Translate this page into:
Incorporating ABC in physiology education: Active learning, blended learning and curricular changes
Correspondence to DEEPIKA VELUSAMI; deepy843@gmail.com
[To cite: Soundariya K, Velusami D. Incorporating ABC in physiology education: Active learning, blended learning and curricular changes. Natl Med J India 2023;36:182–6. DOI: 10.25259/NMJI_883_2021]
Abstract
Physiology is of central importance in medicine. Teaching the complex physiological frameworks to the current generation of students with the implementation of competency-based medical education (CBME) has become a challenging task. Development of digital technology in educational field during Covid-19 pandemic has made medical educators modify their teaching learning strategies from traditional to blended mode. We offer tips to embrace the three major challenges namely, generational diversity with active learning strategies, technological growth with blended learning, and strategies to implement curricular changes in physiology education. Adult learning principles involve active learning as a crux component. Various simple active teaching strategies that can be adapted for large and small group teaching are highlighted. Blended learning is characterized by self-paced learning, and face-to-face training sessions with online collaborative learning. Simple ways to incorporate the blended mode of teaching strategies with the use of virtual platforms and learning management system (LMS) are described. Further, we discuss the nuances that help to adapt the various curriculum changes brought about by the implementation of CBME. Teaching physiology is an ever-challenging task. With an appropriate mindset, medical educators can turn these challenges into opportunities and make teaching learning a better experience.
INTRODUCTION
Human physiology forms the bedrock of the medical curriculum in laying a strong foundation for the understanding of the pathophysiology, clinical features, and management of a disease. Physiology can be considered the integrator of medical sciences. Medical physiologists need to use a multifaceted approach to handle the challenges associated with teaching physiology to undergraduate medical students. These include (i) generational diversity of the learners; (ii) technological growth in education; and (iii) the curricular change with the implementation of competency-based medical education (CBME) in the Indian undergraduate medical curriculum.
Generational diversity plays a major role in bringing a dynamic change in medical education. Every generation of learners is unique in their respective characteristics. This is the greatest challenge to medical educators in tailoring their instructional deliveries in alignment with the expectations of the existing generation of learners.1 In the existing scenario, Generation Z forms a major student population in medical colleges. The millennial teachers being educated by the generation of baby boomers need to be amphipathic in adapting to the attributes of generation Z.
Medical teachers need to embrace themselves with strategies to effectively utilize technology in physiology education, to confront the technologically fluent generation of learners. The Covid-19 pandemic has unravelled many information and communication technology (ICT)-enabled tools and virtual platforms that could be used by the teachers for providing interactive learning sessions.2 Blended learning offers opportunities to blend traditional classroom teaching with online learning thereby enhancing the learning experience.
The National Medical Commission (NMC) of India introduced CBME for the undergraduate medical curriculum. This has added to the existing responsibilities of medical physiologists to adopt and adapt to the curriculum and implement necessary changes in curricular delivery.3
METHODS
Search strategy
This narrative review offers tips for medical physiologists to embrace the three major challenges such as generational diversity with active learning strategies, technological growth with blended learning, and strategies to implement curricular changes in physiology education.4 So, the articles cited are hand-picked, with effective utilization of cross references to offer a better insight to the readers. The articles were picked from PubMed, Google Scholar and Eric (for an effective coverage of practices in higher education), using the key words ‘Active Learning’, ‘Blended Learning’, ‘Medical Education’, ‘Generation Z’, ‘CBME’, ‘Medical Curriculum’, ‘E-Learning’ and ‘Digital Tools’. We have also added recommendations from the NMC. After removing duplicates, we came to a consensus of 38 articles.
A FOR Z (ACTIVE LEARNING STRATEGIES FOR GENERATION Z)
Generation Z learners are active learners, who are accustomed to getting information on demand. They require customization towards instructional delivery and prefer hands-on training. Choosing the appropriate active learning strategy for generation Z learners plays a major role in the attainment of learning outcomes.5 Bonwell and Eison defined active learning strategies as those ‘instructional activities involving students in doing things and thinking about what they are doing’.6 Educational theories play a major role in the delivery of curricula. In the present scenario, the relationship between a teacher and a learner has progressed from a pedagogical approach to a heutagogical approach, which is essentially learner-led. The principles of connectivism, designed by George Siemens aptly suit the instructional designs for the current generation of adult learners with extensive social media and internet usage. Embedding educational theory in instructional delivery influences learning outcomes.7
Active learning is aligned with adult learning principles. Active learning fits the need for self-directed adult learners, who like to take responsibility for their own learning and correlate the relevant content with their past experience. The selection of appropriate active learning strategies depends on the types of learners and the content to be delivered.
Active learning strategies that can be adopted for large group teaching (Fig. 1)
Instant methods that require less time and preparation
Clarification pause. In this technique, the teacher, at the end of every 10–15 minutes during instructional delivery, takes a strategic clarification pause. During this period, the students can pair with their neighbour, discuss, review notes, and get their doubts clarified. It is considered an effective, yet simple approach to enhance student engagement.8
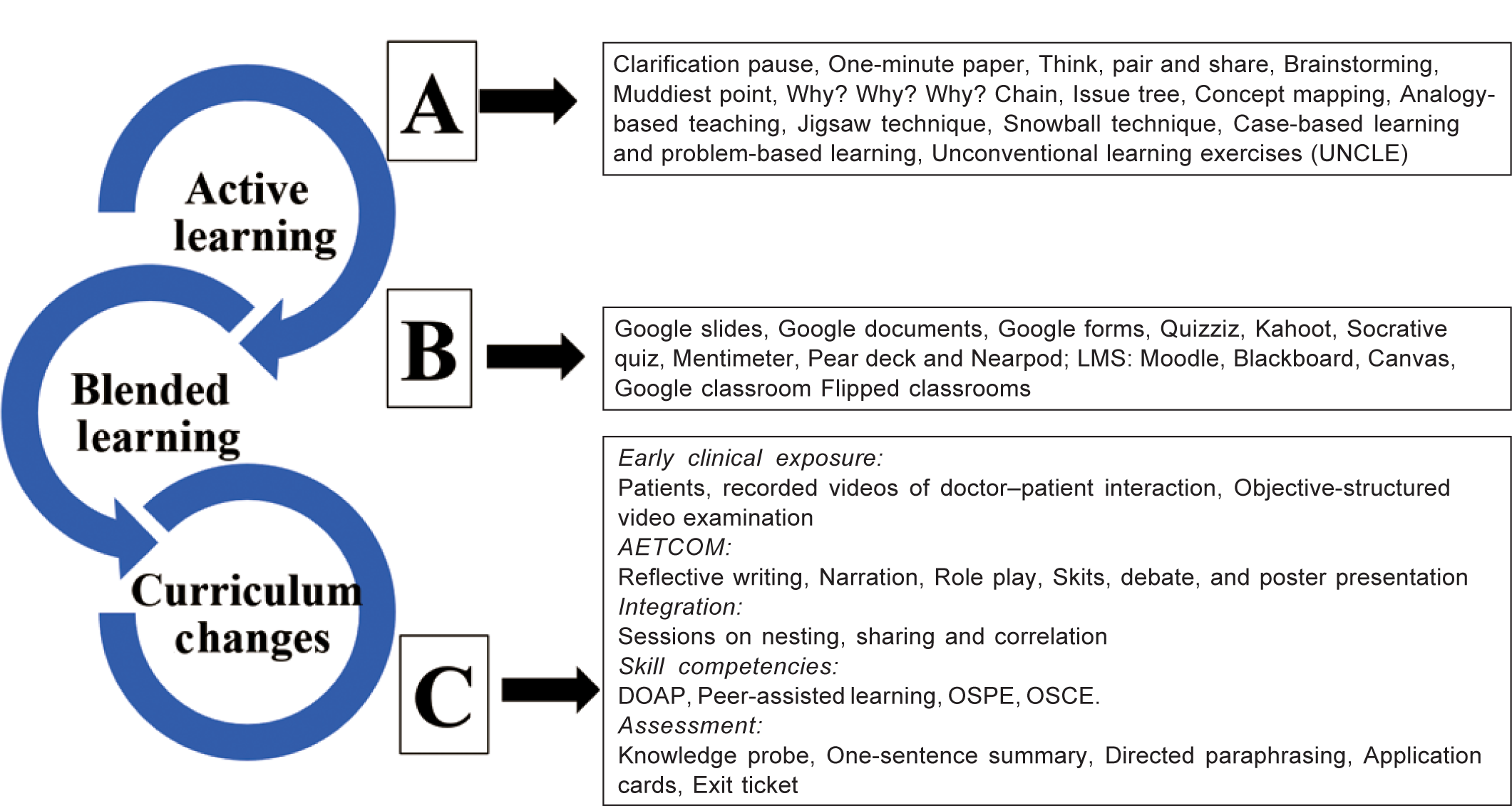
- Active learning strategies, blended learning and curriculum changes for improved teaching–learning in medical education DOAP demonstrate, observe, assist, perform OSPE objective-structured practical examination OSCE objective-structured clinical exmination
One-minute paper. This quick assessment technique reflects the achievement of learning objectives. Teachers may reserve one minute during or at the end of the session, where the learners are given an opportunity to reflect on two points like ‘What was the most important thing learned during the class?’ and ‘What was the most difficult concept to understand?’ This facilitates the achievement of learning outcomes.9
Think, pair and share. This helps students to individually form ideas and later pair with another learner and share their views, thereby enhancing collaborative learning.10
Brainstorming. In this technique, a list of ideas is gathered from a group of members to arrive at a conclusion. This technique is known to enhance ‘out of the box’ thinking by the learners.11
Muddiest point. This simplest technique provides information to the teachers on what the students perceive as the most confusing part of the delivered content.12
Methods with moderate time consumption
Why? Why? Why? Chain. This technique enhances the critical thinking of the learners by analysing the cause for an underlying issue, in stages by asking the question why. The role of the teacher is minimal.13
Issue tree. It is a way of structuring an enquiry to find out the causes, effects and solutions of a particular issue.13 This method helps the learners to have an in-depth understanding of the physiological concepts.
Concept mapping. This strategy helps learners to systematically categorize the physiological concepts and link the related facts visually by a graphical representation. The concept maps serve as effective learning resources with high learner engagement.14
Analogy-based teaching. The use of analogies in the learning process helps students to gain a better understanding of physiological concepts. The burden on the teacher in the preparation of resources may be reduced by encouraging students to frame and depict their own analogies.15
Active learning strategies that can be adapted for small group teaching
The following active learning strategies can be implemented in the classroom while addressing a small group of students.
Jigsaw technique. It is a collaborative technique where the students are divided into parent groups for discussion of a particular physiological concept. Each student in a parent group is allotted a sub-topic of the chosen concept. The members in each parent group on a particular sub-topic join together to form the expert group and discuss the sub-topic. Later, they return to the main parent groups for presentation. This method breaks the monotony, enhances communication skills and learner engagement.16
Snowball technique. It is a modification of buzz groups, where groups of two students join for a discussion. Then they pair up into groups of four and eight sequentially such as a pyramid and then ending with a presentation. It is considered to be effective in collaborative learning.17,18
Case-based and problem-based learning. Both these methods share the use of a clinical vignette in common. However, case-based learning is considered a guided inquiry with predefined objectives and the active role of the facilitator. In problem-based learning, the learning objectives are identified during the session, and the role of the facilitator is minimal. Both the methods are known to enhance clinical knowledge, attitude and teamwork.19
Unconventional learning exercises (UNCLE). These are active learning strategies that enhance student participation through the use of worksheets, group discussions, quizzes, debates and exercises that enhance critical thinking. It has been shown to enhance the presentation skills of students.20
In addition to the application of active learning strategies, the attainment of learning outcomes with the use of these techniques can be assessed by organizing events for students that test the higher levels of Bloom’s taxonomy such as preparation of concept posters, short videos and preparation of models depicting physiological concepts.
B FOR Z (BLENDED LEARNING FOR GENERATION Z)
Addressal of the technologically fluent generation of learners has demanded the incorporation of blended learning in medical education. The Covid-19 pandemic has reinforced the implementation of blended learning, in which students learn through online learning and also from the traditional brick-and-mortar location. Blended learning is characterized by self-paced learning and face-to-face training sessions with online collaborative learning.21–24 Blended learning fulfils the requirements of self-paced learning through online mode and the provision of personal contact with peers and teachers is offered through face-to-face learning (Fig. 1).
Simple ways to incorporate blended learning
In addition to the regular classroom activities, resources may be shared through email, WhatsApp, and virtual classrooms such as Google classroom. Assignments and announcements may also be made through these platforms.
This step can be made a little more interactive by creating threads in Google groups and motivating the students to participate in the chat and discussion forum.
Tools that can be used for blended learning
Google slides, Google documents, Google forms are widely used for sharing resources and posting assessments. They also facilitate collaborative learning.25
Platforms that can be exclusively used for assessment
Quizziz, Kahoot, Socrative Quiz, and Mentimeter are some virtual tools that can be effectively utilized for organizing quizzes for both small group and large group teaching, thus facilitating blended collaborative learning.26
Virtual classrooms
Pear Deck and Nearpod are some platforms that offer provisions for the synchronous and asynchronous mode of interactive learning.
Resources and formative assessments can be effectively planned and posted through these virtual platforms and have been shown to increase student engagement.
Learning management system (LMS)
Moodle, Blackboard, Canvas, Google classroom are some examples of LMS that may be effectively utilized for all processes in learning, starting from student enrolment for the courses to the assessment and awarding of credits to the students.27
All these virtual tools provide a supportive learning environment and enhance student engagement, provided they are appropriately and optimally used along with face-to-face sessions in the curriculum.
Flipped classroom
The flipped classroom can be a perfect example for blended learning. It is called flipped because it is considered an inversion of the traditional classroom. In a flipped classroom, objectives and handouts are shared well in advance of the class, the students perform a considerable amount of preparation well ahead of the class. In the actual class hours, problem-solving, discussion with peers, tutors and real-time collaboration and interaction take place. Studies have shown flipped classroom as an effective learning strategy that considerably enhances student engagement.28,29
C FOR Z (CURRICULAR CHANGES FOR GENERATION Z)
The outcome-based CBME has been implemented for the undergraduate medical curriculum in India. The essential components of the CBME include early clinical exposure, AETCOM (Attitude, Ethics, and Communication Skills), integrated teaching, certifiable skill modules with emphasis on self-directed learning, and formative assessments (Fig. 1).
To a physiologist, the implementation of CBME is associated with both challenges and opportunities. We highlight some strategies that help in converting the challenges to opportunities.
Early clinical exposure
The NMC has allotted 90 hours for early clinical exposure in the academic year for the first professional year, which are equally shared by Anatomy, Physiology and Biochemistry. In the 30 hours allotted for Physiology, 18 hours is allotted for basic science correlation and 12 hours for clinical skill demonstration.
Challenges. Shortage of faculty, non-availability of planned cases in the stipulated time and non-availability of clinical faculty are some of the challenges faced with the implementation of early clinical exposure.
Converting challenges into opportunities. The utilization of process experts may help in handling the issues of shortage of faculty.30 In case of non-availability of patients, recorded videos of doctor–patient interaction of interesting cases with patient consent, may be shared with the students for their reflection. This method of ‘objective-structured video examination’ as recommended by the NMC were of great help in conducting online clinical postings during the pandemic period.31 The clinical discussion may be conducted by medical physiologists and there are no guidelines that the content has to be delivered exclusively by the clinical faculty.
AETCOM
AETCOM is another important component of CBME and it is to be implemented longitudinally throughout the medical curriculum. The so-called ‘hidden curriculum’ has now been made explicit with the introduction of the AETCOM module across all the professional years. The AETCOM module can be organized by using many innovative teaching–learning strategies such as reflective writing, narration, role play, skits, debate, and poster presentation.4 The NMC has recommended including a short answer question in AETCOM module in the summative assessment.
Integration
Integration of the subject objectives across various domains/disciplines is a basic prerequisite for the successful attainment of competencies. Temporal coordination, sharing, nesting and correlation are some of the techniques of integration recommended by the NMC for the undergraduate medical curriculum.32
Waghmare et al. have suggested templates that can be used for implementing sessions on nesting, sharing and correlation.33 The following simple tips may help in planning a well-integrated session.
Review of the competencies from the different subjects in the respective topics chosen for integration
Removal of redundant competencies and objectives
Finalize the objectives to be planned for the session
Creation of linkers in liaison with the integrating department
Framing the lesson plan with appropriate teaching–learning method and assessment
Sharing and review of the content planned for delivery
Appropriate hours can be allotted for self-directed learning
Feedback should be obtained from the students and the faculty
The CBME curriculum offers ample opportunities to provide a holistic view of the physiological concepts through integration. Motivating faculty, good coordination between the departments, framing of a good lesson plan, choice of appropriate instructional delivery and assessment play a major role in the successful implementation of integrated teaching.
Certifiable skill competencies
Certification of certain skill competencies is another essential component of CBME.34 DOAP (Demonstrate, Observe, Assist, Perform) sessions are the suggested instructional strategy for the skill modules. It can be carried out in the following stages.
Instructor does and describes
Instructor does, the student describes
The student describes and does, under supervision, receives feedback
The student practices on her own
The student does
‘Peer-assisted learning’ is another active learning strategy that can be adopted during revision, where students acquire knowledge and skills through learning with peers in groups. In this technique, the peers take an active role as presenters, moderators and facilitators. The students are more likely to retain the steps in skill demonstration when they teach others.35
ASSESSMENT IN CBME
Formative assessment incorporated with feedback is a crucial component of the CBME curriculum.
Classroom assessment techniques
Some of the simple formative assessment techniques that can be incorporated in the classroom are as follows:36,37
Knowledge probe: At the beginning of the class, few questions may be posted to the students as MCQs or clinical scenarios to assess their prior knowledge on the content to be delivered. Clickers may be used in the class to provide a rough idea of the existing prior knowledge of the students.
One-sentence summary: The students may be asked to write the important concept that has been learnt from that particular session, in one sentence. With the implementation of blended learning, virtual classrooms may be effectively utilized by the students to post the content and the teachers to assess the same.
Directed paraphrasing: The students are instructed to write a crude summary of what they have learnt in the class and may be randomly asked to present it to their peers and the identified gaps clarified.
Application cards: The students may be asked to write down a real-world application for a concept that has been thought.
Exit ticket: At the end of the class, students are asked to write a response to a single question, posed on the content delivered in that class.
Skill assessment techniques
OSCE/OSPE: Objective-structured clinical examination (OSCE) and objective-structured practical examination (OSPE) are good examples for assessment of practical and clinical skills with the provision of immediate feedback.
SELF-DIRECTED LEARNING
The NMC has recommended the allotment of 25 hours in the physiology curriculum for self-directed learning. In self-directed learning, the students are encouraged to establish learning objectives, locate and access resources, adopt and execute their own learning activities, evaluate their own performance and with review can reassess their own learning strategies.38 It is better to allocate topics for self-directed learning, during the planning of the academic calendar. Further, the concept of self-directed learning should be adopted in various components of CBME such as early clinical exposure, AETCOM and integration. Self-directed learning plays a major role in linking active and blended learning, as many virtual tools may be effectively used for providing active learning strategies for asynchronous learning by the students.
CONCLUSION
Teaching medical physiology is associated with challenges. It is the purview of the faculty with support from the institution to convert all the challenges into opportunities. Implementation of the CBME curriculum is not free of challenges, but at the same time, it has opened the doors for active learning and blended learning in physiology education. It is time that physiologists act as facilitators in incorporating active learning strategies through a blended mode to facilitate the implementation of curricular changes in physiology education for generation Z learners.
Conflicts of interest
None declared
References
- Several Ways Generation Z May Shape the Medical School Landscape. J Med Educ Curric Dev. 2019;6:2382120519884325.
- [CrossRef] [PubMed] [Google Scholar]
- How COVID-19 kick-started online learning in medical education-The DigiMed study. PLoS One. 2021;16:e0257394.
- [CrossRef] [PubMed] [Google Scholar]
- Blended learning: Ten tips on how to implement it into a curriculum in healthcare education. GMS J Med Educ. 2020;37:Doc45.
- [Google Scholar]
- Competency-based physiology UG curriculum: Use of novel learning tools. Indian J Physiol Pharmacol. 2020;64(Suppl1):S19-S20.
- [CrossRef] [Google Scholar]
- Is medical education ready for generation Z? J Grad Med Educ. 2018;10:378-81.
- [CrossRef] [PubMed] [Google Scholar]
- Active learning: Creating excitement in the classroom 1991 ASHE-ERIC Higher Education Reports. ERIC Clearinghouse on Higher Education, The George Washington University, One Dupont Circle, Suite 630, Washington, DC 1991:20036-1183.
- [Google Scholar]
- Educational theory and its application to advanced life support courses: A narrative review. Resusc Plus. 2020;5:100053.
- [CrossRef] [PubMed] [Google Scholar]
- Effective use of pause procedure to enhance student engagement and learning. J Clin Diagn Res. 2014;8:XM01-XM03.
- [Google Scholar]
- One-minute paper: A thinking centered assessment tool. Internet J Med Update. 2013;8:1-9.
- [Google Scholar]
- Perceived effectiveness and applicability of think-pair-share including storytelling (TPS-S) to enhance clinical learning. Teach Learn Med. 2021;33:184-95.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of brainstorming session as a teaching-learning tool among postgraduate medical biochemistry students. Int J Appl Basic Med Res. 2017;7(Suppl 1):S15-S18.
- [CrossRef] [Google Scholar]
- Active learning strategies: Student perceptions. Acad Exchange Q. 2014;18:1096-453.
- [Google Scholar]
- Applying visual mapping techniques to promote learning in community-based medical education activities. BMC Med Educ. 2021;21:210.
- [CrossRef] [PubMed] [Google Scholar]
- Use of essential analogies in clinical anatomy active learning curriculum: A personal reflection. Transl Res Anatomy. 2020;18:100062.
- [CrossRef] [Google Scholar]
- Using the jigsaw technique to teach patient safety. Med Educ Online. 2020;25:1710325.
- [CrossRef] [PubMed] [Google Scholar]
- Small group discussion technique in pharmacology: An insight from a medical school in Mauritius. Quest Int J Med Health Sci. 2018;1:5-7.
- [CrossRef] [Google Scholar]
- Differentiating case-based learning from problem-based learning after a two-day introductory workshop on case-based learning. Australasian Med J. 2017;10:973-80.
- [CrossRef] [Google Scholar]
- An integrated problem-based curriculum for biochemistry teaching in medical sciences. Indian J Clin Biochem. 2002;17:52-9.
- [CrossRef] [PubMed] [Google Scholar]
- Blended learning: Ten tips on how to implement it into a curriculum in healthcare education. GMS J Med Educ. 2020;37:Doc45.
- [Google Scholar]
- A blended approach to active learning in a physiology laboratory-based subject facilitated by an e-learning component. Adv Physiol Educ. 2008;32:65-75.
- [CrossRef] [PubMed] [Google Scholar]
- Students' perception of animal or virtual laboratory in physiology practical classes in PBL medical hybrid curriculum. Adv Physiol Educ. 2019;43:451-7.
- [CrossRef] [PubMed] [Google Scholar]
- Student perceptions and learning outcomes of blended learning in a massive first-year core physiology for allied health subjects. Adv Physiol Educ. 2017;41:44-55.
- [CrossRef] [PubMed] [Google Scholar]
- Google Docs in an out-of-class collaborative writing activity. Int J Teach Learn Higher Educ. 2012;24:359-75.
- [Google Scholar]
- Using Kahoot! as a formative assessment tool in medical education: A phenomenological study. BMC Med Educ. 2019;19:230.
- [CrossRef] [PubMed] [Google Scholar]
- Learning management system and e-learning tools: An experience of medical students' usage and expectations. Int J Med Educ. 2016;7:267-73.
- [CrossRef] [PubMed] [Google Scholar]
- The flipped classroom: For active, effective and increased learning--especially for low achievers. Int J Educ Technol High Educ. 2016;13:33.
- [CrossRef] [Google Scholar]
- Flipped classroom or an active lecture? Clin Anat. 2018;31:118-21.
- [CrossRef] [PubMed] [Google Scholar]
- Tutors' roles and responsibilities in (PBL): Pros and cons of subject expert and tutorial process expert literature overview. Int Educ Res J. 2017;3:42-4.
- [Google Scholar]
- Module 8: Online learning and assessment 2020. p. :1-57. Available at www.nmc.org.in/wpcontent/uploads/2020/11/Module-8-Online-learning-and-assessment-17-11-20-version-final-foruploading-converted.pdf (accessed on 16 Oct 2021)
- [Google Scholar]
- Alignment and integration module for undergraduate medical education program. 2019:1-34. Available at www.nmc.org.in/wpcontent/uploads/2020/08/Alignment-and-Integration_03.10.2019.pdf (accessed on 16 Oct 2021)
- [Google Scholar]
- Revisiting integration: A proposed framework in the light of competency-based medical education in Indian context. J Clin Diagn Res. 2020;14:1-4.
- [CrossRef] [Google Scholar]
- A novel approach to medical student peer-assisted learning through case-based simulations. West J Emerg Med. 2018;19:193-7.
- [CrossRef] [PubMed] [Google Scholar]
- Attributes of classroom formative assessment techniques in medical education: A review. Vidarbha J Int Med. 2018;25:75-80.
- [Google Scholar]
- Classroom assessment techniques: An assessment and student evaluation method. Creative Educ. 2012;3:903-7.
- [CrossRef] [Google Scholar]
- Module to facilitate self-directed learning among medical undergraduates: Development and implementation. J Edu Health Promot. 2020;9:231.
- [CrossRef] [PubMed] [Google Scholar]




