Translate this page into:
Ventricular bigeminy in enteric fever
Corresponding Author:
Priyanka Tolani
Department of Medicine, Northern Railway Central Hospital, New Delhi
India
priyankartolani@gmail.com
| How to cite this article: Kaushal M, Tolani P, Kumar N, Chopda A. Ventricular bigeminy in enteric fever. Natl Med J India 2019;32:216-217 |
Abstract
Salmonella infection causes a wide range of intestinal and extraintestinal manifestations as well as a lifetime carrier state. Untreated patients may develop complications, which can be life-threatening. Electrocardiogram (ECG) changes are a common occurrence in enteric fever and may be helpful in predicting myocarditis. Common ECG changes are decreased amplitude of QRS complexes, QTc prolongation and right bundle branch block. Ventricular bigeminy in enteric fever is a rare phenomenon. We report its occurrence in a patient.Introduction
Enteric fever is endemic in India. It is caused by Salmonella typhi and S. paratyphi. Usually, it is uncomplicated but complications, which can even be fatal, may occur in untreated patients. Hence, it is important to have a high index of suspicion for even rare manifestations of this common entity. We describe a patient infected with S. paratyphi A who developed ventricular bigeminy.
The Case
A 24-year-old man was admitted to our hospital with chief complaints of fever with chills for 5 days associated with severe occipital headache and restlessness. On examination, his pulse rate (PR) was 120/minute, regularly irregular, pulsus bigeminus, blood pressure was 120/80 mmHg and the temperature was 101.2 °F with no signs of meningeal irritation. The rest of the general physical and systemic examination were unremarkable.
Investigations revealed a haemoglobin of 12.4 g/dl, total leucocyte count 6200/cmm (neutrophils 72.2%, lymphocytes 16.4%, monocytes 10.9%, eosinophils 0.1% and basophils 0.4%) and platelet count 122 000/cmm. Immunochromatography and peripheral smear for malarial parasite were negative. The renal and liver function tests were: urea 15 mg/dl; creatinine 0.8 mg/dl; total bilirubin 0.8 mg/dl; aspartate aminotransferase 29 U/L; alanine aminotransferase 24 U/L; alkaline phosphatase 90 U/L; serum sodium 135 mmol/L and serum potassium 3.4 mmol/L. Urine routine and microscopic examination were normal as was the chest X-ray. Blood and urine cultures were sent.
Electrocardiogram (ECG) showed ventricular bigeminy at admission [Figure - 1]. Echocardiogram revealed normal left ventricular systolic function (ejection fraction 65%) with no abnormality of the valvular or regional wall motion. Pericardial reaction was present. In view of high-grade fever, low general condition, slight monocytosis, eosinopenia and thrombocytopenia and negative peripheral smear for malarial parasite, a possible diagnosis of enteric fever was made.
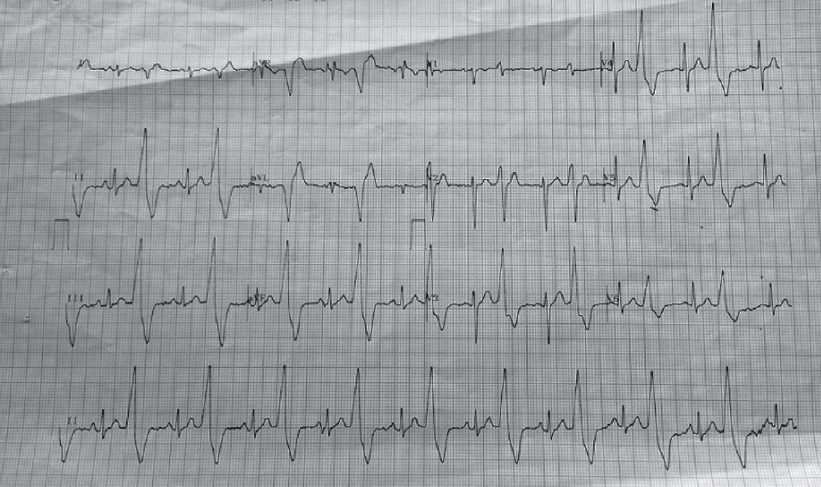 |
| Figure 1: Electrocardiogram on the first day of admission |
The patient was admitted to the intensive care unit and injection ceftriaxone was started. On the second day of antibiotic therapy, he started feeling better and his ECG reverted to normal sinus rhythm [Figure - 2]. On the third day, few ventricular ectopics were noted [Figure - 3] which settled by the fourth day [Figure - 4]. By the fourth day, he was afebrile. There was growth of S. enterica serotype paratyphi A in blood culture after 4 days which was susceptible to all the commonly used antibiotics (ampicillin, co-trimoxazole, chloramphenicol, tetracycline, ciprofloxacin, ofloxacin, ceftizoxime, cefotaxime, ceftriaxone, gentamicin, amikacin, colistin, piperacillin and meropenem).
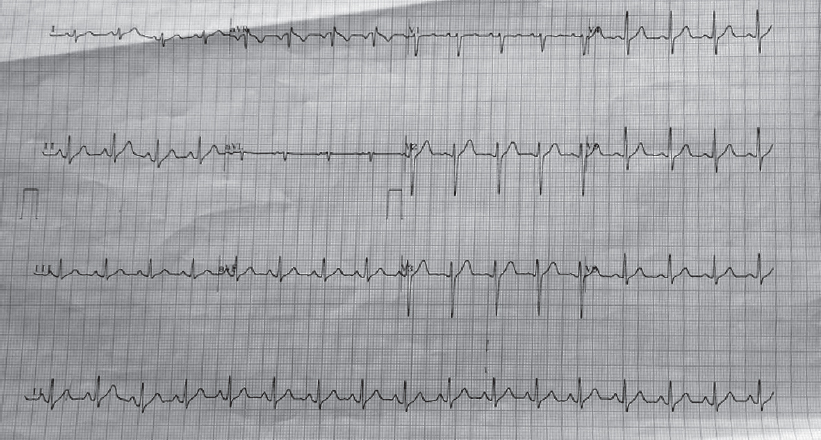 |
| Figure 2: Electrocardiogram on the second day of admission |
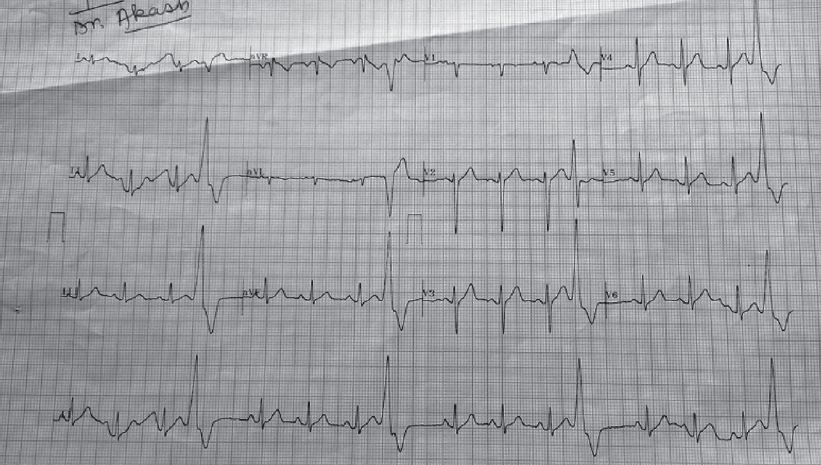 |
| Figure 3: Electrocardiogram on the third day of admission |
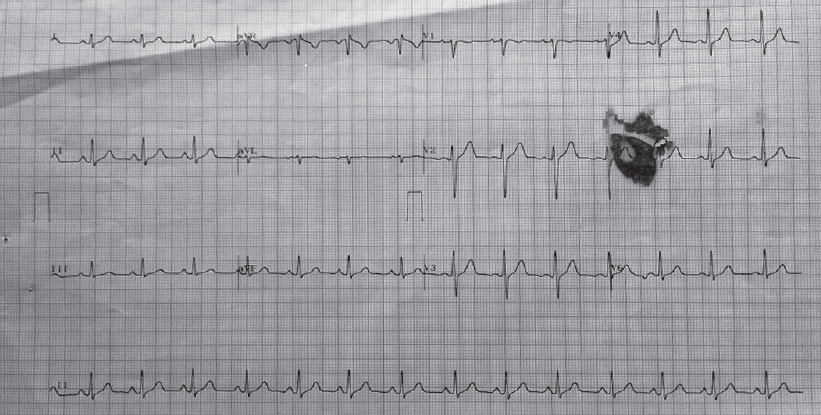 |
| Figure 4: Electrocardiogram on the fourth day of admission |
Injection ceftriaxone at a dose of 2 g i. v. 12 hourly was continued for 7 days. He was discharged in a stable condition on the seventh day after admission on oral cefixime 400 mg twice a day for 7 days and tablet azithromycin 500 mg twice a day for 5 days.
Discussion
Enteric fever includes typhoid and paratyphoid fever. In the pre-antibiotic era, it used to be a fatal disease with a mortality rate of 10%–20%. With antibiotic treatment, however, mortality has decreased to 1%.' Life-threatening complications typically occur during the third week of illness and are primarily gastrointestinal. The incidence of cardiac involvement is variable. In one series, cardiac complications were seen in only 4.6% of patients.[2] Among cardiovascular complications, the most common is salmonella myocarditis (1%–2%), others being endocarditis and pericarditis. A few cases of arterial and venous thrombosis post-enteric fever have also been reported in the literature.[3]
Isolated ECG abnormalities occur in 40%–80% of patients. ECG changes appear at the height of the pyrexial illness and are transient except bundle branch block, which may persist longer.
They occur commonly between the first and second week. Some common ECG abnormalities reported in enteric fever are decreased amplitude of QRS complexes (possibly due to myocarditis), prolongation of the QTc interval (related to loss of K+ from myocardial cells due to tissue anoxia), ST-T segment changes, prolongation of the PR interval, right bundle branch block and Wenckebach phenomenon.[3],[4] Ventricular ectopics have rarely been reported in patients with myocarditis.[5] However, ventricular bigeminy is a rare ECG manifestation of enteric fever.
ECG alterations bear a direct relationship to severity of the disease process, occur at the height of illness and have a bearing on the prognosis. Prognosis has been reported to be poor in patients where the ECG alterations persisted and such patients usually had a fatal outcome.[6]
Hence, it is important to get an ECG of all patients admitted with enteric fever, so that cardiovascular complications can be predicted. Early and prompt institution of treatment—with antibiotics or corticosteroids—will lead to better prognosis and early recovery of the patient.
We report this rare association of enteric fever with ventricular bigeminy. With prompt institution of antibiotic therapy, the patient’s symptoms improved and his rhythm reverted to normal sinus rhythm.
Conclusion
Cardiovascular complications and ECG abnormalities have been observed in enteric fever, but isolated ventricular bigeminy is rare. Hence, a 12-lead ECG should be done in all patients suspected to have enteric fever.
Conflict of interest. None declared
| 1. | Palombo M, Margalit-Yehuda R, Leshem E, Sidi Y, Schwartz E. Near-fatal myocarditis complicating typhoid fever in a traveler returning from Nepal. J Travel Med 2013;20:329-32. [Google Scholar] |
| 2. | Esmailpour N, Rasoolinejad M, Abdolbaghi MH. Cardiopulmonary manifestations of typhoid fever: A prospective analysis of 65 cases in Iran. Trop Doct 2006;36:118-19. [Google Scholar] |
| 3. | Singh S, Singhi S. Cardiovascular complications of enteric fever. Indian Pediatr 1992;29:1319-22. [Google Scholar] |
| 4. | Singh S, Gupta A, Marwaha RK. Wenckebach phenomenon and motor aphasia in enteric fever. Indian J Pediatr 1993;60:147-9. [Google Scholar] |
| 5. | Chowdhary S, Bhatnagar HN, Singh SV. Myocarditis in enteric fever. J Assoc Physicians India 1974;22:251-4. [Google Scholar] |
| 6. | Khosla SN. The heart in enteric (typhoid) fever. J Trop Med Hyg 1981;84:125-31. [Google Scholar] |
Fulltext Views
2,921
PDF downloads
2,049




