Translate this page into:
Surveillance of maternal deaths in Barpeta district of Assam
Corresponding Author:
Priyanka Das
Department of Community Medicine, Fakhruddin Ali Ahmed Medical College, Barpeta, Assam
India
drpriyankadas4@gmail.com
| How to cite this article: Kakoty SD, Das P. Surveillance of maternal deaths in Barpeta district of Assam. Natl Med J India 2018;31:206-210 |
Abstract
Background. Assam has the highest maternal mortality in India. It is difficult to make a precise estimate of maternal mortality because the available information from various surveys has a wide confidence interval. Biomedical causes of maternal mortality are known, but there is little information on determinants of sociocultural and health system aspects. Delays at various levels such as at home (first level), during transportation (second level) and at hospital (third level) operate in a maternal death. Information on these determinants will give a better understanding of the circumstances of death. We aimed to estimate the maternal mortality ratio of Barpeta district in Assam and to understand the sociocultural factors and delays at various levels, which contribute to maternal death.Method. We did a community-based, cross-sectional study. During the surveillance period of 1 year, all maternal deaths occurring in the district were identified from multiple sources and informants. These included all deaths occurring in the health facility or in the community. In 50% of such deaths, social autopsy was conducted. The data were analysed manually for descriptive statistics and thematic areas.
Results. The maternal mortality ratio of the district is 225 per 100 000 live-births. About 95% of respondents availed antenatal services and 57% delivered in hospital. The routine maternal death surveillance system is sensitive and detected 94% of maternal deaths. However, community-based verbal autopsy is yet to be functional. Most maternal deaths occur among women from low socioeconomic conditions. Delay at the first level occurred in 10 maternal deaths, at the second level in 18 maternal deaths and at the third level in 8 maternal deaths.
Conclusions. Health-seeking behaviour is favourable and 90% of mothers sought services. Improved and functioning infrastructure will ensure better transportation facilities and early referral to a secondary- or tertiary-level health facility, which can prevent many maternal deaths.
Introduction
India has a high maternal mortality ratio (MMR). Though various national programmes have brought a steady decline in the MMR, it is slow. Maternal deaths have been described as the tip of the iceberg and maternal morbidity as the base. For every woman who dies of pregnancy-related causes, 20 others experience acute or chronic morbidity, often with permanent sequelae that undermine their normal functioning.[1]
Nearly two-thirds of maternal deaths in India are contributed by the Empowered Action Group (EAG) states and Assam. In India, maternal mortality has declined from 212 per 100 000 live-births in 2007–09 to 178 in 2010–12 and 168 in 2011–13.[2],[3] In India, Assam has the highest MMR. Any precise estimate of population MMR is not available because maternal death is a relatively rare event and will require a large sample. Though many methods are available,[4],[5] data so generated have a large confidence interval.
Scientific research on maternal mortality is focused mainly on clinical factors. However, this approach may not be the most useful if we are to understand the problem of maternal mortality as a whole and appreciate the importance of economic and social factors.[6] The United Nations Population Fund (UNPFA) has promoted the ‘3 delays model’—a framework put forth by Thaddeus and Maime.[7] It is useful for identifying the stages at which delays can occur in the management of obstetric complications. An analysis of the levels of delay--first level occurring at the household, second level occurring in the process of mobilization to a health facility and third level at the healthcare facility in providing appropriate treatment will give valuable information.
It is important to have a good system of maternal death audit/ reviews in place. The Government of India in 2010, mandated maternal death review (MDR) at the district-level across the country and published guidelines for the same.[8] However, as of March 2012, only 18% of all expected maternal deaths were being reported under the MDR process, and of these, only two-thirds were being reviewed by the district-level committee for MDR. Also, this exercise was restricted largely to finding a medical cause for death rather than identifying gaps in the health system and instituting corrective action, the original objective of the whole process.[9]
Assam has initiated MDR in all districts. This system has provided much ground-level information. However, the major source of this information is hospital statistics that do not reflect overall patterns in the community. Information on social, cultural and behavioural factors that contribute to maternal mortality is scarce. There is a need to generate local-level data to know the precise MMR; various medical and social reasons contribute to it and the levels of delay in causing maternal death and use this information for planning at the local level. We aimed to determine the MMR in the district in a 1-year period, identify the type of delay associated with these deaths and the reasons for it, and identify gaps in service delivery.
Methods
We did a community-based cross-sectional study during 2015–16. All maternal deaths in the district during the study period constituted the study sample. Any maternal death as per the definition of ICD 10 of a resident of the district was included. Social autopsy was done in 50% of maternal deaths. To ensure uniform geographical distribution, an equal number of deaths were selected from each block for verbal autopsy.
The selection of the district was based on convenience of location. Barpeta district is one of the backward districts in Assam.[10] It occupies an area of 3245 km2 and has a population of 1 693 190 (as of 2011 census).[11] It has a literacy rate of 63.8%. More than four-fifths of the population depends upon agriculture for their livelihood. The district has 11 development blocks and 840 revenue villages. Maternal health services are provided through a network of a medical college, 1 district hospital, 1 subdivisional hospital, 6 community health centres (CHCs), 8 block primary health centres (PHCs), 20 mini PHCs, 8 state dispensaries and 264 subcentres. There are 31 sites for institutional delivery in the public sector and 4 hospitals in the private sector.
We attempted to capture all female deaths in the 15–49 years age group for a period of 1 year, ascertain the maternal deaths among them and detail the circumstances of the maternal deaths. The source of such information was facility- as well as community-based.
Antenatal care (ANC) services were available at the village level in which maternal deaths took place. All the villages had accredited social health activist (ASHA) workers. Outreach sessions, in which auxiliary nurse midwife (ANM)/ASHA workers were present, were held in the villages. Adequacy of ANC was defined as 4 or more visits, with measurement of weight, blood pressure and haemoglobin during at least one of the visits.
Social autopsy
We did social autopsy, ‘an interview process aimed at identifying social, behavioural, and health system contributors to maternal and child deaths’.[12] To ensure completeness of information, family members, neighbours, health service providers mainly ASHA and anganwadi workers were also interviewed. In a few maternal deaths, the doctor who did the delivery was also interviewed after explaining the purpose of the study.
Identification of maternal death
To expand the network for reporting deaths, we used the services of independent surveillance workers. We personally interacted and networked with block development officers (BDOs) and child development programme officers (CDPOs), Integrated Child Development Scheme (ICDS) supervisor and ASHA supervisor. Members of Panchayati Raj institutions (PRIs), anganwadi workers, and supervisors of health and ICDS were sensitized at the beginning of the project. During the study period, they were sensitized in their monthly meetings and follow-up was done. Thus, the sources of maternal death reporting were: (i) surveillance worker of the project; (ii) anganwadi workers, supervisors, CDPOs of the ICDS system; (iii) PRI members; (iv) influential persons and local clubs and organizations identified by surveillance workers in their areas; and (v) routine reporting by the health system. This process was adopted to ensure completeness of maternal death reporting.
Study tool
An interview schedule was developed with inputs from the verbal autopsy tool developed by WHO, Indian Council of Medical Research and other researchers.[13],[14],[15],[16] It contained information on sociodemographic, previous obstetric, ANC in previous and current pregnancy, time of death and filters to ascertain cause, health-seeking behaviour, on levels of delay and services from ICDS.
The Kuppuswamy socioeconomic status assessment score (2014) was used.[17] For calculating MMR, the annual birth cohort in the district was considered.
A peripheral facility was a government hospital that conducts deliveries and a tertiary facility was a medical college.
Data analysis
Data were processed, coded and tabulated manually. Descriptive statistics were used. Information from in-depth interviews was analysed for thematic areas.
Permission was obtained from the institutional ethics committee.
Results
We identified 79 maternal deaths during the surveillance period in a birth cohort of 35 000 giving us an MMR of 225 per 100 000 live-births in the district. There were two additional deaths, 1 accidental and 1 suicidal. Thus, the total pregnancy-related deaths were 81. Of the 42 deaths investigated by us, in only 9 deaths community-based verbal autopsy was done by the PHCs.
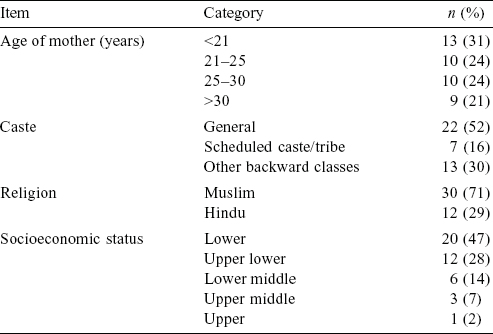
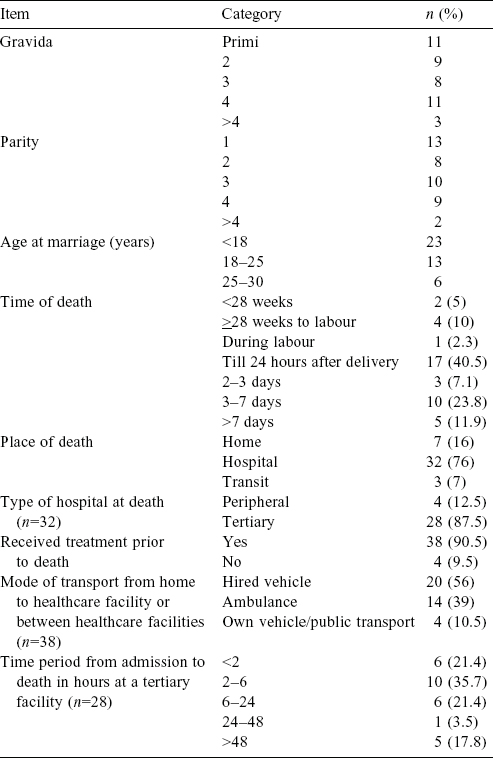
At the time of their death, 13 mothers (31%) were below 21 years of age. The level of literacy was low: 20 (47%) mothers and 27 (64%) husbands were illiterate; 34 (80%) mothers and 38 (90%) husband had <8 years of schooling [Table - 1]. In general, the husband’s level of literacy was less than that of the wife in a majority of couples. Thirty-eight mothers (90%) were housewives and the rest were engaged in petty jobs; 23 husbands (54%) were daily wage earners, 9 (21%) had petty businesses of their own, 4 were farmers and 4 were employees in government or private establishments. About 75% (32) of families were of lower socioeconomic status, 41 mothers were from rural areas and 1 from an urban area. All were residents of the district. None of the mothers who died was single, divorced or separated. Two mothers did not avail ANC services as one of them was in Delhi at the time of her pregnancy though she is a usual resident of the district and delivered in the district. The other mother was not registered at the subcentre, though she was a resident of the district and did avail of ration services from ICDS [Table - 2].
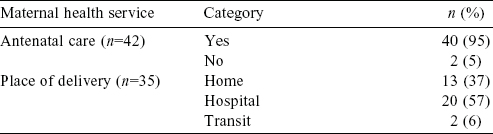
Of the 40 mothers who availed of ANC services, 7 (17%) made <3 visits, 21 (52%) made 3–5 visits and 12 (30%) made >5 antenatal visits. In 31 mothers (77%) ANC was found to be adequate. Ultrasound and blood examination was done during the ANC period in 25 (60%) maternal deaths. Only 8 (20%) mothers had consumed 100 tablets of iron-folic acid. In all pregnancies, home visits were done by ASHA at least once, though the ANM made home visits rarely.
Seven mothers died before child birth. Of the 35 mothers who delivered, 13 (37%) delivered at home, 20 (57%) delivered in hospital and 2 (6%) delivered on the way to hospital [Table - 2]. Of the hospital deliveries 10 (50%) were conducted in peripheral health facilities, 7 (35%) at tertiary health facilities and 3 (15%) in a private health facility. The private facilities were unauthorized delivery setups run by paramedical personnel to conduct deliveries at home.
Of the 7 deaths that occurred at home, 3 did not seek any treatment, 2 died at home but visited multiple facilities in the course of their delivery and 2 were brought home against medical advice. Of the 3 deaths in transit, 1 was on the way from home to the health facility and 2 on the way from a peripheral to a tertiary health facility. Four mothers did not receive any treatment—2 families did not realize the seriousness of the condition, 1 did not have money available and 1 mother died on the way from home to the hospital. Thirty-eight mothers (90.5%) received treatment before death, 7 (18%) were taken directly to peripheral health facilities, 10 (26%) were taken directly to the tertiary health facility, 3 (8%) sought services from private practitioners and 18 (47%) accessed both secondary and tertiary health facilities. Private practitioners were paramedical persons conducting delivery in their own setup at home.
In 27 maternal deaths (64%), the patient was taken to >1 health facility. In 18 maternal deaths, there was referral from peripheral to tertiary-level facilities in the district. On an average, 1–2 hours were lost in the process of referral to a tertiary facility. An analysis of deaths in tertiary facility revealed that 16 mothers (57%) died within 6 hours of admission to the medical college.
Delays
Delay at the first level could be identified in 10 maternal deaths. The reasons were: (i) seriousness of condition not realized in 2; (ii) attempts at traditional methods for removal of retained placenta in 3; and (iii) 5 were observed at home.
Delay at the second level was identified in 18 maternal deaths. It was mainly due to non-availability of a government ambulance and time needed to hire a vehicle. The district is flood-prone and in such a season accessibility of roads due to flood also interfered with early mobilization.
Delay at the third level at a peripheral facility. This occurred in 5 instances. These were (i) prolonged labour in 1; (ii) normal delivery attempted in known breech presentation in 1; (iii) normal delivery attempted despite a history of per vaginal bleeding on previous occasions in the index pregnancy in 1; and (iv) delayed referral of women with postpartum hemorrhage in 2.
Delay at the third level at a tertiary facility. These included (i) non-availability of O-negative blood at the blood bank in 2; and (ii) sepsis-related death due to prolonged labour in 1.
Discussion
During the surveillance period, we identified 79 maternal deaths and an MMR of 225 per 100 000 live-births, while the web-based MDR reporting system reported 74 maternal deaths in the district. In Assam, the MMR was estimated to be 300 as per the Sample Registration System 2011–13[2],[3] while the Regional Resource Centre-North East (RRC-NE) 2009–2010[18] estimated it to be 333. There was a discrepancy between our study and the MDR system of 5 maternal deaths. Thus, the routine MDR system could identify most (94%) maternal deaths in the district and could be said to be functioning satisfactorily.
The facility- and community-based audit of maternal deaths is conducted by the department of health in the district. We conducted social autopsies in 42 of the 79 maternal deaths. Of the 42 deaths, in only 9 (20%) community-based verbal autopsy had been done. Also, the process of MDR at various levels was cursory and MDR meetings were not held regularly in the district. Though identification of maternal deaths was nearly complete, the MDR process was not fully functional. Other researchers too have made similar observations.[9],[19],[20] Initiating a confidential inquiry into maternal deaths can supplement and strengthen the process.[21],[22]
Most maternal deaths were among those with low levels of literacy and poor socioeconomic strata. The Census of India 2011 reported 69% male literacy, 58% female literacy and 7% scheduled caste/tribe population in the district.[11] A high maternal mortality in marginalized populations has been reported by others as well.[23],[24],[25],[26] Despite a social disadvantage, 90% of mothers sought medical services, when a complication arose.
The district has a wide network of human resource and infrastructure for providing maternal health services. ANC services are widely accessed by mothers (97%). However, intranatal services are sought less frequently as is evident by one-third of deliveries occurring at home during the index pregnancy. The district reported an institutional delivery rate of 45% as per the Annual Health Survey (AHS) 2011. The AHS 2012 reports 55% and the Health Management Information System (HMIS) (April to September 2014) reported 30% home deliveries in the district. The reasons for home delivery are mostly sociocultural. While conducting verbal autopsy, Muslim families preferred home delivery. Sociocultural factors have been highlighted by other reports too.[20],[27] Since the ANC is close to home, women accepted the services and can be motivated by ASHAs to avail services.
With wider availability and accessibility of ANC, the focus should shift from coverage to quality of care. Anaemia and pregnancy-induced hypertension are major causes of maternal mortality in Assam.[28],[29],[30] We also observed these factors. Good quality ANC should be able to avoid many maternal deaths. The quality parameters of ANC can vary. In our study, 77% of mothers fulfilled the requirements of an adequate ANC. However, during the verbal autopsy process, the investigator could identify risk factors in 50% of maternal deaths. Documented haemoglobin and blood pressure points to the same values, which may be coincidental or false. In 66% of cases of pregnancy, ultrasound was done at private facilities as per the doctor’s advice or at ASHA’s own initiative. ASHAs were convinced of the need of an ultrasound in pregnancy and felt it to be an important intervention such as tetanus toxoid (TT) injection or iron-folic acid tablet. The AHS (2011) Assam report for the district reported that 37% of mothers went for ultrasonography, 35% of women had 3 or more ANC visits and 12% of mothers had full check-up.
We identified 1 accidental death due to burns and another suicidal death. Accidents or suicides among pregnant women within 42 days of delivery have been classified as being incidental to the pregnant state. However, increasing evidence suggests that such deaths might, at least in part, be caused by the pregnancy.[31],[32]
History of domestic violence was reported in 1 maternal death. This may not reflect the actual situation as we did not include this aspect in the study instrument. A previous study from India has reported a high incidence of domestic violence in pregnancy.[33]
In the maternal deaths studied by us, nearly one-third of mothers were below 21 years of age and 6 (14%) were teenage pregnancies. The AHS 2011 reported 4.4% teenage marriages and all deaths among Muslim women. About 50% of maternal deaths were among women 20–25 years of age; similar observations were made by others.[3],[34],[35] In 74% of cases, maternal death occurred in women 30 years of age or less. Gravida 1 and 2 comprised 50% of deaths. However, there are considerable high-order pregnancy deaths; 30% of maternal deaths were 4th order gravida and more and 45% maternal deaths were 3rd and 4th order parity or more. Lower gravida and higher parity deaths were also reported by others.[35] This implies the need for strengthening family planning services in the district. We identified 1 illegal abortion-related death due to insertion of a local herb. The mother died of septicaemia after a period of 10 days after consulting a private practitioner and the medical college.
Nearly half (18, 43%) of maternal deaths took place in the intranatal period (beginning of labour to 24 hours of delivery) and half (21, 50%) occurred within 48 hours of delivery. This re-emphasizes the need for a 48-hour stay in an institution following delivery. Analyses of deaths worldwide have shown that most maternal deaths cluster around labour, delivery and the immediate postpartum period.[3],[24],[26],[27]
In the event of a maternal complication, 38 (90%) families sought treatment—an observation much higher than other studies.[26],[33],[34],[35] Given the sociodemographic background of maternal deaths, delay was expected and identified in 10 (24%). The time of death also supports such an observation; 26% (11/42) died within 6 hours of onset of the complication leaving little time for intervention—30% died within 2 hours and 61% within 24 hours of hospital admission. Though 16% (7) of deaths occurred at home, only 3 did not seek any health service. Thus, it can be concluded that social factors do not operate against treatment-seeking behaviour as hypothesized, but contribute to delay at the first level.
Three-fourths of the deaths (76%; 32) were at a health facility. The district has a network of 31 sites of institutional delivery, of which only 6 function round the clock. Of the institutional deaths, 4 deaths (12.5%) occurred at a peripheral facility and 28 (87.5%) at a tertiary facility. In 18 maternal deaths, there was a referral pathway from the peripheral to the tertiary facility. Though there is a network of ambulance services including those exclusively for pregnant women, 56% were transported in hired vehicles due to non-availability of government vehicles. Delay due to transportation were reported by other studies also.[24],[33] Availability of 102/108 ambulances was limited and this issue was highlighted by ASHAs; they also said that some of the PHC ambulance drivers charged for transportation services especially at night.
The process of mobilizing private vehicles took 1–2 hours, contributing to delay at the second level. Analyses of the pattern of death in the tertiary facility showed that 54% of mothers died within 6 hours of admission. Thus, peripheral facilities were not equipped to handle emergencies. It is evident that there is delay at two levels and this cumulatively prolonged the critical time of intervention in a maternal emergency. As peripheral facilities are not equipped to handle emergency cases, referral of maternal emergencies to peripheral facilities will unnecessarily prolong the critical time of intervention.
We identified 3 maternal deaths at private facilities supervised by paramedical workers (ANM). We could identify 3 such facilities during the study. However, there may be many such unauthorized setups given the sociodemographic background of the district and preference for delivery by female service providers.
Though conceptually 3 levels of delay are identified in an adverse maternal outcome, there may be an overlap among these. Many studies have reported delays at the health facility level.[19],[26],[33],[34],[35] We too noticed delays at the secondary-level health facility. Despite 31 institutional delivery sites, only 4 operated round the clock but were not equipped to handle complications. Delays at the third level were difficult to identify with our study methodology but there were 2 maternal deaths due to non-availability of blood of a specific type at the facility and 1 sepsis-related death following caesarean section done at the facility. Maternal death is a risk factor for neonatal and infant death. In our study, only 50% of children born were surviving at the time of social autopsy. Many researchers[33],[36] have reported a high mortality rate among infants whose mothers have died.
Conclusion
Analyses of the causes of maternal mortality at the district level provide information that could help prevent delays at the second and third level. This information can be provided by the MDR system. While social and cultural factors influenced accessing routine maternal services, these were not the key factors in seeking emergency care.
Acknowledgement
We acknowledge Srimanta Sankaradeva University of Health Sciences, Assam for funding this project.
| 1. | Firoz T, Chou D, von Dadelszen P, Agrawal P, Vanderkruik R, Tunçalp O, et al.; Maternal Morbidity Working Group. Measuring maternal health: Focus on maternal morbidity. Bull World Health Organ 2013;91:794-6. [Google Scholar] |
| 2. | Sample Registration System (SRS). Maternal Mortality Ratio Bulletin 2011-13 and A Presentation on Maternal and Child Mortality and Total Fertility Rates (07-07-2011). Available at www.censusindia.gov.in/2011-Common/Sample_Registration_ System.html (accessed on 1 Jan 2017). [Google Scholar] |
| 3. | An analysis of levels and trends in maternal health and maternal mortality ratio in India 2015. A report. New Delhi:National Institute of Public Cooperation and Child Development; 2015 [Google Scholar] |
| 4. | Bhat PN, Navaneetham K, Rajan SI. Maternal mortality in India: Estimates from a regression model. Stud Fam Plann 1995;26:217-32. [Google Scholar] |
| 5. | Hanley JA, Hagen CA, Shiferaw T. Confidence intervals and sample-size calculations for the sisterhood method of estimating maternal mortality. Stud Fam Plann 1996; 27:220-7. [Google Scholar] |
| 6. | Gil-González D, Carrasco-Portiño M, Ruiz MT. Knowledge gaps in scientific literature on maternal mortality: A systematic review. Bull World Health Organ 2006;84:903-9. [Google Scholar] |
| 7. | Thaddeus S, Maine D. Too far to walk: Maternal mortality in context. Soc Sci Med 1994;38:1091-110. [Google Scholar] |
| 8. | Maternal Health Division, Ministry of Health and Family Welfare. Maternal death review guidebook. New Delhi:Ministry of Health and Family Welfare, Government of India; 2011 [Google Scholar] |
| 9. | Malhotra M. Maternal death review—Country perspective: Presentation at WHO multicountry workshop. Bangkok, Thailand, 24-28 September 2012. New Delhi:Deputy Commissioner, Maternal Health, MoHFW, Government of India; 2012. [Google Scholar] |
| 10. | Census report for Barpeta district. Office of the Census Commissioner. Govt of India. [Google Scholar] |
| 11. | Baseline survey of minority concentrated districts, District report, Barpeta. Study Commissioned by Ministry of Minority Affairs. Government of India. [Google Scholar] |
| 12. | Kalter HD, Salgado R, Babille M, Koffi AK, Black RE. Social autopsy for maternal and child deaths: A comprehensive literature review to examine the concept and the development of the method. Popul Health Metr 2011;9:45. doi: 10.1186/14787954-9-45. [Google Scholar] |
| 13. | Waiswa P, Kalter HD, Jakob R, Black RE; Social Autopsy Working Group. Increased use of social autopsy is needed to improve maternal, neonatal and child health programmes in low-income countries. Bull World Health Organ 2012;90:403- 403A. doi: 10.2471/BLT.12.105718. [Google Scholar] |
| 14. | Campbell O, Ronsmans C, World Health Organization, Maternal health and safe motherhood programme. Verbal autopsies for maternal deaths. London:WHO; 1995. Available at http://www.who.int/iris/handle/10665/61029 (accessed on 1 Jan 2017). [Google Scholar] |
| 15. | Joshi R, Kengne AP, Neal B. Methodological trends in studies based on verbal autopsies before and after published guidelines. Bull World Health Organ 2009;87:678-82. [Google Scholar] |
| 16. | Institute for Research in Medical Statistics, Indian Council of Medical Research. Estimates of maternal mortality ratios in India and its states. A pilot study. New Delhi:Department of Family Welfare, Ministry of Health and Family Welfare; 2003. [Google Scholar] |
| 17. | Oberoi SS. Updating income ranges for Kuppuswamy’s socio-economic status scale for the year 2014. Indian J Public Health 2015;59:156-7. doi: 10.4103/0019- 557X.157540. [Google Scholar] |
| 18. | MMR and IMR Survey report Assam 2009. Survey conducted by Regional Resource Centre for North East States, Ministry of Health and Family Welfare, Government of India. [Google Scholar] |
| 19. | Padmanaban P, Raman PS, Mavalankar DV. Innovations and challenges in reducing maternal mortality in Tamil Nadu, India. J Health Popul Nutr 2009;27:202-19. [Google Scholar] |
| 20. | Kalter HD, Mohan P, Mishra A, Gaonkar N, Biswas AB, Balakrishnan S, et al. Maternal death inquiry and response in India—the impact of contextual factors on defining an optimal model to help meet critical maternal health policy objectives. Health Res Policy Syst 2011;9:41. [Google Scholar] |
| 21. | Knight M, Kenyon S, Brocklehurst P, Neilson J, Shakespeare J, Kurinczuk JJ (eds.) on behalf of MBRRACEUK. Saving Lives, Improving Mothers’ Care—Lessons learned to inform future maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2009—12. Oxford:National Perinatal Epidemiology Unit, University of Oxford; 2014. [Google Scholar] |
| 22. | Paily VP, Ambujam K, Rajasekharan Nair V, Thomas B. Confidential review of maternal deaths in Kerala: A country case study. BJOG 2014;121 Suppl 4:61-6. [Google Scholar] |
| 23. | Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: A systematic review. Lancet 2006;367:1066-74. [Google Scholar] |
| 24. | Iyengar SD, Iyengar K, Gupta V. Maternal health: A case study of Rajasthan. J Health Popul Nutr 2009;27:271-92. [Google Scholar] |
| 25. | Kumar S. Reducing maternal mortality in India: Policy, equity, and quality issues. Indian J Public Health 2010;54:57-64. [Google Scholar] |
| 26. | Gabrysch S, Campbell OM. Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy Childbirth 2009;9:34. doi: 10.1186/1471-2393-9-34. [Google Scholar] |
| 27. | Warren C, Mekbib T. Reviewing maternal mortality in rural Ethiopia: using the verbal autopsy approach. Ethiopian J Reprod Health 2009;3:4-14. [Google Scholar] |
| 28. | Swasthya Sanbad. Quarterly National Rural Health Mission Newsletter from Assam. Vol 6, Issue 2:13 [Google Scholar] |
| 29. | HMIS 2012-13 Assam, National Health Systems Resource Center. Available at http://nhsrcindia.org/hmis-details/hmis-analysis-2012—13/NjQ4 (accessed on 1 Jan 2017). [Google Scholar] |
| 30. | HMIS 2013-14 Assam, National Health Systems Resource Center. Available at http://nhsrcindia.org/hmis-details/hmis-analysis-2013—14/NjQ1 (accessed on 1 Jan 2017). [Google Scholar] |
| 31. | Fauveau V, Blanchet T. Deaths from injuries and induced abortion among rural Bangladeshi women. Soc Sci Med 1989;29:1121-7. [Google Scholar] |
| 32. | Ronsmans C, Khlat M. Adolescence and risk of violent death during pregnancy in Matlab, Bangladesh. Lancet 1999;354:1448. [Google Scholar] |
| 33. | Ganatra BR, Coyaji KJ, Rao VN. Too far, too little, too late: A community-based case-control study of maternal mortality in rural west Maharashtra, India. Bull World Health Organ 1998;76:591-8. [Google Scholar] |
| 34. | Montgomery AL, Ram U, Kumar R, Jha P; Million Death Study Collaborators. Maternal mortality in India: Causes and healthcare service use based on a nationally representative survey. PLoS One 2014;9:e83331. [Google Scholar] |
| 35. | Subha Sri B, Khanna R. Dead women talking: A civil society report on maternal deaths in India. CommonHealth and Jan Swasthya Abhiyan, 2014. [Google Scholar] |
| 36. | Saleem S, McClure EM, Goudar SS, Patel A, Esamai F, Garces A, et al.; Global Network Maternal Newborn Health Registry Study Investigators. A prospective study of maternal, fetal and neonatal deaths in low- and middle-income countries. Bull World Health Organ 2014;92:605-12. [Google Scholar] |
Fulltext Views
2,308
PDF downloads
591




