Translate this page into:
Salt-sensitive phenotypes: A community-based exploratory study from northeastern India
2 Indian Council of Medical Research, New Delhi, India
3 Assam Medical College, Dibrugarh, Assam, India
4 Institute of Genomic and Integrative Biology, New Delhi, India
Corresponding Author:
Jagadish Mahanta
Regional Medical Research Centre, North East Region (ICMR), Dibrugarh 786001, Assam
India
jmahanta@gmail.com
| How to cite this article: Borah PK, Sharma M, Kalita HC, Pasha M, Paine SK, Hazarika D, Bhattacharjee CK, Mahanta J. Salt-sensitive phenotypes: A community-based exploratory study from northeastern India. Natl Med J India 2018;31:140-145 |
Abstract
Background. Salt sensitivity is known to increase the risk of cardiovascular diseases in both normotensive and hypertensive subjects. The population in the northeastern region of India consumes excess dietary salt but their saltsensitive phenotype is not known.Methods. We did a community-based exploratory study using volunteers in the northeastern region of India to determine salt-sensitive (SS) and salt-resistant (SR) phenotypes. A total of 374 (206 normotensive and 168 hypertensive) subjects who gave informed consent were stabilized for salt with 7 days of a low-salt (2.9 g/day) diet followed by 7 days of a high-salt (15.2 g/day) diet. SS was defined as an increase of mean arterial blood pressure ≥9 mmHg after a high-salt diet.
Results. We noted an increase in systolic blood pressure of 9.3 mmHg in normotensive subjects and 10.7 mmHg in hypertensive subjects, with a modest effect on diastolic blood pressure (6.9 mmHg in normotensive and 8.2 mmHg in hypertensive subjects) after a high-salt diet. Salt-sensitive phenotype was present in 40.8% of normotensive and 47.6% of hypertensive subjects. Resistance to introduction of high salt was observed in 43.7% of normotensive and 33.9% of hypertensive subjects. Consumption of extra salt (adjusted OR 1.99, 95% CI 1.25–3.18) was independently associated with salt sensitivity.
Conclusion. Salt sensitivity was found in a large proportion of normotensive and hypertensive subjects. Restriction of salt intake could be an effective intervention to control hypertension among salt-sensitive subjects.
Introduction
Worldwide, hypertension is among the most prevalent non-communicable diseases. India contributed 7.1 million deaths and 64.3 million disability-adjusted life years (DALYs) due to hypertension to the global burden.[1] About 16% of ischaemic heart disease, 21% of peripheral vascular diseases and 24% of patients with acute myocardial infarction (AMI) are ascribed to hypertension.[2] Dietary sodium intake plays an important role in regulating blood pressure (BP), which may decrease following restriction on dietary salt and increase in a subset of people following consumption of excess salt.[3] Studies have shown that reducing sodium intake results in a step-wise reduction in BP.[3] Populations of developing countries including India habitually consume excess dietary salt than the intake recommended by the JNC-7 guidelines.[4] However, the linear relation between sodium intake and BP was inconsistent across different studies carried out worldwide.[5],[6],[7],[8] The inconsistency between BP and consumption of dietary salt may be ascribed to inadequacy of the linear model due to age, geographical, environmental and population heterogeneity and a complex interplay of gene and environment among different ethnic groups.[9] An acute change in BP following such low- or high-salt consumption is termed as salt sensitivity and commonly reported in large segments of a population, especially in those with diabetes, hypertension and the elderly.[10],[11] Salt sensitivity in a population may predict a chronic rise in BP leading to development of hypertension.[11] Studies in the northeastern region of India have suggested a wide variation in the prevalence of hypertension and significant association with consumption of extra salt (salt as a side dish) in the diet.[12],[13],[14] This study was done in both hypertensive and normotensive subjects in the same population groups as the earlier study[12],[13],[14] to determine saltsensitive phenotypes by measuring the response of BP to dietary salt intake.
Methods
Study site and subjects
Temporary field clinics were set up in tea gardens and selected localities of Assam and Mizoram to check the BP of the local population. Only normotensive (systolic BP [SBP] <120 mmHg and diastolic BP [DBP] <80 mmHg) and stage 1 hypertensive (SBP 140–159 mmHg and/or DBP 90–99 mmHg or on anti-hypertensive therapy) subjects aged 20 years and above were included after the study protocol was clearly explained to them. BP was checked using a mercury sphygmomanometer twice in the sitting position and on two separate occasions, at least one week apart. Those with a wide variation in BP between the first and second check-ups (taken after 1 week) were excluded from the study. We took the average of two readings of BP during the second sitting.
Subjects were purposively selected from the volunteers who opted for the study. All subjects were apprised of the protocol including possible hazards of low- and high-salt consumption and the necessity for strict dietary compliance. A total of 374 individuals (206 normotensive and 168 hypertensive) who agreed to comply with the study protocol and gave written informed consent were recruited for the study. Persons excluded were those with secondary hypertension and diabetes mellitus (history of diabetes or fasting blood sugar ≥126 mg/dl), renal disease (serum creatinine ≥1.4 mg/dl) and coronary artery disease on the basis of clinical features and electrocardiogram. We also excluded pregnant women and women receiving oral contraceptives or hormone replacement therapy. Our study was approved by the institutional ethics committee of the Regional Medical Research Centre, North East Region (ICMR), Dibrugarh.
Collection of sociodemographic and clinical data
Subjects were interviewed by field investigators and relevant sociodemographic, dietary and clinical information was recorded in a specially designed and pretested questionnaire. Participants underwent a complete clinical examination including measurement of BP. Height and body weight were measured using an anthropometric rod and platform balance (SECA) by trained technicians who followed standard techniques. Waist and hip circumference were measured to the nearest 0.5 cm.
Collection of blood sample
Five ml of venous blood was collected for biochemical investigations including blood glucose, urea and creatinine. We used colorimetric methods to measure these parameters.
Collection of 24-hour urinary sodium
Subjects were instructed to commence collection after emptying their bladder and discarding the urine. The time was noted as the start time and all urine voided subsequently was collected for a duration of 24 hours. Subjects were requested to report the exact start and stop times for collection of urine. Completeness of collection was sought by providing detailed instructions to the study subjects. They were asked to redo urine collection if they reported missing more than a few drops of urine or if the total 24hour urine volume was <250 ml. Total volume of the collection was recorded and sample aliquots were taken and stored at –20 °C till analysis.
Laboratory estimation of urinary sodium
An ion exchange chromatography (Dionex, USA) system was used to estimate urinary sodium as per the manufacturer’s instructions. Briefly, the urine sample was diluted with de-ionized water in the ratio 1:25 and run in the chromatograph. The chromatograph provided the concentration of urinary sodium against the sodium standard prepared as 100 ppm/L concentration. The ppm value of urinary sodium was obtained and then multiplied by the dilution factor, i.e. 25 to get the actual concentration of urinary sodium in ppm/L. The value of 24-hour urinary sodium was calculated by multiplying total urine output (in litres). Finally, the ppm value was converted to mmol/L by dividing ppm values with the atomic mass of sodium, i.e. 22.99.
Implementation of salt restriction (low salt) and salt supplementation (high salt)
The medical officer and field staff, who were acquainted with the study protocol and the method of delivery of salt to the study subjects, implemented the salt restriction/supplementation process. The households of the selected subjects were identified and a brief discussion was held with the person responsible for preparing food. The person responsible for cooking was advised to prepare food for the study subject without addition of any salt. The study subject was asked to add salt from the supplied salt packet containing a specific amount of salt (low or high salt) as per protocol. Salt packets were supplied daily and dietary compliance was verified. Only one brand of salt was used. The other members of the family were free to take any amount of salt. Hypertensive and normotensive subjects were put on 2.9 g of dietary salt/day (i.e. low sodium or salt-restriction diet) for 7 days followed by 15.2 g of dietary salt/day (i.e. high sodium or salt supplementation diet) for 7 days. The project staff, including the medical officer, visited the households of selected individuals daily and recorded salt intake by the study subjects during the study period. Further, the 24-hour urinary sodium excretion was measured on the last day of each period to assess compliance with the diet protocol. Sodium excretion of ≥50 mmol over 24 hours for the low-sodium diet and ≥165 mmol over 24 hours for the high-salt supplementation was considered to represent dietary compliance. Subjects who did not adhere to the low- or highsalt diet were excluded from the study. Urine samples were collected as per the study protocol [Figure - 1].
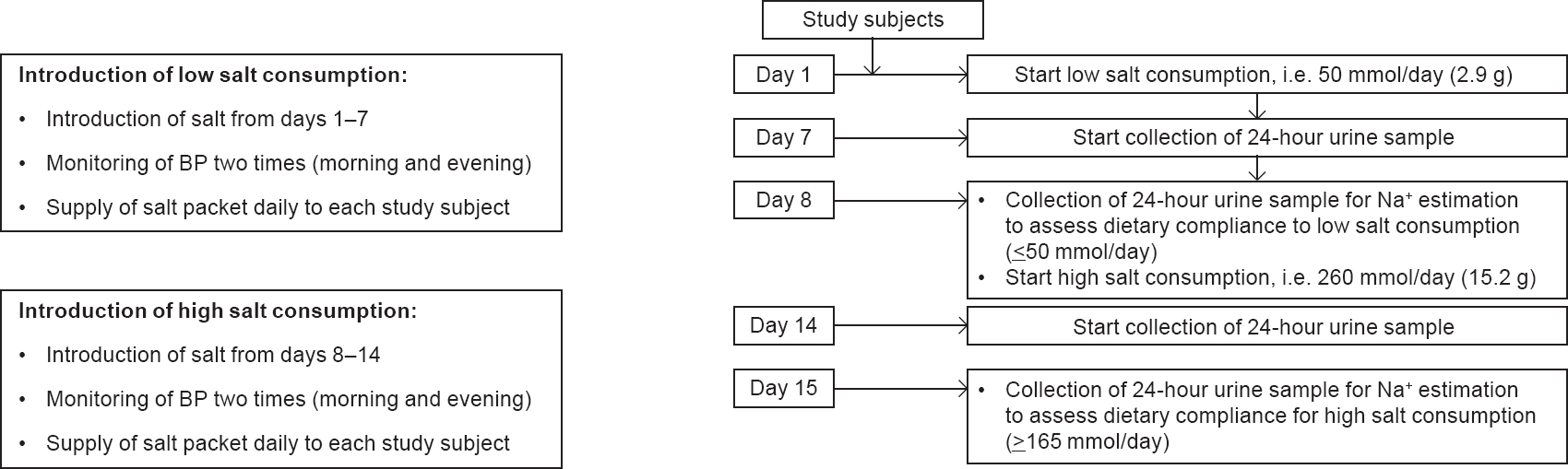 |
| Figure 1: Summary of study protocol |
Definition and phenotype of salt sensitivity Subjects receiving low- and high-salt diet with ≥9 mmHg increase in mean arterial BP (MABP) at the end of the high-salt phase compared with the low-salt phase were classified as salt-sensitive (SS), whereas those with <6 mmHg increase were classified as salt-resistant (SR) and those with a difference of 6–9 mmHg were classified as salt-indeterminate.[15] The MABP was calculated as [2 X (DBP) + SBP]/3.
Results
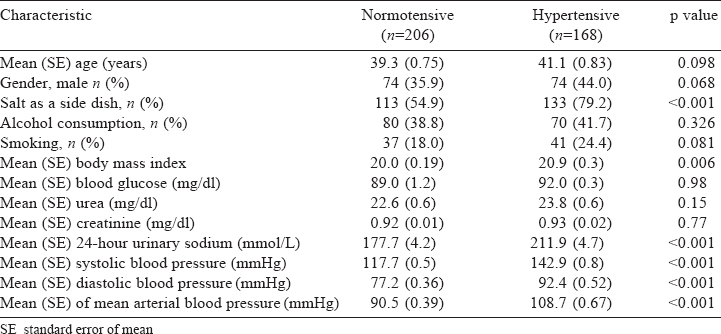
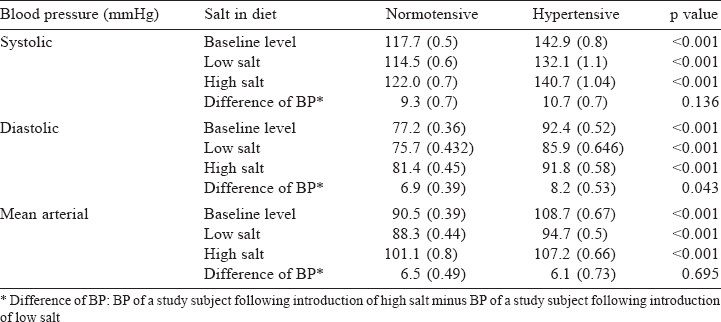
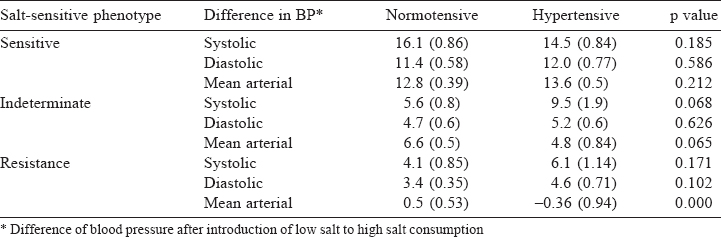
Our study included 374 subjects, 206 of whom were normotensive and 168 hypertensive. Hypertensive subjects had significantly elevated 24-hour urinary sodium excretion (p<0.001, [Table - 1]). The SBP had a mean increase of 9.3 mmHg for normotensive and 10.7 mmHg for hypertensive subjects (p=0.136; [Table - 2]) while the DBP had a mean increase of 6.9 mmHg in normotensive and 8.2 mmHg in hypertensive subjects (p=0.043).
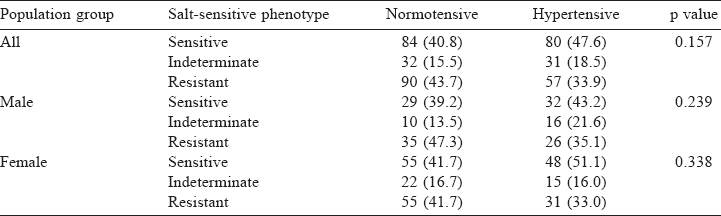
The SS phenotype was present in 40.8% of the normotensive and 47.6% of the hypertensive subjects [Table - 3]. The SR phenotype was seen in 43.7% of the normotensive and 33.9% of the hypertensive subjects. However, these differences were not statistically significant.
Differences in BP (SBP, DBP and MABP) between the introduction of high salt and salt stabilized period were also analysed. There were no significant differences between the BP of normotensive and hypertensive subjects [Table - 4].
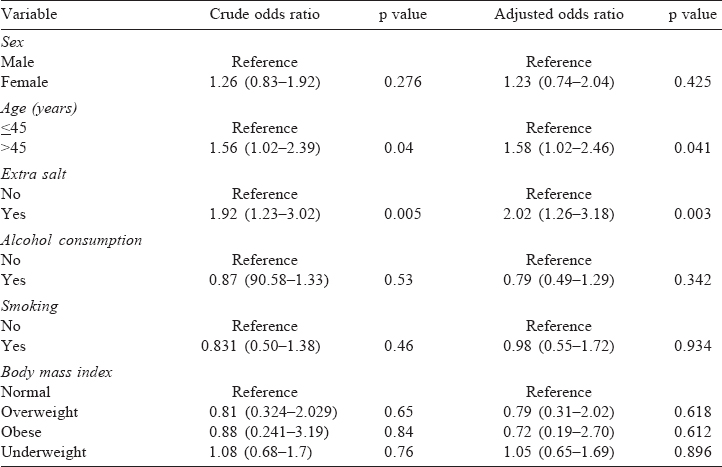
Univariate and multivariate binary logistic regression analyses showed that consumption of excess salt (adjusted OR 2.02, 95% CI 1.26-3. 18) and age ≥45 years (adjusted OR 1.58, 95% CI 1.02–2.45) were independent predictors of SS phenotype [Table - 5].
Discussion
Our study assessed the frequency of the SS phenotype among the northeastern population. Among those living in the northeast especially the Assamese, tea garden workers and the population of Mizoram have had a steady rise of BP over the past few decades[12],[13],[14] with a potential to develop cardiovascular morbidity and mortality. Salt consumption by these populations is high and is possibly associated with hypertension. Therefore, determination of response to BP following consumption of dietary salt is important.
The INTERSALT study[3] showed a relationship between intake of dietary salt and BP in western societies. The response of BP following introduction of salt has been described by several investigators using different techniques and in different populations.[16],[17],[18],[19],[20] Massive sodium loading in normotensive subjects has been shown to result in a rise in BP[21] and a modest reduction in sodium intake has resulted in a decrease in BP.[22]
In our study too the SBP, DBP and MABP increased following 7 days of high-sodium diet (260 mmol/day, ~15.2 g of dietary salt) after a salt stabilization period of 7 days with low-sodium diet (50 mmol/day, ~2.9 g) in both normotensive and hypertensive adults. The magnitude of elevation of BP was more for SBP, which ranged from 9.3 mmHg (normotensive subjects) to 10.7 mmHg (hypertensive subjects), in comparison with DBP (6.9 mmHg in normotensive and 8.2 mmHg hypertensive subjects). Our findings are similar to those reported by Mufunda et al.[23] However, reduction in SBP and DBP in normotensive subjects was much higher in our population than in another population group.[22] A study done among Indians also revealed a rise of BP with an increase in quintile of salt intake.[24] A meta-analysis by Strazzullo et al.[25] showed a decrease in SBP of 4-5 mmHg and DBP of 1-3 mmHg following reduction of salt intake of 5–6 g/day. A meta-analysis by He et al. also showed a reduction in SBP of 5.4 mmHg and DBP of 2.8 mmHg in hypertensive patients when salt intake was reduced by 100 mmol/day, i.e. 5 g sodium chloride/day.[26] The Prospective Urban Rural Epidemiological (PURE) study that enrolled more than 100 000 subjects described the link between salt intake and BP.[27]
The response of BP to salt loading and depletion in humans has a normal distribution, and not dichotomous.[15] Therefore, arbitrary cut-offs for the magnitude of BP response are required to classify subjects into SS and SR groups. Different workers have defined salt sensitivity differently. Sullivan et al. defined salt sensitivity as a change in BP (office measurement) of 5%–10% or at least 5 mmHg, in response to a change in salt intake.[28] Salt sensitivity is also defined as an increase in MABP of at least 4 mmHg (24-hour ambulatory BP monitoring) with an increase in salt intake.[29] Yatabe et al. defined salt sensitivity on the basis of salt sensitivity index, which is the difference between MABP on low-salt and high-salt diets, divided by the MABP on low-salt diet. As per this definition, salt sensitivity index should be at least 5%.[30] We used the response of BP to dietary salt intake. It has been shown that results of dietary protocols reproduced in a fair manner those obtained with the inpatient protocol above, provided that contents of the high- and low-salt diets are 200–220 and 15–20 mmol of sodium per day, respectively, and that the duration of each diet is approximately 1 week.[31],[32]
We did a multivariate logistic regression analysis to determine the predictors of salt-sensitive phenotype. Consumption of extra salt (salt as a side dish) and older age (≥45 years) were independently associated with the salt-sensitive phenotype. Higher salt intake had a strong association with BP as shown in the PURE study.[27] Association of age with salt-sensitive phenotype may be due to the strong association of salt excretion and BP with advancing age.[33]
Reducing salt intake in a population is an easy, efficient and cost-effective means to reduce hypertension and associated healthcare costs. We believe this would result in a major improvement in public health.[25],[34] Our data may form the basis to initiate salt restriction to reduce the burden of hypertension. In the dietary approaches to stop hypertension (DASH) study, a reduction in sodium intake led to a step-wise decrease in BP.[35] Considering the significant change following introduction of high salt consumption and the evidence of salt-induced change in BP, a salt-restriction strategy may be useful for our communities to reduce BP and associated cardiovascular morbidity and mortality.
Developing countries such as India are facing a double burden of iodine deficiency disorders along with an epidemic of chronic diseases such as hypertension leading to increased morbidity and mortality. Salt is the vehicle for supplementation of iodine among patients with iodine deficiency disorders in India. Therefore, salt restriction without any evidence of its effect on the reduction of BP is irrational. Our study will help in formulating policy for recommendation of salt to prevent both these diseases. A previous study has shown that as much as ~3.3 g/day salt is palatable and therefore a more liberal approach limiting salt intake of 5 g per day as advocated by WHO may be adopted in India to reduce the burden of hypertension without interfering with the iodine supplementation programme.[36] We found a positive association of consumption of extra salt with salt sensitivity. It is easy to modify this dietary risk behaviour and reduce dietary salt intake by the community.
Our study has some limitations. We assessed 24-hour urinary sodium excretion which has its limitations. We did not use para amino benzoic acid recovery criteria or creatinine in the 24-hour urine samples to assess completeness of the urine collection. Instead, we adopted the procedure used by two previous, multi-country population-based studies, namely the International Population Study on Macronutrients and BP[3] and the International Study of Sodium, Potassium, and Blood Pressure.[4] We took special care to ensure 24-hour urine collection, but the method is cumbersome and inconvenient and may lead to some error. Variations in the concentration level of urinary sodium due to possible consumption of corticosteroids, non-steroidal anti-inflammatory drugs, diuretics, etc. could not be ruled out.
In conclusion, we have shown that introduction of high salt can cause a significant increase in the SBP and DBP in the study population. Therefore, intake of excess salt might be responsible for hypertension in our study population. It is advisable to restrict salt intake to reduce the burden of hypertension.
Acknowledgement
We are grateful to the Indian Council of Medical Research, New Delhi for the financial assistance provided for this study.
Conflicts of interest. None declared
| 1. | Subramanian H, Soudarssanane MB, Jayalakshmy RD, Navasakthi TD, Sahai A, Saptharishi LG. Non-pharmacological interventions in hypertension: A community-based cross-over randomized controlled trial. Indian J Community Med 2011;36: 191-6. [Google Scholar] |
| 2. | Assessment of burden of non-communicable diseases in India. Final report of Project WR/SE IND RPC 001 RB 02. SE/02/419575. New Delhi:Indian Council of Medical Research; 2004. Available at www. whoindia. org/LinkFiles/Assessment_of_Burden_ of_NCD_Hypertension_Assessment_of_Burden_of_NCDs.pdf(accessed on 27 Aug 2009 Aug 27). [Google Scholar] |
| 3. | Intersalt Cooperative Research Group. Intersalt: An international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Br Med J 1988;297:319-28. [Google Scholar] |
| 4. | Dyer AR, Elliott P, Stamler J, Chan Q, Ueshima H, Zhou BF. INTERMAP Research Group. Dietary intake in male and female smokers, ex-smokers, and never smokers : The INTERMAP study. J Hum Hypertens 2003;17:641-54. [Google Scholar] |
| 5. | Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA 2003;289:2560-72. [Google Scholar] |
| 6. | Staessen JA, Lijnen P, Thijs L, Fagard R. Salt and blood pressure in community-based intervention trials. Am J Clin Nutr 1997;65 (2 Suppl):661S-670S. [Google Scholar] |
| 7. | Alderman MH. Reducing dietary sodium: The case for caution. JAMA 2010;303: 448-9. [Google Scholar] |
| 8. | Kolata G. No benefit seen in sharp limits of salt in diet. The New York Times 2013. [Google Scholar] |
| 9. | Cabrera CP, Ng FL, Warren HR, Barnes MR, Munroe PB, Caulfield MJ. Exploring hypertension genomewide association studies findings and impact on patho- physiology, pathways, and pharmacogenetics. Wiley Interdiscip Rev Syst Biol Med 2015;7:73-90. [Google Scholar] |
| 10. | Gerdts E, Svarstad E, Myking OL, Lund-Johansen P, Omvik P. Salt sensitivity in hypertensive type 1 diabetes mellitus. Blood Press 1996;5:78-85. [Google Scholar] |
| 11. | Choi HY, Park HC, Ha SK. Salt sensitivity and hypertension: A paradigm shift from kidney malfunction to vascular endothelial dysfunction. Electrolyte Blood Press 2015;13:7-16. [Google Scholar] |
| 12. | Hazarika NC, Biswas D, Narain K, Phukan RK, Kalita HC, Mahanta J. Differences in blood pressure level and hypertension in three ethnic groups of northeastern India. Asia Pac J Public Health 2000; 12:71-8. [Google Scholar] |
| 13. | Hazarika NC, Biswas D, Narain K, Kalita HC, Mahanta J. Hypertension and its risk factors in tea garden workers of Assam. Natl Med J India 2002;15:63-8. [Google Scholar] |
| 14. | Hazarika NC, Narain K, Biswas D, Kalita HC, Mahanta J. Hypertension in the native rural population of Assam. Natl Med J India 2004;17:300-4. [Google Scholar] |
| 15. | Weinberger MH, Miller JZ, Luft FC, Grim CE, Fineberg NS. Definitions and characteristics of sodium sensitivity and blood pressure resistance. Hypertension 1986;8:II127-II134. [Google Scholar] |
| 16. | Kawasaki T, Delea CS, Bartter FC, Smith H. The effect of high sodium and low sodium intakes on blood pressure and other related variables in human subjects with idiopathic hypertension. Am J Med 1978;64:193-8. [Google Scholar] |
| 17. | Fujita T, Henry WL, Bartter FC, Lake CR, Delea CS. Factors influencing blood pressure in salt sensitive patients with hypertension. Am J Med 1980;69:334-44. [Google Scholar] |
| 18. | Fujita T, Noda H, Ando K. Sodium susceptibility and potassium effects in young patients with borderline hypertension. Circulation 1984;69:468-76. [Google Scholar] |
| 19. | Dustan HP, Tarazi RC, Bravo EL. Physiologic characteristics of hypertension. Am J Med 1972;52:610-22. [Google Scholar] |
| 20. | Sullivan JM, Ratts TE, Taylor JC, Kraus DH, Barton BR, Patrick DR, et al. Hemodynamic effects of dietary sodium in man: A preliminary report. Hypertension 1980;2:506-14. [Google Scholar] |
| 21. | Luft FC, Rankin LI, Bloch R, Weyman AE, Willis LR, Murray RH, et al. Cardiovascular and humoral responses to extremes of sodium intake in normal black and white men. Circulation 1979;60:697-706. [Google Scholar] |
| 22. | Miller JZ, Daugherty SA, Weinberger MH, Grim CE, Christian JC, Lang CL. Blood pressure response to dietary sodium restriction in normotensive adults. Hypertension 1983;5:790-5. [Google Scholar] |
| 23. | Mufunda J, Chimoskey JE, Matenga J, Musabayane C, Sparks HV Jr. Blood pressure response to acute changes in dietary sodium in young Zimbabwean men. J Hypertens 1992;10:279-85. [Google Scholar] |
| 24. | Ravi S, Bermudez OL, Harivanzan V, Chui KHK, Vasudevan P, Must A, et al. Sodium intake, blood pressure, and dietary sources of sodium in an adult south Indian population. Ann Global Health 2016:82. [Google Scholar] |
| 25. | Strazzullo P, D’Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: Meta-analysis of prospective studies. BMJ 2009;339:b4567. [Google Scholar] |
| 26. | He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomized trials. BMJ 2013;346:f1325. [Google Scholar] |
| 27. | Mente A, O’Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, et al. Association of urinary sodium and potassium excretion with blood pressure. N Eng J Med 2014;371:601-11. [Google Scholar] |
| 28. | Sullivan JM. Salt sensitivity. Definition, conception, methodology, and long-term issues. Hypertension 1991;17 (1 Suppl):I61-I68. [Google Scholar] |
| 29. | De la Sierra A, Giner V, Bragulat E, Coca A. Lack of correlation between two methods for the assessment of salt sensitivity in essential hypertension. J Hum Hypertens 2002;16:255-60. [Google Scholar] |
| 30. | Yatabe MS, Yatabe J, Yoneda M, Watanabe T, Otsuki M, Felder RA, et al. Salt sensitivity is associated with insulin resistance, sympathetic over activity and decreased suppression of circulating renin activity in lean patients with essential hypertension. Am J Clin Nutr 2010;92:77-82. [Google Scholar] |
| 31. | Weinberger MH, Stegner JE, Fineberg NS. A comparison of two tests for the assessment of blood pressure responses to sodium. Am J Hypertens 1993;6:179-84. [Google Scholar] |
| 32. | Sharma AM, Schorr U, Cetto C, Distler A. Dietary v intravenous salt loading for the assessment of salt sensitivity in normotensive men. Am J Hypertens 1994;7: 1070-5. [Google Scholar] |
| 33. | Simonia G, Andronikashvili I, Nozadze P. Aging and salt-sensitivity. Bull Georg Natl Acad Sci Medical Sciences 2009;3 (2): 181-4. [Google Scholar] |
| 34. | Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med 2010;362:590-9. [Google Scholar] |
| 35. | Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. for the DASH Collaborative Research Group. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117-24. [Google Scholar] |
| 36. | He FJ, MacGregor GA. How far should salt intake be reduced? Hypertension 2003;42:1093-9. [Google Scholar] |
Fulltext Views
3,076
PDF downloads
14,240




