Translate this page into:
Scrub typhus presenting as mitral valve infective endocarditis
Correspondence to DEBASISH DAS; dasdebasish54@gmail.com
[To cite: Devi S, Das D, Acharya D, Das T, Singh S, Gupta JD, et al. Scrub typhus presenting as mitral valve infective endocarditis. Natl Med J India 2024;37:203–4. DOI: 10.25259/NMJI_295_21]
Abstract
Scrub typhus presenting as infective endocarditis of the mitral valve is rare. There are few reports of infective endocarditis by scrub typhus with just one previous report of involvement of the aortic valve. An 18-year-old woman presented with prolonged fever for 1 month. Her repeated blood cultures were negative. She was finally diagnosed to have scrub typhus with scrub typhus IgM being positive and became afebrile with prolonged oral doxycycline monotherapy. Although atypical organisms such as Legionella, Mycoplasma and Coxiella are described to cause culture-negative endocarditis, vegetations were present on both the anterior and posterior mitral valve leaflets in our patient.
INTRODUCTION
Scrub typhus is an acute febrile illness caused by Orientia tsutsugamushi. The name derives from the type of vegetation (i.e. terrain between woods and clearings) that harbours the vector. Scrub typhus develops following a painless, unnoticed chigger bite with an average incubation period of 10 days with the development of a painless papule with central necrosis known as an eschar. The patient presents with high-grade fever (104–105 °F) with shaking chills and tender lymphadenopathy. Complications of scrub typhus include pneumonia, encephalitis, renal failure, shock and disseminated intravascular coagulation (DIC). Infective endocarditis in scrub typhus is not a known complication. We describe mitral valve endocarditis in scrub typhus.
THE CASE
An 18-year-old woman presented to the outpatient of the Department of Medicine with a history of prolonged irregular fever (101–103 °F) for 1 month, non-responsive to conventional antibiotics. On examination, she had a temperature of 101 °F, heart rate 120 beats per minute and blood pressure 110/70 mmHg. General examination revealed that she had mild pallor without any regional lymphadenopathy. Respiratory and cardiovascular system examinations were within normal limits and she had mild splenomegaly. Serum chemistry revealed she had anaemia (Hb 9.2 g/dl), total leucocyte count (TLC) of 4200/cmm with 57% neutrophil and 34% lymphocytes, platelet count of 220 000/cmm and erythrocyte sedimentation rate of 52 mm/hour. The peripheral smear revealed microcytic hypochromic anaemia with normal myeloid and megakaryocyte lineage.
Malarial parasite, Widal titre, and urine routine and microscopic examination were within normal limits. Antinuclear antibody (ANA), cANCA (antineutrophil cyto-plasmic antibody), and pANCA were also normal. Repeated blood culture revealed no growth. Fungal culture was also negative. Chest X-ray was within normal limits. Ultrasound abdomen and pelvis was normal. C-reactive protein was positive with a value of 8 ng/ml. The patient was started on injectable ceftriaxone and gentamicin. However, this did not provide any relief. An echocardiography revealed vegetations over both anterior and posterior mitral valve leaflets (Fig. 1). She was started on injection vancomycin on the assumption that she had received multiple oral and intravenous antibiotics in the past, which were responsible for culture negativity. However, the fever did not subside after 7 days of vancomycin.
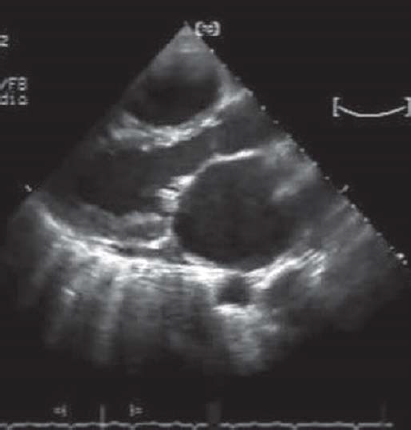
- Vegetations on the tip of the anterior and posterior mitral valve leaflets in the parasternal long axis view
A scrub typhus IgG and IgM was done as a part of her work up for PUO. Scrub typhus IgM was positive. She was started with oral doxycycline 100 mg twice daily and became afebrile after 7 days. She was discharged on oral doxycycline for 6 weeks. During follow-up after 6 weeks, she was afebrile with healed calcified vegetations on the mitral leaflets without any mitral regurgitation and normal left ventricular systolic function.
DISCUSSION
Scrub typhus is an infectious acute febrile illness caused by Orientia (formerly Rickettsia) tsutsugamushi, an obligate intracellular Gram-negative bacterium. Although scrub typhus was originally recognized as a rickettsial disease, O. tsutsugamushi differs from other rickettsiae with respect to cell-wall structure and genetic composition. Scrub typhus is prevalent in sandy beaches, mountain deserts and equatorial rain forests. There exists a ‘tsutsugamushi triangle’, which extends from northern Japan and eastern Russia in the north to northern Australia in the south and Pakistan and Afghanistan in the west, where the disease is endemic. Scrub typhus is often acquired during occupational or agricultural exposures1 because active rice fields are an important reservoir for transmission.2 It was the second or third most common infection reported in US troops stationed in Vietnam.3
There has been a resurgence of scrub typhus across India in recent years; and it has re-emerged as a major cause of acute undifferentiated febrile illnesses (AUFI) with high morbidity and mortality. A large numbers of cases are being reported from Tamil Nadu, Andhra Pradesh, Karnataka and Kerala in the South; Himachal Pradesh, Uttaranchal, and Jammu and Kashmir in the North; Meghalaya, Assam and Nagaland in the Northeast; West Bengal and Bihar in the East; and Maharashtra and Rajasthan in the West. Studies from India report case fatality rates (CFR) ranging from 1.3% to 33.5% depending on the organ involvement and complications. In the past decade, there were 18 781 confirmed cases of scrub typhus reported in 138 hospital-based studies and two community-based studies. IgM ELISA was used in 122 studies to confirm the cases in the majority (89%). The proportion of scrub typhus among acute undifferentiated febrile illness (AUFI) studies was 25.3%, and community seroprevalence was 34.2%. Ninety studies had data published on multiple organ involvement out of which 17.4% of cases had multiple organ dysfunction syndromes, 20.4% of patients required ICU admission, and 19.1% needed ventilation. The overall case-fatality rate was 6.3%, and the mortality among those with multi-organ dysfunction syndrome was as high as 38.9%.4 Cardiac involvement in scrub typhus is rare. However, cases of fatal myocarditis have been reported.5 Relative bradycardia occurs in scrub typhus akin to enteric fever.6 We did not come across any reports of mitral valve involvement in patients with scrub typhus. Our patient had mitral valve endocarditis, which was effectively treated with doxycycline for 6 weeks. Scrub typhus may rarely cause acute renal failure shock and DIC.2 With doxycycline therapy, the patient recovers within 36 hours. Scrub typhus complicates patients older than 60 years, without eschar, or with white blood cell (WBC) counts higher than 10 000/cmm.7 Similarly, our patient had no typical eschar but developed a complication in the form of mitral valve endocarditis. Routine laboratory studies in patients with scrub typhus reveal early lymphopenia with late lymphocytosis, which was absent in our case. Although thrombocytopenia serves as a bad prognostic marker,8 our patient had a normal platelet count. Elevated transaminase levels may be present in 75%–95% of patients; however, our patient had normal liver function test results.
We used rapid immunochromatographic tests for detection of IgM and IgG against O. tsutsugamushi, which are more sensitive and specific than the immunofluorescence assay for the early diagnosis of scrub typhus.9 The current drug of choice for scrub typhus is doxycycline.10 Relapses may occur if antibiotics are not taken for a long enough period. We found only one report of aortic valve endocarditis in scrub typhus.11
Conclusion
We report a rare complication of scrub typhus, mitral valve endocarditis, which was effectively treated with doxycycline.
Conflicts of interest
None declared
References
- Scrub typhus in Darjeeling, India: Opportunities for simple, practical prevention measures. Trans R Soc Trop Med Hyg. 2009;103:1153-8.
- [CrossRef] [Google Scholar]
- Scrub typhus In: Guerrant RL, Walker DH, Weller PF, eds. Tropical infectious diseases. Principles, pathogens and practice Vol Vol 1. (2nd ed). Philadelphia, PA: Elsevier Churchill Livingstone; 2006.
- [Google Scholar]
- Scrub typhus in south Vietnam: A study of 87 cases. Ann Intern Med. 1973;79:26-30.
- [CrossRef] [Google Scholar]
- The burden of scrub typhus in India: A systematic review. PLOS Negl Trop Dis. 2021;15:1-15.
- [CrossRef] [Google Scholar]
- Acute fulminant myocarditis in scrub typhus. Ann Trop Paediatr. 2008;28:149-54.
- [CrossRef] [Google Scholar]
- Scrub typhus infections poorly responsive to antibiotics in northern Thailand. Lancet. 1996;348:86-9.
- [CrossRef] [Google Scholar]
- Clinical and laboratory findings associated with severe scrub typhus. BMC Infect Dis. 2010;10:108.
- [CrossRef] [Google Scholar]
- Clinical study of 20 children with scrub typhus at Chiang Rai Regional Hospital. J Med Assoc Thai. 2005;88:1867-72.
- [Google Scholar]
- Development of new, broadly reactive, rapid IgG and IgM lateral flow assays for diagnosis of scrub typhus. Am J Trop Med Hyg. 2012;87:148-52.
- [CrossRef] [Google Scholar]
- Tsutsugamushi disease presenting with aortic valve endocarditis: A case report and literature review. Am J Cardiovasc Dis. 2016;6:185-90.
- [Google Scholar]




