Translate this page into:
The national licentiate examination: Pros and cons
2 Department of Paediatrics and Medical Education, Christian Medical College, Ludhiana 141008, Punjab, India
Corresponding Author:
Tejinder Singh
Department of Paediatrics and Medical Education, Christian Medical College, Ludhiana 141008, Punjab
India
drtejinder22@gmail.com
| How to cite this article: Mahajan R, Singh T. The national licentiate examination: Pros and cons. Natl Med J India 2017;30:275-278 |
Abstract
A multiple choice-based National Eligibility-cum-Entrance Test for admission to postgraduate courses (NEET-PG) for 201 7 was conducted by the National Board of Examinations of India. It was widely reported in the media and through gazette notifications that the government is going to use this NEET examination as a licentiate examination in the near future. Medical students will be certified to practise in India only if they qualify in this examination. We discuss the pros and cons of such an end-of-term examination, its utility and educational impact besides proposing a comprehensive framework for implementing formative assessment in medical colleges.
Introduction
Newspapers in 2016–17 were rife with reports that the Government of India (GoI) was going to introduce a National Licentiate Examination (NLE), nicknamed as ‘Exit Examination’, for MBBS graduates so as to certify them to practise medicine in India.[1] In 2017, the National Board of Examinations conducted the National Eligibility-cum-Entrance Test for postgraduate courses (NEET-PG), as a single-window entrance examination for postgraduate seats in government medical colleges, private institutes, and Diplomate of National Board (DNB) Broad Specialties.[2] As per reports, GoI was contemplating to broaden the scope of NEET-PG to serve three purposes: (i) an eligibility test for admission to postgraduate courses across all medical colleges in India; (ii) a NLE; and (iii) a replacement for the existing Foreign Medical Graduate Examination (FMGE), a Medical Council of India (MCI) screening test to assess the eligibility of Indian nationals holding medical degrees from foreign countries and intending to practise in India.[1]
The draft of the National Medical Commission Bill (NMCB) by the NITI Aayog made things clearer.[3] The proposed bill has been drafted as per the ‘Preliminary Report of the Committee on the Reform of the Indian Medical Council Act, 1956’, based upon the 92nd Report of the Parliamentary Standing Committee.[4] The draft bill proposes to scrap the MCI and replace it with the National Medical Commission (NMC). The draft bill states: ‘There shall be a National Licentiate Examination for the professionals graduating from the medical institutions under the purview of National Medical Commission through such designated authority in such manner as may be prescribed for granting the licence to practise and enrolment into the Medical Register(s), as referred to in Section 28(1). The designated authority shall ensure the conduct of a uniform licentiate examination in the aforesaid manner. The National Licentiate Examination shall also serve as a National Eligibility-cum-Entrance Test for admission to postgraduate courses in medical colleges/institutions under the purview of National Medical Commission.'
What is a Licentiate Examination
Licentiate is the title of a person who holds an academic degree known as a licence.[5] The term is derived from the medieval Latin word licentiatus, which means ‘having freedom’. The word is used in phrases licentia docendi meaning permission to teach and licentia adpracticandum signifying someone who is competent to practice a profession. Many countries have degrees with this title representing different levels of education. In some universities it is a degree between that of a bachelor's and a master's or doctorate; in some countries it is comparable to a doctorate of philosophy.[5]
In many countries, the licentiate examination is a requirement before one is eligible to practise medicine in the country. In Canada, a physician who meets certain criteria, is enrolled in the Canadian Medical Register as a Licentiate of the Medical Council of Canada (LMCC) and receives a Certificate of Registration. The LMCC is not a licence to practise medicine, but a requirement to gain an independent licence to practice in Canada.[6] In the USA, the medical licensing examination is conducted before a physician can practise medicine in the USA.[7] Licentiate examinations were also prevalent in England, Scotland and Ireland till 1999.
The assessment during these examinations for granting licence to practise medicine is not solely knowledge-based using multiple-choice questions (MCQs). It is a combination of assessing knowledge, skills, attitudes, communication via objective structured clinical examination (OSCE) and standardized patients.[7],[8]
A Licentiate Examination
Arguments in favour
In India, a licentiate examination for medical graduates is being proposed because of concerns being raised over the poor quality of graduate doctors. In the past decade, there has been a boom in the number of private medical institutes in India. At the last count, there were 426 medical colleges in India, more than half of which were in the private sector.[9] Questions have been raised over the admission process, quality of education provided and evaluation process used by private medical colleges. The results indicate a big difference between the pass percentage in government and private colleges, as well as in different states in the All-India Post-Graduate Medical Entrance Examination (AIPGMEE).
For instance, the AIPGMEE 2014 results showed that based on the 50% score as minimum qualifying criteria, 22 802 candidates from government institutions passed the examination, compared to a mere 8862 candidates from private medical colleges. From foreign institutions, only 1188 passed. Similarly, the result of AIPGMEE 2015 showed that Andhra Pradesh had an average pass percentage of 84.9%, Chandigarh 73.6% while West Bengal and Uttar Pradesh had 53.6% and 51.6%, respectively. The pass percentage in Assam, Jammu and Kashmir and in foreign institutes was even lower at 46.4%, 37.8% and 31.4%, respectively.[10] As per regulatory body officials, the performance of graduates in AIPGMEE is an indicator of the quality of doctors being produced, although it can also be argued that performance in MCQ-based tests depends, in addition to knowledge, on the educational environment. Students from metropolitan and larger cities with access to ‘coaching in cracking the examination’ are likely to score better.
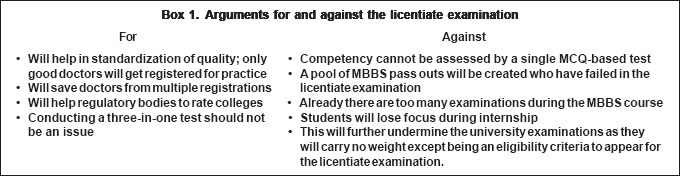
It is believed that a licentiate examination will bring uniformity and quality in medical education, as all MBBS students passing from a government or private medical college or from a foreign university will have to pass the licentiate examination before being able to practise in India. Hence, their skills will be standardized, and only those with requisite skills and knowledge will be allowed to practise medicine.[11] It is stated that this licentiate examination will also help regulatory bodies to rate medical colleges[11] [Box 1]. At best, it is a one-sided argument which ignores the overall process of knowledge and skill acquisition and the role of a hidden curriculum in motivating students the way they learn.
Arguments against
The licentiate examination, on the other hand, is being criticized on the ground that practical knowledge holds the key in MBBS training.[11] How far a single MCQ-based test will be able to assess practical knowledge and competency is doubtful. While we are contemplating to introduce competency-based medical education (CBME) at the undergraduate level in medical training through draft guidelines on graduate medical education, 2012,[12] we are also toying with the idea of an MCQ-based single licentiate examination for assessing eligibility of MBBS pass outs for granting permission to practise in India [Box 1]. One of the functions of the Undergraduate Medical Education Board (UGMEB), as stated in the NMCB, is: ‘To develop a competency-based dynamic curriculum (including assessment) at the undergraduate level in consultation with stakeholders so that medical graduates have appropriate knowledge, skills, attitude, values and ethics for providing healthcare, as per the societal needs.‘[3] It is questionable how far the assessment method based solely on MCQs will be aligned with the stated objectives.
Another debatable issue is the fate of those who pass the MBBS examination but fail to get the minimum prescribed percentile in the licentiate examination.[11] With the introduction of a licentiate examination, there might be a pool of medical graduates with valid degrees from colleges recognized by the MCI who will not be able to practise as they have not been able to pass the licentiate examination.[13] What will the government do for them? Will their efforts of five and half years in passing MBBS go in vain? No roadmap to tackle this situation has been proposed.
Other strong arguments against the licentiate examination are: as there are already too many tough internal tests and university examinations during the MBBS course, the licentiate examination may deter students from paying attention to acquire and sharpen their clinical skills during internship; they already lose focus so as to prepare for postgraduate entrance examinations; and it will put more pressure on medical students.
Utility of Licentiate Examination
Procedural and legal issues have already been raised against the NEET, the flagship postgraduate entrance examination which will also serve the purpose of the licentiate examination.[14] Instead of going into those arguments, we will focus on the utility of such an examination.
It has been established that for any assessment to be useful, it must be aligned with the instructional strategies and learning objectives.[15] As discussed above, a single MCQ-based test will never fully assess the skills, attitudes, values and ethics of medical graduates, and will be restricted to assess only the cognitive domain. Such a licentiate examination will never meet the learning objectives.
Like any assessment, we must confirm what is and will be the utility of the licentiate examination. Utility of any assessment depends on five main attributes, viz. validity, reliability, acceptability, feasibility and educational impact.[16] Although each of these attributes is important, a low value in one attribute can be compensated by a higher value in another attribute.[17] As an example, a low reliability can be compensated with a very high educational impact. However, in the case of the proposed licentiate examination, validity will be under the scanner as assessment is not going to address the objectives, making it unfit for the purpose. Similarly, it may have zero or negative educational impact as it may hinder learning by distracting students away from developing good attitudes and skills. So, the overall utility will practically be zero or even negative as far as learning is concerned [Figure - 1].
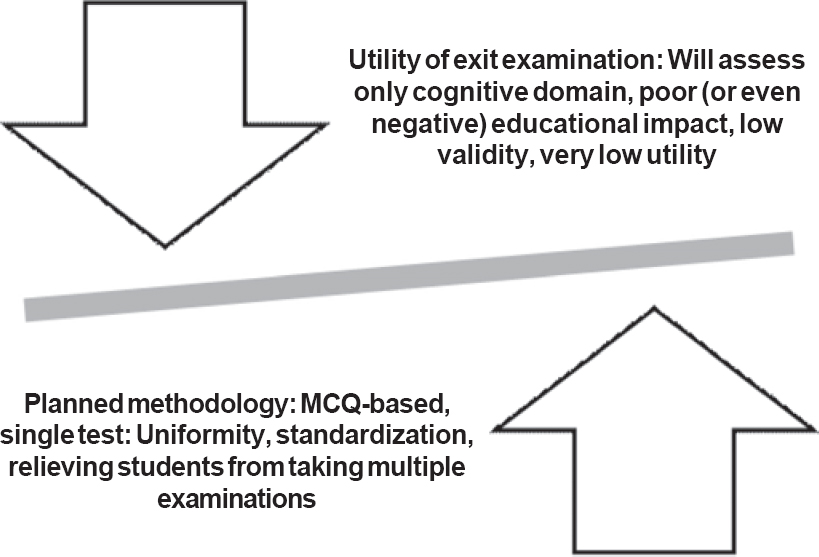 |
| Figure 1: Potential imbalance between utility and methodology of the proposed licentiate examination |
Swot Analysis of Proposed Licentiate Examination
A SWOT analysis is an evaluation of internal strengths and weaknesses, its opportunities for development, and the threats the external environment presents to its survival. A SWOT analysis is a precursor to strategic planning, so as to balance an intervention with the external environment and to maintain that balance over time.[18] The SWOT analysis of the proposed licentiate examination is given in [Box 2].
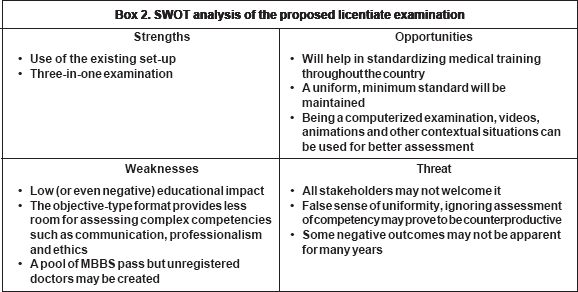
Evidently, the odds are against the licentiate examination, with threats which may arise from stakeholders, particularly MBBS graduates. More importantly, with low educational impact, the licentiate examination will be unable to differentiate between a competent and a not-so-competent doctor. All students with marks above the cut-off in an objective and theoretically conducted examination will be registered as physicians, thus jeopardizing the efforts to impart practical knowledge.
The Solution: Our Proposal
A summative assessment in the garb of a licentiate examination as a prerequisite for registration, at the end of MBBS course, suggests as if it has been designed to identify graduates who are not fit to practise. If we consider this situation from a manufacturer's point of view, the purpose of end inspection is to weed out products that do not meet the required quality standards, but no manufacturer will simply discard all the defective products. Rather, there is a need to have multiple intermediary inspections so that necessary corrective changes in the input and process can be made. The rationale of the licentiate examination, i.e. poor quality of training being imparted in some institutes and the proposed solution, seems to hit fault lines and divergent targets. The underlying assumption is that students have been certified fit by internal/university examinations and now only the best have to be selected. The licentiate examination goes contrary to this assumption by trying to identify students who are not fit. All efforts seem to be directed towards sieving good (presumed competent) MBBS graduates from not-so-good graduates, without making any effort to improve the standards during the training period itself.
We propose that focusing on skills development, faculty development and in-course assessment is more important than a licentiate examination alone as an input to maintain quality. Paradoxically, the licentiate examination will end up further weakening the present medical education system and promote only knowledge-based learning at the cost of skills, attitudes and communication—so crucial for success as a physician. Considering that our admission process aims to include the poor and the marginalized, the need to improve formative aspects of assessments becomes all the more important. Even in countries such as the USA with a long experience of conducting various formats of licentiate examinations, voices of dissent have become louder to reduce the dependence on such examinations. People opine that such exit/licentiate examinations do not allow teaching and training to be targeted to the health needs of the population and leave less scope for innovation.[19] Formative or in-course assessments stand out as useful tools to provide the much needed feedback as an input for better learning, as highlighted by Hattie's meta-analysis.[20],[21]
The importance of formative assessment in undergraduate medical education for mid-course remedial purposes has been emphasized by the Liaison Committee on Medical Education.[22] Konopasek et al. have also suggested that such a formative assessment should be part of an ongoing process, and should be interwoven with summative assessment. They further advocated that such a process should create information which should be assimilated in a continuous cycle over time, named as plan–do–study–act (PDSA) cycle.[23]
The literature has documented two types of student orientations for assessment—performance and learning orientation. In the former, students aim to ‘look good’ and tend to hide errors and consider feedback as a punitive action; while in the learning orientation the goal of the learner is to improve and they welcome the feedback.[24],[25] For feedback to be effective, we must develop a culture where learning orientation can thrive.
The proposed framework must have sufficient encounters of self-assessment, reflections and workplace-based assessment. Further, faculty development and learners’ development must be essential components of this framework [Figure - 2].
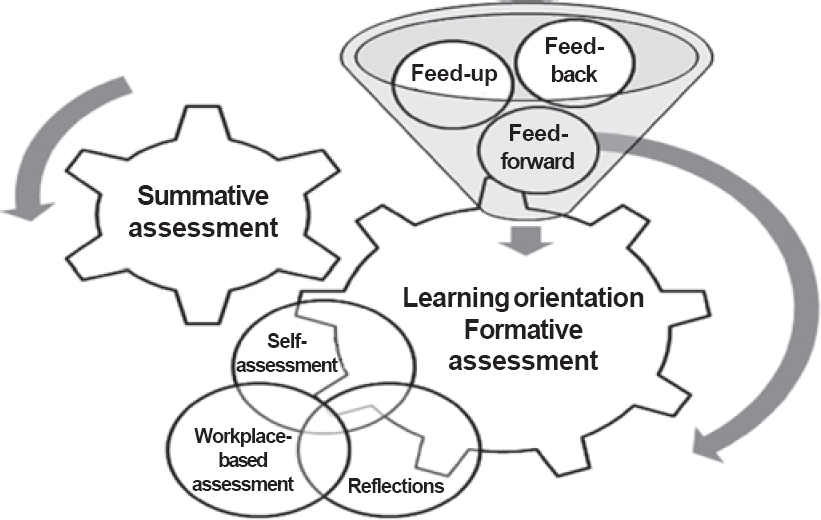 |
| Figure 2: Essential components of a comprehensive framework for medical student assessment |
Conclusion
The intent of a licentiate examination is not in doubt but it will be a mistake to put too many stakes on only one intervention. We must realize that many competencies that are vital for successful practice of medicine are not amenable to assessment by highly objective and one end-of-the-course examination. Instead of ad hoc arrangements, we should strengthen our existing assessment systems with continuous and structured formative assessment incorporating objective and specific feedback instruments, which will go a long way in improving the standards of our medical education.
Licentiate/exit examinations can be a useful intervention provided we focus simultaneously on strengthening our incourse assessments, include formative feedback, and provide opportunities for training of skills, communication and attitudes in the medical curriculum so as to give students ample time for mid-course correction.
| 1. | Singh MK. Govt plans exit exams for all MBBS students. TNN 27 July 2016. Available at http://timesofIndia. Indiatimes. com/India/Govt-plans-exit-exam-for-all-MBBS-students/articleshow/53406483.cms (accessed on 27 Aug 2016). [Google Scholar] |
| 2. | National Board of Examinations. National Eligibility cum Entrance Test (NEET-PG): Scope of NEET-PG 2017. Available at http://nbe.edu.in/neetpg/about-neetpg.html (accessed on 22 Dec 2016). [Google Scholar] |
| 3. | Niti Aayog. The proposed bill—The National Medical Commission Bill, 2016. Available at http://niti.gov.in/writereaddata/files/new_initiatives/MCI%20Bill %20Final.pdf (accessed on 27 Aug 2016). [Google Scholar] |
| 4. | Medical Dialogues. National Medical Commission to replace MCI, NITI Aayog panel asks for comments; 10 August 2016. Available at http://medical dialogues.in/mci-replacement-niti-ayog-invites-public-comments-on-national-medical-commission-bill-2016/ (accessed on 27 Aug 2016). [Google Scholar] |
| 5. | Oxford Dictionaries. Definition of Licentiate. Available at www. oxford dictionaries.com/definition/english/licentiate?region=uk&q=Licentiate (accessed on 27 Aug 2016). [Google Scholar] |
| 6. | Medical Council of Canada. Licentiate of the Medical Council of Canada. Available at http://mcc.ca/about/lmcc/ (accessed on 27 Aug 2016). [Google Scholar] |
| 7. | Melnick DE, Dillon GF, Swanson DB. Medical licensing examinations in the United States. J Dent Educ 2002;66:595-9. [Google Scholar] |
| 8. | Reznick R, Smee S, Rothman A, Chalmers A, Swanson D, Dufresne L, et al. An objective structured clinical examination for the licentiate: Report of the pilot project of the Medical Council of Canada. Acad Med 1992;67:487-94. [Google Scholar] |
| 9. | Medical Council of India. List of colleges teaching MBBS. Available at www.mciIndia.org/InformationDesk/ForStudents/ListofCollegesTeaching MBBS.aspx (accessed on 27 Aug 2016). [Google Scholar] |
| 10. | Dey S. Govt plans exit exams for MBBS doctors.TNN; 1 June 2015. Available at http://timesofIndia.Indiatimes. com/India/Govt-plans-exit-exam-for-MBBS-doctors/articleshow/47494308.cms (accessed on 27 Aug 2016). [Google Scholar] |
| 11. | Bhatnagar S. The unending debate over ‘Exit Test’ after MBBS. Exams watch, debate corner, Education News, 24 June 2016. Available at http://examswatch. com/the-unending-debate-over-exit-test-after-mbbs/ (accessed on 27 Aug 2016). [Google Scholar] |
| 12. | Medical Council of India. Regulations on Graduate medical Education, 2012. Available at www.psgimsr.ac.in/wp-content/uploads/2012/pdf/others/mci-regulations-graduate-medical-education-12.pdf (accessed on 27 Aug 2016). [Google Scholar] |
| 13. | Medicos slam exit exam for MBBS pass-outs. TNN, Chandigarh; 27 August 2014. Available at http://timesofIndia. Indiatimes. com/city/chandigarh/Medicos-slam-exit-exam-for-MBBS-pass-outs/articleshow/40951827. cms (accessed on 27 Aug 2016). [Google Scholar] |
| 14. | Dhavan R. Medical Council's NEET: Unfair, unjust, arbitrary. The Wire 16 May 2016. Available at http://thewire.in/36274/mcis-neet-unfair-unjust-arbitrary/ (accessed on 2 Sep 2016). [Google Scholar] |
| 15. | Anderson LW. Curricular alignment: A re-examination. Theory Practice 2002;41:255-60. [Google Scholar] |
| 16. | van der Vleuten CPM, Schuwirth LWT. Assessing professional competence: From methods to programmes. Med Educ 2005;39:309-17. [Google Scholar] |
| 17. | van der Vleuten CPM, Norman GR, De Graaff E. Pitfalls in the pursuit of objectivity : Issues of reliability. Med Educ 1991;25:110-18. [Google Scholar] |
| 18. | Harrison JP. Strategic planning and SWOT analysis. In: Harrison JP (ed). Essentials of strategic planning in health care. Chicago, IL:Health Administration Press; 2010:91-7. [Google Scholar] |
| 19. | Gliatto P, Leitman M. Muller D. Scylla and Charybdis: The MCAT, USMLE, and degrees of freedom in Undergraduate medical education. Acad Med 2016;91: 1498-500. [Google Scholar] |
| 20. | Hattie J. Influences on student learning. Inaugural lecture: Professorial Address, University of Auckland, New Zealand; 1999. Available at http://projectlearning. org/blog/wp-content/uploads/2014/02/Influences-on-Student-Learning-John-Hattie.pdf (accessed on 22 Sep 2016). [Google Scholar] |
| 21. | Hattie J, Timperley H. The power of feedback. Rev Educ Res 2007;77:81-112. [Google Scholar] |
| 22. | Liaison Committee on Medical Education. Functions and structure of a medical school: Standards for accreditation of medical school programs leading to the M.D. degree. March 2016. Available at www.lcme.org/publications (accessed on 23 Sep 2016). [Google Scholar] |
| 23. | Konopasek L, Norcini J, Krupat E. Focusing on the formative: Building an assessment system aimed at student growth and development. Acad Med 2016;91:1492-7. [Google Scholar] |
| 24. | Dweck C. Self-theories: Their role in motivation, personality, and development. Philadelphia, Pa:Taylor Francis/Psychology Press; 2013. [Google Scholar] |
| 25. | Mangels JA, Butterfield B, Lamb J, Good C, Dweck CS. Why do beliefs about intelligence influence learning success? A social cognitive neuroscience model. Soc Cogn Affect Neurosci 2006;1:75-86. [Google Scholar] |
Fulltext Views
4,100
PDF downloads
1,451




