Translate this page into:
Truth telling and fully disclosing to cancer patients in India: A pragmatic approach
2 Department of Clinical Hematology, Tata Medical Center, New Town, Kolkata, West Bengal, India
3 Department of Digestive Diseases, Tata Medical Center, New Town, Kolkata, West Bengal, India
Corresponding Author:
Mohandas K Mallath
Department of Digestive Diseases, Tata Medical Center, New Town, Kolkata, West Bengal
India
mohandaskm@gmail.com
| How to cite this article: Nayar N, Nair R, Mallath MK. Truth telling and fully disclosing to cancer patients in India: A pragmatic approach. Natl Med J India 2020;33:375-378 |
Introduction
Incidence of cancer in India crossed a million new cases by 2018.[1] Modern multidisciplinary cancer care is a prolonged process involving expensive investigations and treatment. Many parts of India with large populations do not have well-staffed affordable treatment facilities for cancer near their homes.[1] Our public hospitals are overcrowded with new and relapsed cancer patients resulting in long waiting lists. Cancer care is the leading cause of out-of-pocket and catastrophic health expenditure in India.[2] Our population-based cancer survival is below the global average,[3] and cancer is feared by many Indians.
It is important to inform patients the whole truth about the status of their cancer including the stage, treatability and prognosis.[4] Several studies from the USA, Japan, China, etc., have revealed that full disclosure to patients with cancer is woefully inadequate.[5],[6],[7] Oncologists do disclose some information but not comprehensive enough or frequent enough to reinforce awareness of prognosis.[4] Unrealistic optimism when important treatment decisions are being made can result in net harm. It is the oncologist’s task to maintain an appropriate balance between optimism and realism while communicating with patients.[4]
Twenty-five years ago, one of us (MKM) had published a viewpoint on communicating bad news in India.[8] Since then, clinical oncology has seen a sea change. We found no high-quality primary research on truth telling to cancer patients from India. In view of our combined experience of 60 years in clinical oncology in public and not-for-profit cancer hospitals of India, we highlight the hurdles we have faced, and offer pragmatic steps to improve truth telling in India.
Hurdles to Truth Telling in India
Social, economic and linguistic hurdles
A systematic study of causes of deaths in 1.1 million homes had revealed that mortality related to cancer was most common in rural India and among the illiterate, the poor and the elderly.[9] Explaining to these patients the reality about cancer can be time consuming. A large proportion of Indian patients seek better treatment in far-off metropolitan cancer centres. The long waiting lists and delays make truth telling difficult for all stakeholders. Repeated hardships from travel, lodging, boarding and mounting expenses make patients and relatives desperate, vulnerable and too exhausted to ask questions when their turn comes up. Many patients are unable to comprehend what has been told to them more than once and keep asking: ‘Will I become all right?' The communication is further hampered by the linguistic diversity of India with interstate movement of patients.
Family is involved
The diagnosis of cancer has adverse effects on the whole family. In India, it takes a family to treat cancer, for the family members have multiple roles in providing physical, emotional and financial support.[10],[11] Some family members even take important decisions on behalf of patients. Family members often try to titrate the truth-telling process. Wide variations in India’s cultural, religious, linguistic and socioeconomic fabric combined with poor health literacy, superstitions and personal beliefs create hurdles to truth telling.
Requests from caregivers not to disclose the diagnosis of cancer and/or its prognosis directly to the patient are common. Obliging to such requests by keeping a mentally sound patient unaware of the true nature of their cancer and its treatment is unlawful except in case of an oncological emergency.[12] Yet as it often happens in India, even judges, lawyers, doctors, bureaucrats, politicians and union leaders do ask us not to disclose the diagnosis of cancer to their loved ones. Every patient being treated in a specialized cancer hospital comes to know the diagnosis sooner or later, but in multispecialty hospitals, the truth may be hidden for long.
Lack of privacy to grieve
All our public and not-for-profit cancer treatment facilities are overcrowded with long waiting lists. All oncologists are overburdened and hard-pressed for time. The art and skill set for communicating bad news was never taught to medical practitioners of India till recently. As a result, any provisional diagnosis of cancer is hardly communicated to a patient by their primary physicians. This role is passed on by referring the patient to a higher centre or to an oncologist. Compared to the West, most oncology consultations in India are of shorter duration. The clinics of our public hospitals also lack the privacy needed for communicating bad news. The truth telling process is carried out in overcrowded, impersonal settings in a hurried manner often by less experienced trainee oncologists.
Half-informed patients
Truth telling used to be a monologue on which oncologists had absolute control. Today, patients or their family members come for a dialogue with prior information often because of the internet. This is a good trend, but there is ‘one last question’ that never ends if you are empathetic. Information accessed from the internet is of uncertain quality and can be a double-edged sword.[13] For example, many with metastatic cancers come with inflated hope, expecting that the latest treatments (e.g. immunotherapy) will cure them. The younger family members who usually gather the internet information create another layer and increase the duration of truth telling. In the era of personalized oncology, several treatment options are possible for the same patient. Explaining the elements of precision oncology before expensive mutation testing or prescribing expensive palliative treatments requires intense dialogues and explanation. Financial toxicity from modern cancer treatment is a global issue and must be an inherent part of truth telling when patients are paying out of pocket.
Potential for violence
Miscommunication is one of the leading causes of increasing violence against doctors. Frivolous litigation in consumer or criminal courts is another kind of mental violence against doctors. Mistaken diagnosis, missed diagnosis, delayed diagnosis, delayed starting of treatments, discordance between imaging and surgical findings, rapid progression or deterioration after a biopsy, sudden changes in treatment plans after the detection of metastasis following exploratory surgery, short survival after expensive therapy, etc. are common reasons for loss of trust, expression of anger and litigation in clinical oncology. Little explanation can trigger misunderstanding. Involvement of caregivers simultaneously or separately during the truth telling process may be needed, for they often trigger aggression on the doctors. These local realities have to be accommodated.
To tell or not to tell
Oncology is one of the most demanding and stressful areas of medicine. Oncologists face life and death decisions on a daily basis, administer toxic treatments with narrow therapeutic index, must keep up with rapid introduction of new treatments and walk the tight rope when providing expensive toxic palliative treatments. Explaining treatment options after confirmation of cancer is an important part of truth telling. Should the oncologist disclose all the treatment options available, knowing that some of these are catastrophically expensive? Caregivers not told about the latest therapies may turn hostile when they find through a second opinion consult or from the internet that a new treatment may have helped their loved one. The frustration and anger of the family members sometimes result in complaints, litigation or physical violence.
Pragmatic solutions
It is universally agreed that all cancer patients are fully informed, for such a patient has the greatest ability and freedom to choose their treatment and reduce the dependence on others. Understanding that the cancer is terminal can empower a patient to take important decisions regarding palliative treatments, living will, funeral arrangements, etc. Indian laws are based on western thoughts and mandate that all patients should be told the whole truth. Studies show that truth telling is partial even in the developed countries.[5],[6],[7] Dr Hanny Ai-Samkari has published that his effort to mandate a competency in disclosure for haematology–oncology fellows was voted out as too many attending oncologists do not do this themselves.[4]
Truth telling in modern clinical oncology needs to be done many times during the cancer care continuum.[4] Starting before the diagnostic and staging procedures, truth telling is done before primary treatments (surgery, radiotherapy and chemotherapy), when cancer recurs, before second- or third-line therapies, when sudden unexpected complications arise after treatments, when all treatments have failed and the patient has to move on to palliative care, ending finally with the do-not-resuscitate (DNR) consent. Given these realities, the non-validated western methods of truth telling are not pragmatic in India.
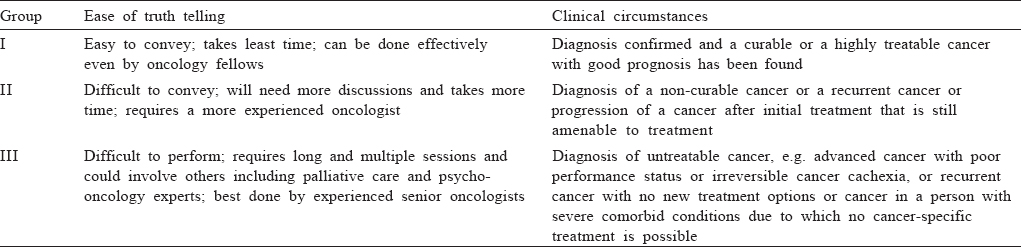
Conveying the diagnosis of cancer to an unknown new patient is difficult. The context, the time and expertise needed in truth telling vary widely in clinical practise. We suggest grading bad news in three groups [Table - 1]. Talking to patients in group I is straightforward for it ends by giving much hope for recovery. The effective interventions make it easy for the less experienced oncologist. Truth telling to the middle group is time-consuming and involves dialogues and clarifications. The prospects of some treatments prolonging life or improving the quality of life make the communication manageable with some experience. The third and the most difficult group continues to challenge even the experienced. Truth telling to patients in this group needs ample time, tact and hands-on experience. Answering repeated questions and handling the emotional outbursts (often by women family members) needs patience and tact. Initially, we provide some facts to the patient and direct them to palliative care services while the full truth is conveyed to patient’s caregivers. As the communication channels build up, more on prognosis and issues such as ‘DNR’ are discussed in subsequent visits. For some, there will not be a second visit. The hopeless situation is often met with unrealistic questions such as: ‘Please do something.' ‘Will I be all right doctor?' ‘Is there expertise in other hospitals in India or abroad?' Rarely, socioeconomically weak patients show up in private clinics, hoping that some treatment will be available on payment. Listening patiently and repeating the truth and offering them help with palliative care is the only way forward. We do feel unhappy after such sessions. In desperate situations, we may even suggest patients to try alternative therapies. We have found that the economic status of a patient is directly proportional to the duration of the truth telling process. Below poverty line patients or their caregivers quietly accept a junior oncologist’s brief communication rather quickly and humbly as the will of god. Long sessions are generally needed with young patients with unfinished parental responsibilities.
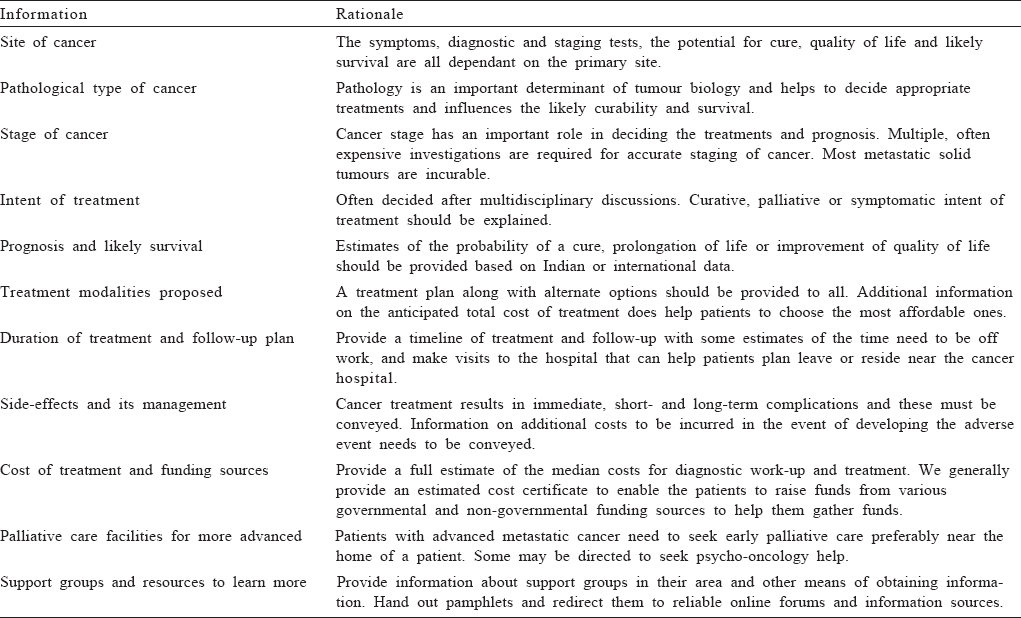
There are no validated methods for truth telling in India. Western protocols are untested and impractical. One popular approach uses the Setting, Perception, Invitation, Knowledge, Empathy and Summary (SPIKES) protocol.[14] It would be obvious to anyone who has worked in or visited the overcrowded clinics of our government-run public hospitals that ground realities do not match the SPIKES protocol. At present, there is no quick, simple and easy-to-use practical approach for truth telling to our patients. More effort is needed to overcome the lack of time needed for truth telling in Indian hospitals. An oncologist needs to discuss the treatment plan, possible complications and survival benefits and cost estimates for each of the treatment options including additional costs if complications arise. More explanations can be offered when the patient is admitted for treatment. Electronic medical records (EMRs) are increasing Indian oncology practices. The EMR enables speedy capture of relevant information, which can be handed over to the patient [Table - 2]. In the absence of EMR, a printed form which can be filled by hand can provide the essential information that can be given to all patients. Patients should also be advised to read information booklets about their cancers in regional languages, which are now available in India.
Many referring doctors in India are uncomfortable in having any discussion on the likely diagnosis of cancer and pass on the job to the next level. There is an urgent need for practical, hands-on training on truth telling during medical training to improve the skills of young doctors. The regulators, university board of studies, employers, patient advocacy groups and other stakeholders need to facilitate this. We hope that the new competency-based MBBS curriculum would help to close some of these gaps.[15]
Summary
Truth telling following the diagnosis of cancer is a complex, time-consuming exercise, intertwined with multiple discussions regarding re-testing and re-treating. Full disclosure is comparatively easy when cancer is diagnosed early in a treatable stage. Full disclosure is extremely difficult for many patients and their oncologists when there is no hope of further treatment other than palliative care. Achieving the ideal aim of providing full disclosure to all patients with cancer will continue to pose ethical, legal and societal challenges in India. Our experience shows that giving a neatly written or typed statement with all the useful information to all patients helps in eliminating major gaps. Such a document remains a ready reckoner with the patient even if he/she chooses to get another opinion and also helps to meet the ethical and legal requirements of our society.
Conflicts of interest. None declared
| 1. | Smith RD, Mallath MK. History of the growing burden of cancer in India: From antiquity to the 21st century. J Glob Oncol 2019;5:1–5. [Google Scholar] |
| 2. | Rajpal S, Kumar A, Joe W. Economic burden of cancer in India: Evidence from cross-sectional nationally representative household survey, 2014. PLoS One 2018;13:e0193320. [Google Scholar] |
| 3. | Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšiæ M, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018;391:1023–75. [Google Scholar] |
| 4. | Al-Samkari H. Striving for full disclosure—an intergenerational challenge. Cancer 2020; 126:1150–1. [Google Scholar] |
| 5. | Weeks JC, Catalano PJ, Cronin A, Finkelman MD, Mack JW, Keating NL, et al. Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med 2012; 367:1616–25. [Google Scholar] |
| 6. | Uchida M, Sugie C, Yoshimura M, Suzuki E, Shibamoto Y, Hiraoka M, et al. Factors associated with a preference for disclosure of life expectancy information from physicians: A cross-sectional survey of cancer patients undergoing radiation therapy. Support Care Cancer 2019;27:4487–95. [Google Scholar] |
| 7. | Wang H, Zhao F, Wang X, Chen X. To tell or not: The Chinese doctors’ dilemma on disclosure of a cancer diagnosis to the patient. Iran J Public Health 2018; 47:1773–4. [Google Scholar] |
| 8. | Mohandas KM. Ethical dilemmas in breaking bad news. Med Ethics 1995;3:59–60. [Google Scholar] |
| 9. | Dikshit R, Gupta PC, Ramasundarahettige C, Gajalakshmi V, Aleksandrowicz L, Badwe R, et al. Cancer mortality in India: A nationally representative survey. Lancet 2012;379:1807–16. [Google Scholar] |
| 10. | Burn G. From paper to practice: Quality of life in a developing country. The challenges that face us. Ann N Y Acad Sci 1997;809:249–60. [Google Scholar] |
| 11. | Rao A, Ekstrand M, Heylen E, Raju G, Shet A. Breaking bad news: Patient preferences and the role of family members when delivering a cancer diagnosis. Asian Pac J Cancer Prev 2016;17:1779–84. [Google Scholar] |
| 12. | Mathiharan K. Law on consent and confidentiality in India: A need for clarity. Natl Med J India 2014;27:39–42. [Google Scholar] |
| 13. | Chen X, Siu LL. Impact of the media and the internet on oncology: Survey of cancer patients and oncologists in Canada. J Clin Oncol 2001;19:4291–7. [Google Scholar] |
| 14. | Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES-A six-step protocol for delivering bad news: Application to the patient with cancer. Oncologist 2000;5:302–11. [Google Scholar] |
| 15. | Medical Council of India. Competency based undergraduate curriculum. Available at www.mciindia.org/CMS/information-desk/for-colleges/ug-curriculum (accessed on 1 Dec 2019). [Google Scholar] |
Fulltext Views
2,485
PDF downloads
1,163




