Translate this page into:
Thoracic splenosis: A curious case of thoracic masses
Correspondence to Bhaveshwar Vihar, 383 Sardar V.P. Road, Mumbai 400004, Maharashtra, India; bhavin@jankharia.com
To cite: Jankharia B. Thoracic splenosis: A curious case of thoracic masses. Natl Med J India 2022;35:93–4.
Abstract
An asymptomatic patient from another country, with a past history of an abdominal gunshot wound and splenic rupture, treated 20 years ago, presented with thoracic masses. It was possible to make the diagnosis of thoracic splenosis, after reviewing the history, the imaging findings and the final histopathology report, without subjecting the patient to surgery.
INTRODUCTION
Splenic rupture is known to lead to fragments of splenic tissue spreading within the thorax and the abdomen, remaining stable or growing minimally and usually presenting many years later with a diagnostic conundrum.1–4 This is one such case.
THE CASE
A 45-year-old man from a troubled African nation was referred on an urgent basis for a computed tomography (CT)-guided biopsy of ‘masses’ in the chest. Since he carried no prior imaging and reports, a CT scan was first performed, which showed multiple homogeneously enhancing extrapleural lesions in the left hemithorax, larger and more numerous superiorly (Fig. 1). The differential diagnosis included neurogenic tumours, mesothelioma and metastases.
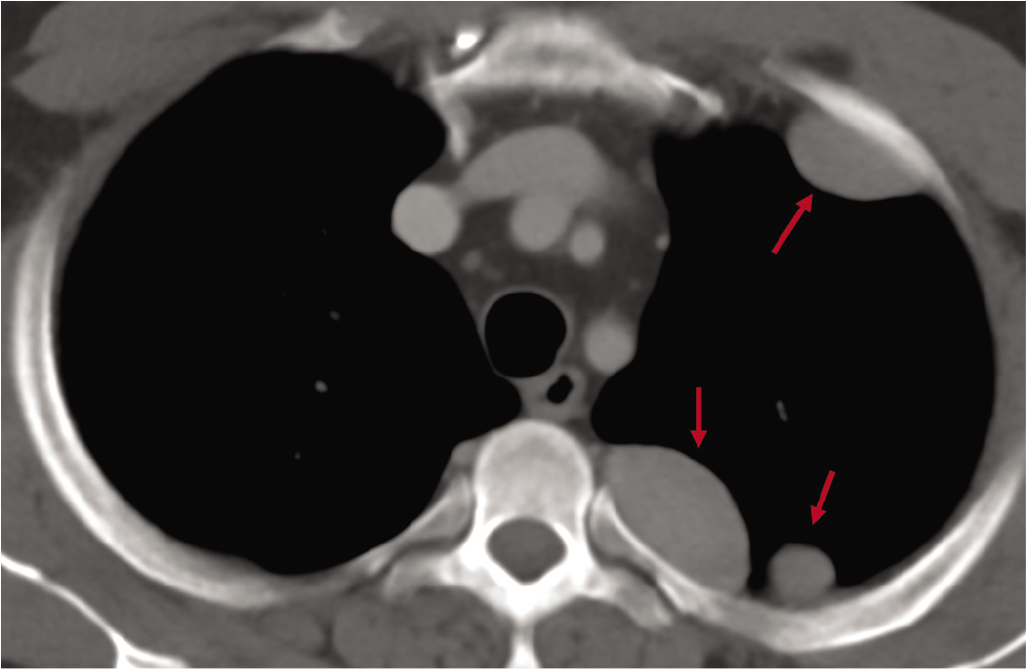
- Axial computed tomography scan of the chest showing multiple pleural/extrapleural nodules (arrows)
The patient, who incidentally had suffered a gunshot wound to the abdomen 20 years ago, resulting in a splenectomy, was discovered to have these chest lesions two years ago during a routine examination. The patient had been to Jordan and China for evaluation, and biopsies done in both countries were reported to be negative. He was worried about mesothelioma, a diagnosis mentioned in the only paper he carried with him, which was a summary of clinical findings from a doctor in Thailand, who had recommended a video-assisted thoracoscopic biopsy, which the patient had refused.
A CT-guided core biopsy was performed (Fig. 2). The lesion was soft, and a multiquadrant biopsy yielded blood and fibrinous material. Tumours such as mesothelioma, metastases and neurogenic tumours are invariably ‘hard or rough’ to feel. On reviewing the images, the sagittal reconstruction (Fig. 3) showed evidence of a healed diaphragmatic tear, which he had perhaps sustained at the time of the gunshot injury and the ruptured spleen, 20 years ago.
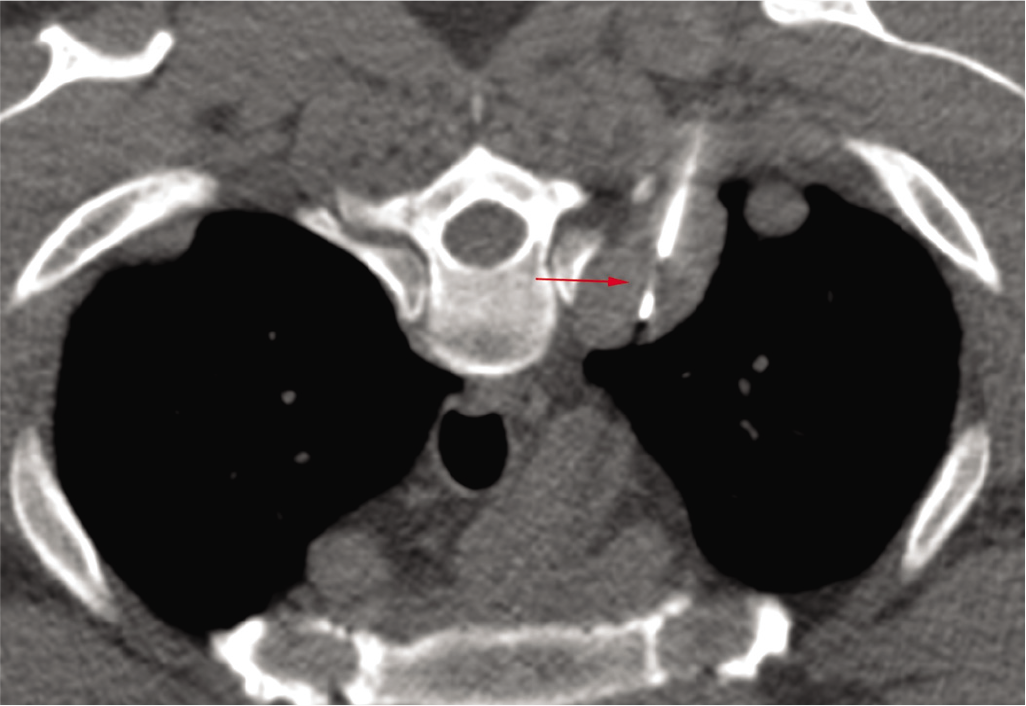
- Axial prone computed tomography-guided biopsy showing the 18G gun tip inside the posterior nodule (arrow)
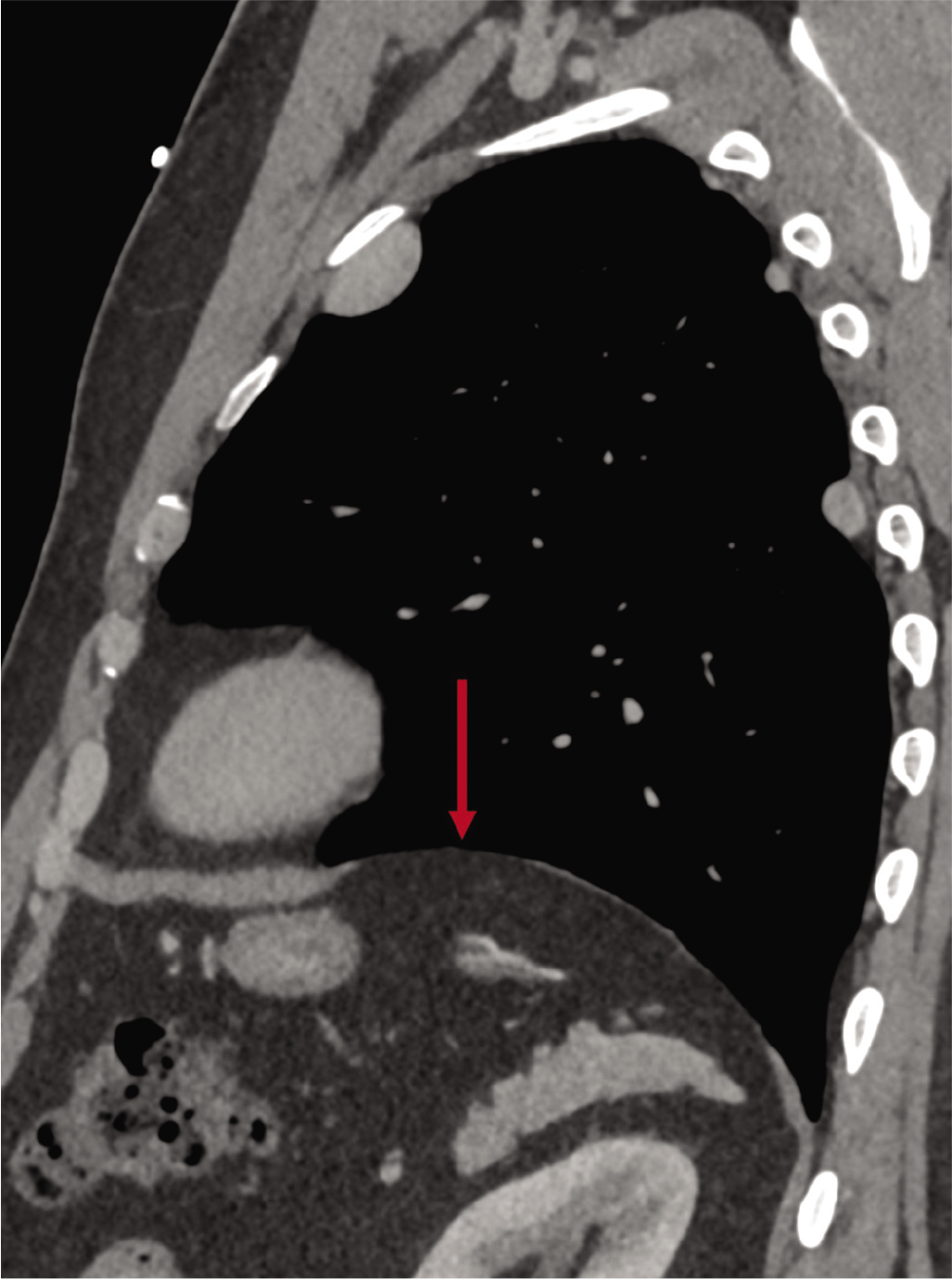
- Sagittal computed tomography scan of the left half of the chest showing the defect in the left hemi-diaphragm (arrow). Note no spleen is seen
A Tc-sulphur colloid scan was done, which showed findings consistent with splenosis (Fig. 4). The pathologist confirmed that the material biopsied was splenic tissue (Fig. 5).
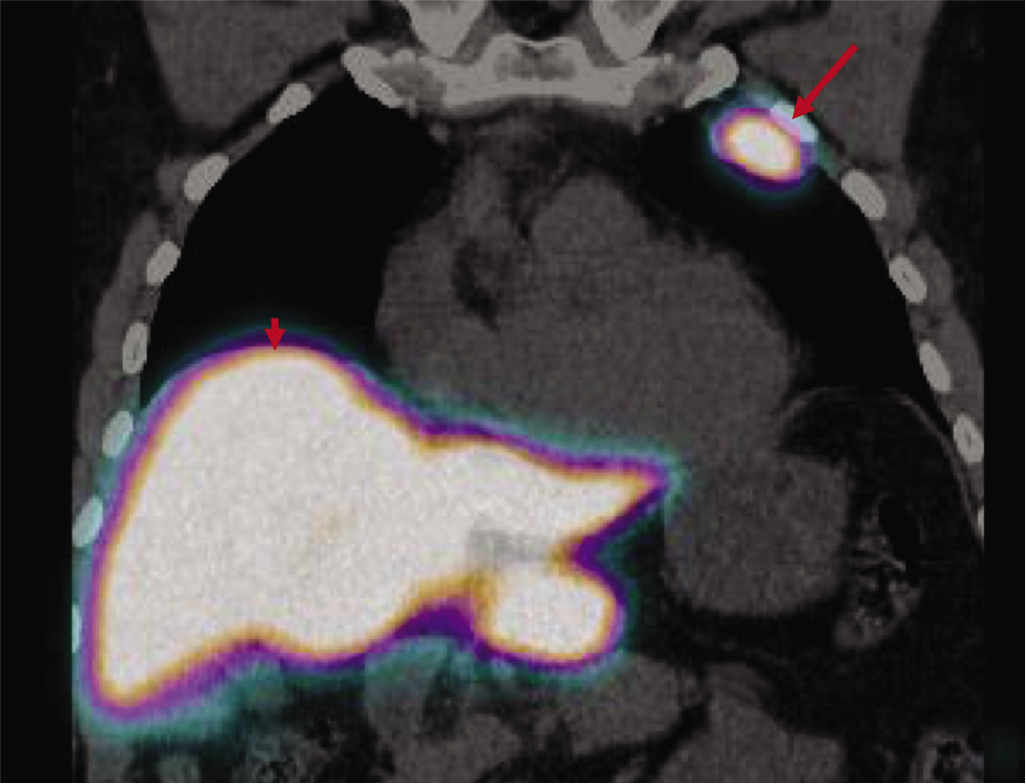
- Coronal Tc-sulphur colloid scan showing the pleural/ extrapleural nodule (arrow) with the same uptake as that of the liver (arrowhead)
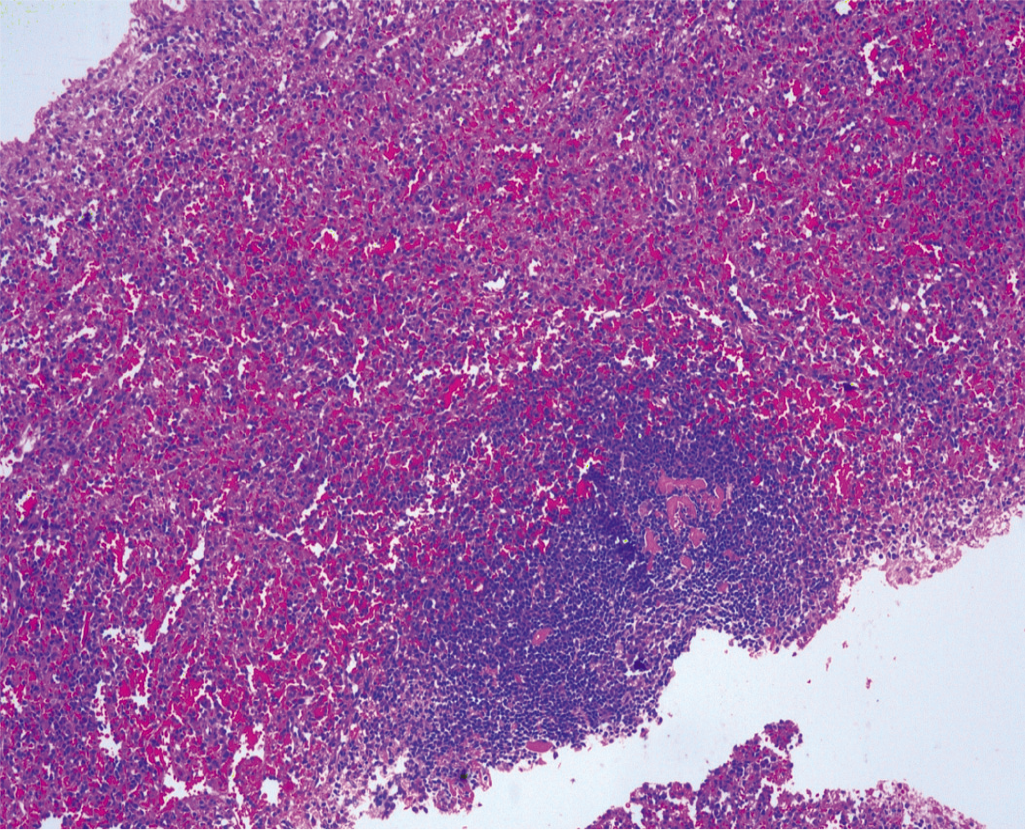
- Haematoxylin and eosin histopathology slide showing typical splenic tissue
DISCUSSION
There are anecdotal case reports and series describing thoracic splenosis.1–5 The concept is clear—if there is injury and splenic rupture along with a tear of the diaphragm, splenic tissue can migrate into the thorax and grow. Only one case of thoracic splenosis without a diaphragmatic rupture has been reported, suggesting haematogenous spread.6 Since thoracic splenosis is usually picked up a decade or two later, usually incidentally, when the patient comes for some other tests and the history of past trauma has often been forgotten or is not mentioned by the patient, the diagnosis can be a challenge. Some patients have even had thoracic surgery done to get to the diagnosis.5
It is possible that the diagnosis could have been achieved with a combination of the history, the Tc-sulphur colloid scan and the CT scan findings, but the biopsy report of splenic tissue within the thoracic masses confirmed the aetiology conclusively and allowed the patient to go back to his country, relieved.
With thoracic splenosis, unless the patient is symptomatic, no further intervention is required except for yearly or biannual follow-up with chest radiographs.
Conflicts of interest
None declared
References
- Thoracic splenosis mimicking a pleuropneumonia: A case report. Medicine (Baltimore). 2017;96:e7552.
- [CrossRef] [PubMed] [Google Scholar]
- A growth opportunity: Thoracic splenosis. Am J Med. 2017;130:420-2.
- [CrossRef] [PubMed] [Google Scholar]
- Scintigraphic diagnosis of intrathoracic splenic implants masquerading as malignancy. J Nucl Med Technol. 2016;44:267-8.
- [CrossRef] [PubMed] [Google Scholar]
- Thoracic splenosis: Correct imaging diagnosis prevents invasive procedures like biopsy and thoracoscopy. BMJ Case Rep. 2018;2018:bcr2018227355.
- [CrossRef] [PubMed] [Google Scholar]
- Thoracic splenosis presenting as pulmonary space-occupying lesion. BMC Surg. 2018;18:119.
- [CrossRef] [PubMed] [Google Scholar]
- Intrathoracic splenosis without clinical evidence of diaphragmatic rupture. Ann Thorac Surg. 2019;108:e221-2.
- [CrossRef] [PubMed] [Google Scholar]




