Translate this page into:
Non-traditional tools for predicting coronary artery disease
Correspondence to RISHABH KHURANA; rishabhkhurana88@gmail.com
[To cite: Khurana R, Yadav A, Buxi TB, Rawat KS, Ghuman SS. Non-traditional tools for coronary artery disease prediction. Natl Med J India 2022;35:261–5.]
Abstract
Background
The traditional coronary calcium score (CCS) is a time-tested tool for the evaluation of coronary atherosclerosis and predictor of future cardiovascular events. Non-traditional tools can also have a value in predicting and detecting subclinical coronary artery disease (CAD).
Methods
We studied the role of CCS, the traditional CAD risk predictor, and the less-recognized, non-traditional risk factors, i.e. epicardial fat volume (EFV) and thoracic extracoronary calcium (ECC), to assess the degree of subclinical CAD. In this cross-sectional observational study, we included 950 Indian patients (suspected to have CAD). Coronary computed tomography angiography was performed. Estimation of CCS, EFV and thoracic ECC was done.
Results
A CCS of 0 was seen in 583 patients (61.4%). Of these, 492 patients had normal coronary angiogram but 91 patients had CAD. The median values of EFV were statistically significantly higher in the ‘CAD present and CCS 0’ group compared to the ‘CAD absent and CCS 0’ group (p<0.001). The presence of thoracic ECC involving at least a single site was seen in only 6 of these 91 patients. When both EFV and CCS were considered together for the detection of CAD, the sensitivity and negative predictive value (NPV) were improved compared to either of these in isolation. When ECC was taken together with CCS and EFV, no further improvement in sensitivity or NPV was observed.
Conclusion
The combined use of traditional CCS along with non-traditional EFV may guide us in better profiling cardiovascular risk and supplement the various traditional cardiovascular risk factors/scores.
INTRODUCTION
Cardiovascular diseases (CVDs) and stroke are the leading causes of mortality in India, with ischaemic heart disease as the major attributing factor. The Global Burden of Disease study has estimated the CVD death rate in India to be 272/100 000 population, as against the global average of 235/100 000. The situation is even more alarming in India as the onset of disease is at an earlier age with increased morbidity and mortality.1
The prevalence of ‘first-time’ coronary artery disease (CAD) is at nearly twice that of the prevalence of ‘recurrent’ CAD. This is inspite of vigorous preventive efforts in place for earlier risk recognition, assessment and characterization, with early risk management and interventions.2 Coronary calcium score (CCS) is an established surrogate marker of coronary atherosclerosis with significant association with medium- to long-term occurrence of major adverse cardiovascular events. It has evolved from the days of electron beam computed tomography (CT) to more precise measurements on dual-energy CT, but the Agatston and volume scores and estimation of plaque burden have remained largely unchanged. However, the major drawback is that only the stable calcified plaques are estimated and a relative risk of the disease is extrapolated. The vulnerable plaques, on the other hand, are predominantly fatty and escape detection on CCS.
Localized thoracic fat depots, especially the estimation of epicardial fat volume (EFV), is gaining importance as a new and independent risk predictor of CAD. Moreover, detection of calcification in various thoracic extracoronary (ECC) sites such as the aortic valve, mitral valve3 or thoracic aorta4 is a useful adjunct in predicting cardiovascular atherosclerosis, as the disease has a more all-encompassing presence.
Previously, we had observed that higher EFV was seen in patients having CAD compared to patients without CAD. Using an EFV cut-off value (49.75 ml) for CAD prediction, the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were 81%, 45.9%, 58.2% and 72.2%, respectively, with an overall diagnostic accuracy of 62.84%. Moreover, higher EFV was seen in patients with greater degrees of coronary arterial stenosis. On multivariate analysis, EFV was found to be an independent predictor for the presence of CAD.5 However, at present, EFV and thoracic ECC are not being used consistently for risk profiling of individuals.
We assessed the role of traditional CCS, and the less-recognized, but more promising, non-traditional factors, i.e. EFV and thoracic ECC, alone and in combination with each other to improve the detection of subclinical CAD with higher sensitivity and specificity. These were compared with the degree of coronary artery stenosis on coronary CT angiography performed concurrently for substantiating their roles.
METHODS
This cross-sectional, observational study comprised 950 Indian patients suspected to have CAD (symptomatic patients with intermediate pre-test probability of CAD or uninterpretable electrocardiogram or unable to exercise on stress tests). Coronary CT angiography was done for these patients during 2013–2016. Details of the analysed group and scan acquisition are referenced elsewhere.5 The study was approved by the ethical committee of the hospital and followed the guidelines mentioned in the Declaration of Helsinki.
Coronary artery calcium scoring was done as Agatston scores. Each calcified segment of coronary arteries was scored using software (semi-automatic) available at our institution. Predefined prediction of calcification was presence of minimal of three contiguous pixels with an attenuation of ≥130 Hounsfield Units.
Non-contrast scans were also analysed for the presence of calcification at four extracoronary sites, namely (i) aortic valve calcification (AVC); (ii) mitral valve calcification; (iii) thoracic aorta calcification (TAC); and (iv) aortic root calcification (ARC). Any calcified focus observed extending from the aortic valve to the aortic root was called AVC. TAC included visualized portions of the ascending and descending thoracic aorta. ARC was assessed and measured at the level of the aortic ring. Simple ordinal scoring from 0 to 4 was done for the above-mentioned sites.
The quantification of EFV was done using the abovementioned semi-automatic technique.5 Finally, coronary arteries were assessed for the presence of CAD and its degree of severity. The severity of CAD was classified as mild (<50% stenosis, non-obstructive), moderate (50%–75% stenosis) and severe (>75% stenosis). Greater than 50% stenosis was considered obstructive/significant CAD. In patients with varying degrees of stenosis in different coronary artery segments, the highest degree of stenosis was considered for classification of the severity of CAD.
Statistical analysis
The following methods were adopted: (i) statistical testing was done using the Statistical Package for Social Sciences (SPSS) software, version 17.0; (ii) continuous variables are presented as mean (standard deviation; SD) or median (interquartile range [IQR]); (iii) categorical variables are expressed as frequencies and percentages. Kruskal–Wallis test/Mann–Whitney U-test were used to compare medians as the data were non-normally distributed; (iv) a receiver operating characteristic (ROC) analysis was done; (v) the area under the curve (AUC), sensitivity, specificity, PPV, NPV and diagnostic accuracy were estimated. A value of p<0.05 was taken to indicate a significant difference.
RESULTS
A total of 950 patients were enrolled in the study. The mean (SD) age was 51 (11.2) years. The men-to-women ratio was 1.9:1 with 623 men (65.6%). Figure 1 shows the prevalence of traditional risk factors.
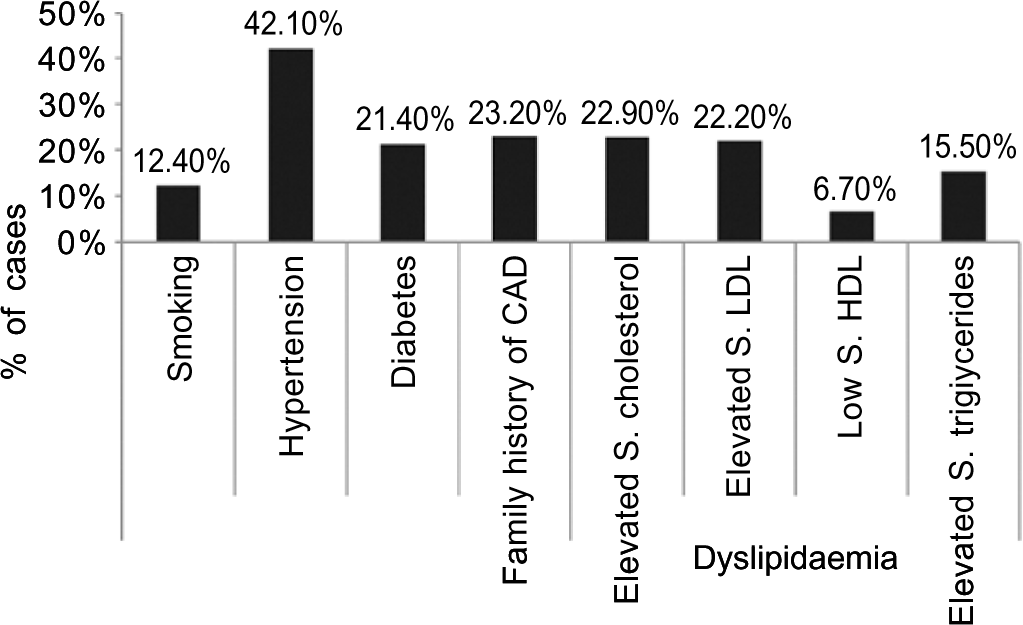
- Bar diagram showing distribution of various traditional risk factors in the study population CAD coronary artery disease S.HDL serum high-density lipoprotein S.LDL serum low-density lipoprotein
CCS was done in all the patients. The mean (SD) CCS in all patients was 98.5 (290.18). The patients were categorized on the basis of Agatston scores (Table I). A majority of patients (n=583, 61.4%) had a calcium score of 0. The majority of patients with a calcium score of 0 had a normal CT coronary angiogram (n=492). However, there was a subset of patients with a CCS 0 but having CAD (n=91). Hence, using CCS as the sole tool for CAD prediction, the sensitivity, specificity, PPV and NPV were 80.1% 100%, 100% and 84.4%, respectively, with a diagnostic accuracy of 90.2%. Higher CCS was observed in CAD groups with increasing severity of stenosis (Table II).
| CCS severity (%) | n (%) |
|---|---|
| Normal: 0 | 583 (61.4) |
| Minimal: 1–9 | 4 9 (5.1) |
| Mild: 10–99 | 133 (14) |
| Moderate: 100–399 | 118 (12.4) |
| Severe: >400 | 6 7 (7.1) |
| Total | 950 (100) |
| Coronary calcium score | |
| Mean (SD) | 98.5 (290.18) |
| Median (IQR) | 0 (0–43.91) |
| Range | 0–3897 |
SD standard deviation IQR interquartile range
| Case | Coronary calcium score total | p value | |
|---|---|---|---|
| Mean (SD) | Median (IQR) | ||
| Coronary artery disease (CAD) | |||
| No CAD (n=492) | 0 | 0.00 (0) | <0.001 |
| Non-obstructive CAD (mild, n=244) | 94.58 (215.030) | 16.70 (0–92.74) | |
| Obstructive CAD (moderate+severe, n=214) | 329.34 (496.449) | 157.87 (31.35–397.65) | |
| Mann–Whitney U-test | |||
| No CAD | Mild (non-obstructive CAD) | <0.001 | |
| Obstructive CAD (moderate+severe) | <0.001 | ||
| Mild (non-obstructive CAD) | Obstructive CAD (moderate+severe) | <0.001 | |
IQR interquartile range SD standard deviation
EFV was calculated in all patients with similar results. A higher volume of regional fat was noted with increasing severity of CAD. The presence of calcium at an extracoronary site was found in 207 patients (21.8%). The most common site of calcification was thoracic aorta, whereas the least common site was mitral valve. The prevalence of traditional cardiovascular risk factors across the thoracic ECC sites is given in Table IIIa. The number of thoracic ECC sites in various CCS groups is given in Table IIIb.
| Characteristic | Number of extracoronary calcium sites (%) | ||||
|---|---|---|---|---|---|
| 0 (n=743, 78.2%) | 1 (n=128, 13.5%) | 2 (n=60, 6.3%) | 3 (n=18, 1.9%) | 4 (n=1, 0.1%) | |
| Age (mean, median) | 48.44, 49 | 58.27, 58 | 64.23, 64 | 64.78, 64 | 73, 73 |
| Men | 482 (64.87) | 85 (66.40) | 43 (71.67) | 13 (72.22) | 0 |
| Smoking | 90 (12.1) | 21 (16.4) | 3 (5.0) | 2 (11.1) | 0 |
| Hypertension | 279 (37.5) | 73 (57.0) | 39 (65.0) | 8 (44.4) | 1 (100) |
| Diabetes mellitus | 135 (18.2) | 37 (28.9) | 24 (40.0) | 6 (33.3) | 1 (100) |
| Family history of CAD | 167 (22.5) | 35 (27.3) | 17 (28.3) | 0 | 1 (100) |
| Dyslipidaemia | |||||
| High serum cholesterol | 161 (21.7) | 37 (28.9) | 15 (25.0) | 4 (22.2) | 1 (100) |
| Low serum HDL | 44 (5.9) | 10 (7.8) | 8 (13.3) | 3 (16.7) | 0 |
| High serum TG | 114 (15.3) | 21 (16.4) | 10 (16.7) | 2 (11.1) | 0 |
CAD coronary artery disease HDL high-density lipoprotein TG triglyceride
| Coronary calcium score (n=950) | Number of extracoronary calcium sites (%) | ||||
|---|---|---|---|---|---|
| 0 (n=743, 78.2%) | 1 (n=128, 13.5%) | 2 (n=60, 6.3%) | 3 (n=18, 1.9%) | 4 (n=1, 0.1%) | |
| Normal: 0 (583, 61.4%) | 554 (95.02) | 27 (4.63) | 2 (0.3) | 0 | 0 |
| Minimal: 1–9 (49, 5.1%) | 37 (75.51) | 6 (12.24) | 5 (10.20) | 1 (2.04) | 0 |
| Mild: 10–99 (133, 14%) | 86 (64.66) | 33 (24.81) | 12 (9.02) | 2 (1.50) | 0 |
| Moderate: 100–399 (118, 12.4%) | 46 (38.98) | 41 (34.74) | 24 (20.34) | 7 (5.93) | 0 |
| Severe: >400 (67, 7.1%) | 20 (29.85) | 21 (31.34) | 17 (25.37) | 8 (11.94) | 1 (1.49) |
On taking into account the presence of thoracic extracoronary calcium in at least one site, the sensitivity, specificity, PPV and NPV for the presence of CAD were 40.6%, 95.7%, 89.9% and 63.4%, respectively, with a diagnostic accuracy of 69.2%. All patients with a CCS of 0 (n=583) were categorized into two groups based on the absence or presence of CAD (n=492 and 91, respectively). Subsequently, the median EFV and presence of ECC were compared between the two groups (Table IV). The median values of EFV were significantly higher in the ‘CAD present and CCS=0’ group compared to the ‘CAD absent and CCS=0’ group (p<0.001). Presence of thoracic ECC involving at least single site was seen in only 6 of the 91 patients.
| Group | Epicardial fat volume | |
|---|---|---|
| Mean (SD) | Median | |
| CAD present and CCS=0, 91 cases | 69.07 (27.54) | 64.72 |
| CAD absent and CCS=0, 492 cases | 56.69 (27.65) | 51.802 |
p<0.001 CAD coronary artery disease CCS coronary calcium score SD standard deviation
It was observed that when the combination ‘EFV and/or CCS’ is considered for the detection of presence of CAD, the sensitivity and NPV for predicting CAD significantly improved compared to either of them taken in isolation (95% and 90.7%, respectively). However, the specificity had reduced (45.9%). When the ECC is taken together with CCS and EFV, no further improvement in sensitivity or NPV was observed (95% and 90.5%, respectively). Therefore, considering EFV together with CCS may provide an added advantage for CAD screening, as it can identify those cases who had CAD with a 0-calcium score (due to non-calcified plaques), thereby improving the sensitivity and NPV. When ROC curves were plotted, the combination of CCS and ECC was found to have the highest AUC (>0.80); however, the sensitivity and NPV were 81.4% and 84.7%, respectively (lower than those observed with the abovementioned combination of fat volume and calcium score). These results are given in Table V. On multivariate analysis, ECC was not found to be an independent predictor of CAD.
| ‘No CAD’ versus ‘CAD present’ | AUC | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Accuracy (%) | p |
|---|---|---|---|---|---|---|---|
| EFV and/or CCS total | 0.705 | 95.0 | 45.9 | 62.1 | 90.7 | 69.58 | <0.001 |
| EFV and/or ECC total | 0.655 | 86.2 | 44.7 | 59.2 | 77.7 | 64.7 | <0.001 |
| CCS total and/or ECC total | 0.885 | 81.4 | 95.5 | 94.4 | 84.7 | 88.7 | <0.001 |
| EFV and/or CCS total and/or ECC total | 0.698 | 95.0 | 44.7 | 61.5 | 90.5 | 68.9 | <0.001 |
Cut-offs used: EFV-> or <49.75 ml; CCS -0 or >0; ECC -0 or >0 AUC area under the curve CAD coronary artery disease CCS coronary calcium score ECC extracoronary calcium EFV epicardial fat volume PPV positive predictive value NPV negative predictive value
DISCUSSION
CCS is a time-tested tool for the evaluation of coronary atherosclerosis and a predictor of future cardiovascular events. It is well known that the presence of calcium in the coronary arteries is pathognomonic of atherosclerosis. The total CCS is a representation of the overall coronary plaque burden.6–12 Asymptomatic patients without any detectable coronary calcium have a low prevalence of CAD and have a good prognosis.13–20 CCS has outperformed the veracity of conventional risk factors for CAD, carotid intima media thickness and highly sensitive C-reactive protein as a predictor of cardiovascular events, in both symptomatic and asymptomatic patients. The relevant prognostic information obtained using CCS may be useful to initiate or intensify appropriate treatment strategies to slow atherosclerotic disease progression.21 Although the absence of coronary calcification has a high NPV for ruling out presence of atherosclerosis, a number of patients with non-calcified or mixed density coronary atherosclerotic plaques may escape detection or be underestimated by assessing CCS alone. This has been evaluated in previous studies by Gottlieb et al.22 and Morita et al.23 It has been proposed that patients with acute coronary syndrome were found to have higher prevalence of non-calcified vulnerable plaques rather than calcified plaques, in contrast to patients with stable CAD.24,25
In such cases, the newer non-traditional tool for cardiovascular risk prediction—EFV coupled with estimation of ECC—can help improve prediction of CAD. Our previous study showed higher values of EFV in patients with higher degree of coronary artery stenosis. Moreover, it was an independent risk factor for the presence of CAD.5 In the present study, it was observed that the subset of patients with even mild CAD but a CCS of 0 had significantly higher median values of EFV compared to the patients without CAD. This not only strengthens the fact of EFV being an independent contributing risk factor for detection of CAD, but also implies a possibility that it may even predate CCS as a CAD risk predictor. After multivariate adjustment in patients with a 0-calcium score, Ito et al. had found EFV to be a significant predictor of obstructive CAD, and its utility as an important marker for CAD in symptomatic patients with non-calcified plaques.26
A graded association of increasing amount of multisite extracoronary calcium with higher CAD and mortality risk has been suggested in previous studies, and the information supplemented the traditional cardiovascular risk markers.27 In our study, although multisite ECC was more frequently seen in patients with CAD, especially obstructive CAD compared to patients without CAD, ECC if considered alone was found to be a poor predictor of CAD. Moreover, when considering ECC together with CCS and EFV, no further improvement in CAD detection was achieved. Although the AUC for combination of ECC and CCS was maximum, the sensitivity and NPV were lower compared to that of other combinations.
There are a few limitations of our study. First, for any new suggested diagnostic criteria, it has to be validated. Ideally, two datasets should be made a test dataset and a validation dataset (having similar characteristics). The results of the test dataset have to be applied on the validation dataset. However, for our study, a sequential study needs to be designed for studying the results. Another limitation is lack of follow-up of the patients enrolled in the study, to look for any major adverse cardiovascular events as well as CAD progression.
Conclusions
We advocate the combined use of CCS along with EFV to serve as a more robust model for predicting CAD. Future research should determine the prognostic value of EFV and pericardial fat volume, their distribution and comparative analysis with abdominal fat estimation and the perivascular fat attenuation index with the development of extensive normograms for early cardiovascular risk prediction. These can be useful adjuncts in primary prevention of a cardiovascular event with no additional radiation burden or expenditure to the patient as these are analysed on the same set of non-contrast CT images obtained for the estimation of coronary artery calcium. The research is capable of catapulting individualized CAD risk profiling to a higher and more sensitive level. Moreover, it also expands the utility of CT as a modality for CAD prediction and evaluation: predating CCS by EFV on the one end of the spectrum, visualization and characterization of vulnerable plaques on dual source CT, and finally FFR-CT for physiological assessment of stenosis at the other end of the spectrum.
ACKNOWLEDGEMENTS
We acknowledge the contributions of all the participants of the study and efforts of each team member of the Department of CT and MRI, Sir Ganga Ram Hospital, New Delhi, India.
Conflicts of interest
None declared
References
- Cardiovascular diseases in India: Current epidemiology and future directions. Circulation. 2016;133:1605-20.
- [CrossRef] [PubMed] [Google Scholar]
- Heart disease and stroke statistics-2012 update: A report from the American Heart Association. Circulation. 2012;125:e2-220.
- [Google Scholar]
- Cardiovascular morbidity and mortality in community-dwelling elderly individuals with calcification of the fibrous skeleton of the base of the heart and aortosclerosis (The Cardiovascular Health Study) Am J Cardiol. 2006;97:1281-6.
- [CrossRef] [PubMed] [Google Scholar]
- Calcified atherosclerosis in different vascular beds and the risk of mortality. Arterioscler Thromb Vasc Biol. 2012;32:140-6.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation of epicardial fat quantification with severity of coronary artery disease: A study in Indian population. Indian Heart J. 2018;70:S140-S145.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of coronary artery disease by cardiac computed tomography: A scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761-91.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation. 1995;92:2157-62.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of electron beam computed tomography with intracoronary ultrasound and coronary angiography for detection of coronary atherosclerosis. J Am Coll Cardiol. 1997;30:57-64.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants and correlates of target lesion calcium in coronary artery disease: A clinical, angiographic and intravascular ultrasound study. J Am Coll Cardiol. 1997;29:268-74.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic value of coronary calcification and angiographic stenoses in patients undergoing coronary angiography. J Am Coll Cardiol. 1996;27:285-90.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary calcium and standard risk factors in symptomatic patients referred for coronary angiography. Am Heart J. 1998;135:696-702.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term prognostic value of coronary calcification detected by electron-beam computed tomography in patients undergoing coronary angiography. Circulation. 2001;104:412-17.
- [CrossRef] [PubMed] [Google Scholar]
- Electron-beam tomography coronary artery calcium and cardiac events: A 37-month follow-up of 5635 initially asymptomatic low-to intermediate-risk adults. Circulation. 2003;107:2571-6.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term prognosis associated with coronary calcification: Observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49:1860-70.
- [CrossRef] [PubMed] [Google Scholar]
- Absence of coronary calcification on double-helical CT scans: Predictor of angiographically normal coronary arteries in elderly women? Radiology. 1996;199:665-8.
- [CrossRef] [PubMed] [Google Scholar]
- Use of electron-beam computed tomography in the evaluation of chest pain patients in the emergency department. Ann Emerg Med. 1999;33:15-21.
- [CrossRef] [PubMed] [Google Scholar]
- Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography. Circulation. 2002;105:1791-6.
- [CrossRef] [PubMed] [Google Scholar]
- The extent of coronary calcium by electron beam computed tomography discriminates the likelihood of abnormal myocardial perfusion on SPECT. Circulation. 2000;102:543.
- [Google Scholar]
- Absent coronary artery calcium excludes inducible myocardial ischemia on computed tomography/positron emission tomography. Int J Cardiol. 2011;147:424-7.
- [CrossRef] [PubMed] [Google Scholar]
- Negative calcium score and the presence of obstructive coronary lesions in patients with intermediate CAD probability. Int J Cardiol. 2011;148:e16-e18.
- [CrossRef] [PubMed] [Google Scholar]
- Expert review on coronary calcium. Vasc Health Risk Manag. 2008;4:315-24.
- [CrossRef] [PubMed] [Google Scholar]
- The absence of coronary calcification does not exclude obstructive coronary artery disease or the need for revascularization in patients referred for conventional coronary angiography. J Am Coll Cardiol. 2010;55:627-34.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of computed tomographic angiography-verified high-risk plaques and significant luminal stenosis in patients with zero coronary calcium score. Int J Cardiol. 2012;158:272-8.
- [CrossRef] [PubMed] [Google Scholar]
- Noninvasive assessment of plaque morphology and composition in culprit and stable lesions in acute coronary syndrome and stable lesions in stable angina by multidetector computed tomography. J Am Coll Cardiol. 2006;47:1655-62.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of plaque texture by means of multislice computed tomography in patients with acute coronary syndrome and stable angina. Circ J. 2004;68:840-4.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of epicardial fat volume on coronary plaque vulnerability: Insight from optical coherence tomography analysis. Eur Heart J Cardiovasc Imaging. 2012;13:408-15.
- [CrossRef] [PubMed] [Google Scholar]
- Multisite extracoronary calcification indicates increased risk of coronary heart disease and all-cause mortality: The Multi-Ethnic Study of Atherosclerosis. J Cardiovasc Comput Tomogr. 2015;9:406-14.
- [CrossRef] [PubMed] [Google Scholar]




