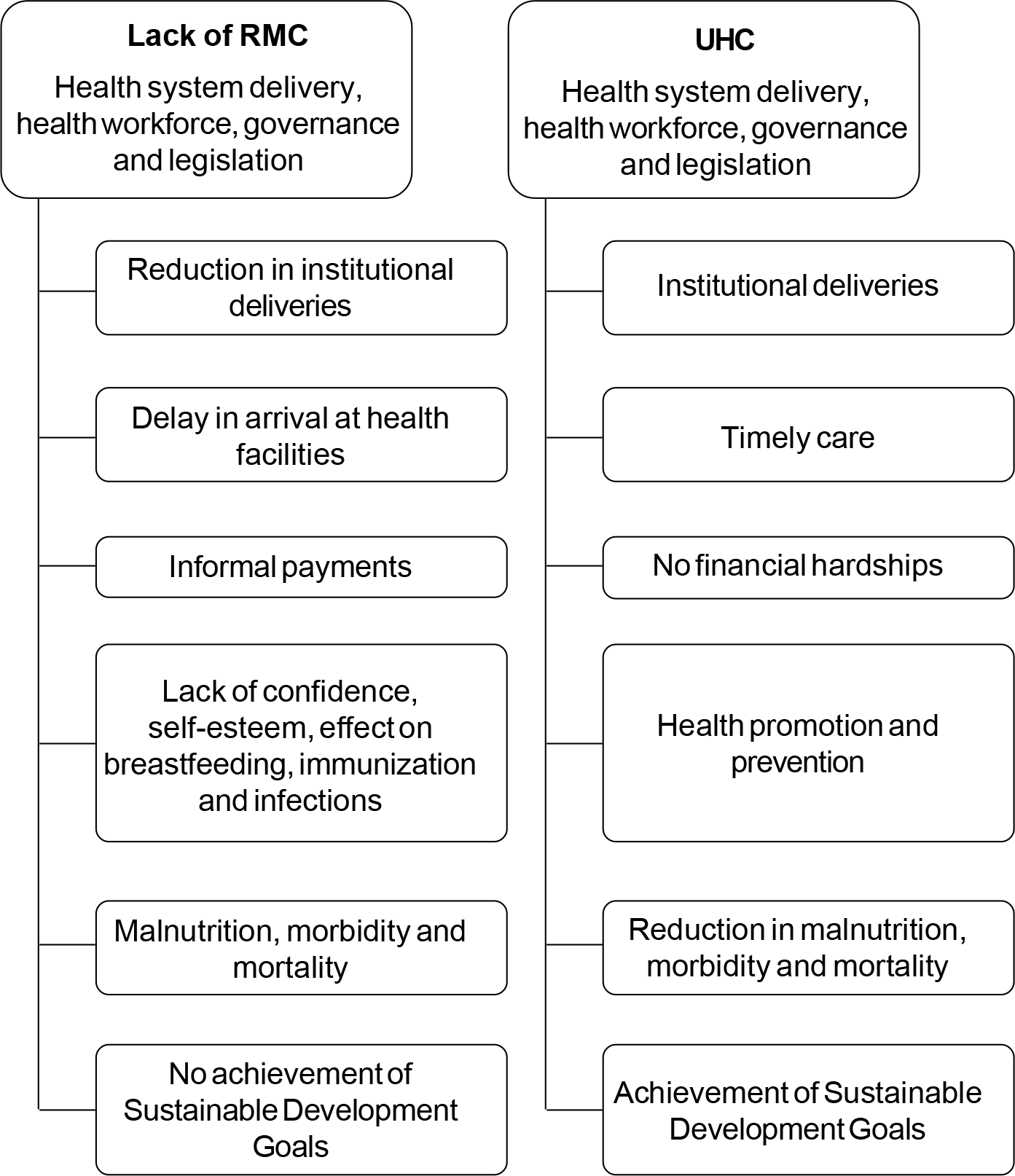
- Respectful maternity care (RMC): A necessary condition for universal health coverage
Integration of UHC and RMC
The WHO document describes the importance of quality of care delivered in UHC.1 UHC is not just related to medical supplies, infrastructure or availability of healthcare providers. It should focus on quality that is person-centred and is based on human rights.
Poor quality results in unmet needs and reluctance/failure to access services at healthcare facilities any time in the future. In addition, resources are wasted and economic and social costs incurred due to an increase in the burden of diseases, thus affecting the health systems and leading to a health system failure. Systems and mechanisms should be in place so that poor quality of care can be reported. RMC is a broad public health goal within the context of UHC. Its achievement will ensure quality services and a successful UHC. Figure 2 shows the central portion focusing on all components of UHC and for each segment, there is an attached component of RMC. Thus, achievement of UHC is incomplete without the achievement of RMC. The SDGs of equity and good health and well-being are possible only when a rights-based approach is included and implemented in UHC. The Lancet Maternal Health series mentions services provided to mothers that are: ‘Too much, too soon, or too little and too late.’5 This again shows that quality that is timely, safe and evidence-based is important in delivering care. Many countries have adopted various programmes for achieving UHC.6 In India, the scheme for achievement of UHC is the Ayushman Bharat Scheme.
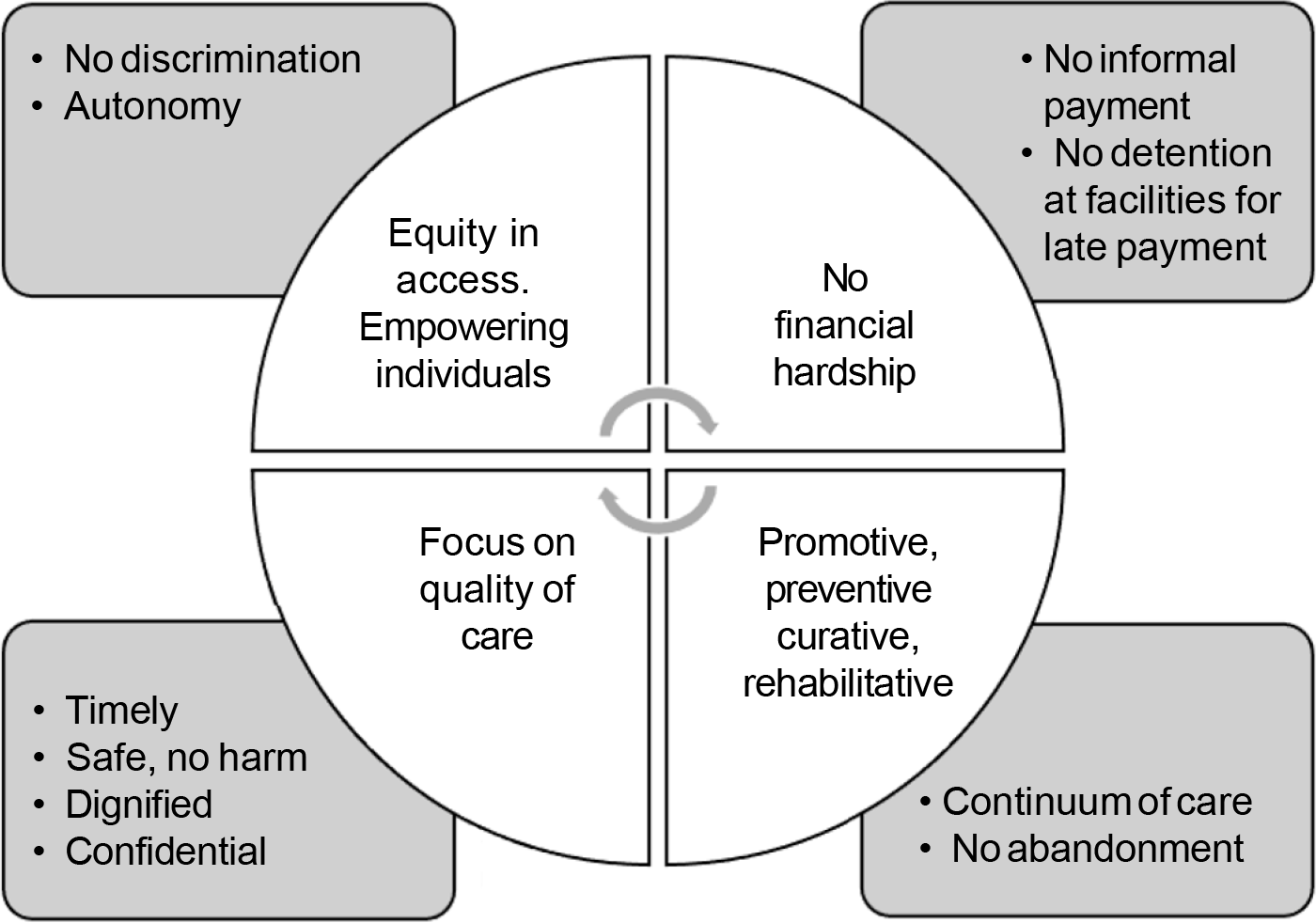
- The link between the components of universal health coverage (centre) with respectful maternity care
AYUSHMAN BHARAT SCHEME
In India, in the year 2018, the Ayushman Bharat Scheme was launched.7 It is also known as the National Health Protection Scheme or the Pradhan Mantri Jan Arogya Yojna. The goal of this scheme is to provide the highest level of health to all, at all ages. For the successful implementation of this scheme, the Government of India has decided to upgrade the existing healthcare services as well as establish health and wellness centres all over the country. The conceptualization behind the development of the scheme was to deliver primary healthcare services and to provide health insurance.8 The scheme also mentions priority given to women and girls, cashless treatment to all beneficiaries, no financial hardships and non-denial of treatment by hospitals. However, the focus on quality in this scheme is limited. Ensuring cashless treatment and health services for all, does not guarantee quality and respectful care. This also does not guarantee that women will not have to face the brunt of informal payments or hospital detention if they refuse informal payments such as tips or extra money for services. Women like before, may continue to face abuse, disrespect and ill treatment in lieu of the free services provided. Promotive, preventive, rehabilitative and curative services are mentioned in UHC, but the assurance of provision of services by skilled staff, continuum of care and regulations on abandonment and threats are still lacking. The different types of services provided under Ayushman Bharat and the cash incentives might increase the workload of the health facilities, where again, quality and rights may be compromised.9 UHC is for all people and communities, and therefore discrimination and autonomy of women in this scheme needs to be addressed. Another challenge of the scheme is to strengthen the existing healthcare infrastructure that will help in delivering quality care. Mechanisms for reporting problems faced by the recipients are lacking. Therefore, in spite of the scheme mentioning maternal services, special emphasis on the components of RMC including physical and verbal abuse, non-dignified, non-consented care, forced procedures, lack of privacy and confidentiality, discrimination, abandonment, threats and detention are lacking. Few concerns of RMC are just touched upon in the scheme, and a ‘rights-based’ approach including quality of care and services provided, still needs to be addressed. RMC rights can be safeguarded in the UHC agenda provided the focus is on the quality of care delivered.
FUTURE RESEARCH
Future research should focus on RMC among the beneficiaries of the scheme. This will help in identifying the problems faced by the beneficiaries of the scheme and accordingly, interventions may be planned, and policy and programmes may be implemented.
CONCLUSION
Data with respect to UHC and RMC are lacking, suggesting the need for collecting data globally as well as in India. While planning for UHC, the importance of RMC should be considered. Integration of RMC within the context of UHC is essential.
ACKNOWLEDGEMENTS
Funding support from the Department of Science and Technology, Government of India, for INSPIRE Fellowship to Dr Humaira Ansari is gratefully acknowledged.
Conflicts of interest
None declared
References
- Delivering quality health services: A global imperative for universal health coverage. 2018. Geneva: World Health Organization, Organisation for Economic Cooperation and Development, and The World Bank; Available at www.worldbank.org/en/topic/universalhealthcoverage/publication/delivering-quality-health-services-a-global-imperative-for-universal-health-coverage (accessed on 12 Mar 2020)
- [Google Scholar]
- Respectful maternity care: The universal rights of childbearing women. 2011. White Ribbon Alliance. Available at www.whiteribbonalliance.org/wp-content/uploads/2017/11/Final_RMC_Charter.pdf (accessed on 12 Mar 2020)
- [Google Scholar]
- The mistreatment of women during childbirth in health facilities globally: A mixed-methods systematic review. PLoS Med. 2015;12:e1001847.
- [CrossRef] [PubMed] [Google Scholar]
- Losing women along the path to safe motherhood: Why is there such a gap between women's use of antenatal care and skilled birth attendance? A mixed methods study in northern Uganda. BMC Pregnancy Childbirth. 2015;15:287.
- [CrossRef] [PubMed] [Google Scholar]
- The Lancet maternal health series: Global research and evidence. 2016. Lancet. Available at www.maternalhealthseries.org (accessed on 12 Mar 2020)
- [Google Scholar]
- Tracking Universal Health Coverage: 2017 Global Monitoring Report. 2017. World Health Organization and International Bank for Reconstruction and Development/ The World Bank. Available at www.who.int/healthinfo/universal_health_coverage/report/2017/en/ (accessed on 12 Mar 2020)
- [Google Scholar]
- Cabinet Approves Ayushman Bharat-National Health Promotion Mission. Available at https://pib.gov.in/Pressreleaseshare.aspx?PRID=1546948 (accessed on 12 Mar 2020)
- [Google Scholar]
- Ayushman Bharat Yojana: A memorable health initiative for Indians. Int J Community Med Public Health. 2019;5:3152-3.
- [CrossRef] [Google Scholar]
- India's national health protection scheme: A preview. Med J Dr DY Patil Vidapeeth. 2018;11:385.
- [CrossRef] [Google Scholar]




