Translate this page into:
Addressing disparities in rural and remote access for rheumatology practice through a transformative tele-healthcare delivery system: Experience of a large cohort of patients in eastern India
Correspondence to SANJAY KUMAR YADAV; sky1508@gmail.com
[To cite: Das BK, Parida MK, Tripathy SR, Pattanaik SS, Yadav SK, Mishra SK. Addressing disparities in rural and remote access for rheumatology practice through transformative tele-healthcare delivery system: Experience of a large cohort of patients in eastern India. Natl Med J India 2024;37:79–81. DOI: 10.25259/NMJI_182_2022]
Abstract
Background
We present the experience of telerheumatology consultation services carried out in an eastern state of India.
Methods
We did this prospective, observational study of patients with rheumatological disorders and followed through telemedicine between December 2015 and May 2019.
Results
During the study period, we provided teleconsultation to 3583 patients with the help of 11 201 telemedicine visits. Patients resided at a median distance of 248 (13 to 510) km from the telemedicine hub. The cumulative savings of the patients as a result of this service were ₹2.4 crore (24 million). The median travel time saved was 7 hours (30 minutes to 12 hours) per patient per visit and a median of ₹6700 was saved per visit per patient.
Conclusion
Sustained efforts over a long period can lead to the delivery of essential rheumatology services via telemedicine to an under-priviledged population, reduce the financial burden of the poor, and help women to access healthcare services in remote parts of low- and middle-income countries (LMICs).
INTRODUCTION
By 2030, the world population is projected to reach 8.6 billion and India would become the most populous country.1 At present, even developed countries are facing challenges to provide adequate healthcare. The situation is worse in low- and middle-income countries (LMICs). Telemedicine is conceived as one of the solutions to overcome this growing disparity. A pilot study on tele-rheumatology using the telephone was first reported by Pal2 in 1997. Since then, numerous publications have established its effectiveness in providing remote access care. However, most of these publications are from developed countries. We share our experience of tele-rheumatology services carried out in Odisha, eastern India. Odisha is among the lowest per capita income (₹82 000) states of India. It is also ranked lowest in a health survey index conducted by Niti Aayog in 2018.3
METHODS
We did this prospective observational study between December 2015 and May 2019, in the Department of Rheumatology, Shriram Chandra Bhanj Medical College and Hospital (SCB MCH), Cuttack, India. A total of 3583 patients with rheumatological disorders who preferred telemedicine follow-up for financial reasons were enrolled. The study was approved by the Institutional Ethics Committee.
Telemedicine services
The SCB MCH, Cuttack started telemedicine services in Odisha in 2001 with guidance from the Department of Information Technology, Government of India and the Sanjay Gandhi Post Graduate Institute of Medical Sciences (SGPGIMS), Lucknow. Subsequently, in the same year, the Indian Space Research Organization (ISRO) provided the necessary infrastructure and human resource. The Odisha Telemedicine Network was expanded in 2011 with funding from the state government and all 30 district headquarters were provided telemedicine facilities (Fig. 1).
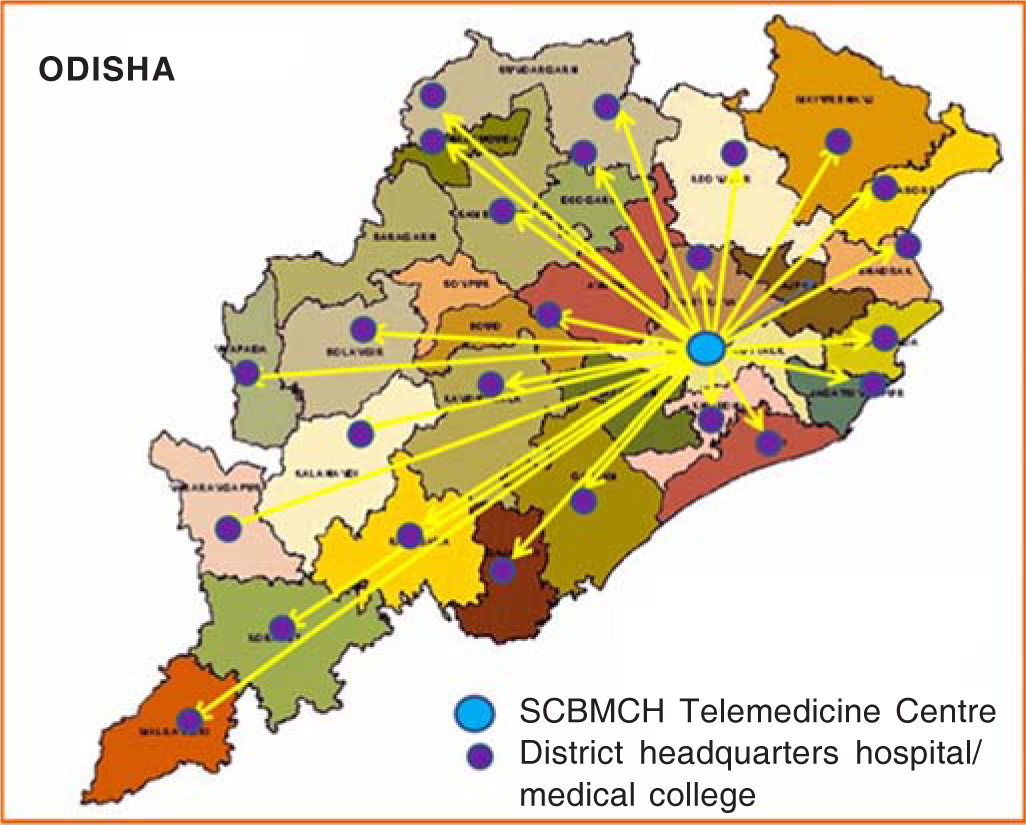
- Thirty-two telemedicine nodal centres connected to SCB Medical College and Hospital (MCH) telemedicine hub
All the district-level telemedicine centres are connected to the SCB MCH, Cuttack. The Bharat Sanchar Nigam Limited (BSNL) was the primary communication tool provider and used MPLS-VPN/VPNoBB connectivity. An upload and download speed up to 2 Mbps and with unlimited data volume was made available. The Centre for Development of Advanced Computing (CDAC), Pune implemented this project on a BOT (Build, Operate, and Transfer) model. The expenditure for implementation of the network was $688 000 excluding connectivity charges of $51 000 for the first year. At present, this platform is being used to provide telemedicine services.
Tele-follow-up
Patients visiting our rheumatology outpatient department (OPD) at SCB MCH were evaluated, diagnosed and advised about the management plan and follow-up requirement. Patients are counselled to attend the tele-follow-up from the nearest district telemedicine nodes. All patients who agreed were given an appointment with the hub. Patients could visit the telemedicine nodes on specific days of the week. In case of an emergency, they were advised to report to the nearest health centre or the nearest medical college. Since patients were required to visit the nodal centres, which are primary/community health centres, they usually have all the basic laboratory services, medications and emergency injectables.
Outcome data
We collected data at each follow-up. Our patients included those whose per capita income was below the national average and were issued BPL (below the poverty line) certificates by the Government of India. To ensure compliance with national and provincial law pertaining to telemedicine practice the patients were informed and consent obtained regarding the data collection, retention and the right to withdraw if not willing to participate in the study.
RESULTS
During the study period (December 2015 to May 2019), we provided teleconsultation to 3583 patients over 11 201 tele-medicine visits. The majority of patients were women (66%) and the commonest age group was 41–60 years (1556, 43.4%) followed by 21–40 years (1425, 39.8%) and >60 years (442, 12.3%; Table I).
| Characteristic | n |
|---|---|
| Age groups (years) | |
| 10–20 | 1 6 0 |
| 21–40 | 1425 |
| 41–60 | 1556 |
| >60 | 4 4 2 |
| Gender | |
| Men | 1218 |
| Women | 2365 |
| Patient home district distance from hub (median) | 400 km (range 21–821) |
| Primary visit diagnosis | |
| Rheumatoid arthritis | 2257 |
| Seronegative spondyloarthropathies | 5 7 3 |
| Juvenile idiopathic osteoarthritis | 2 1 5 |
| Osteoarthritis | 2 1 5 |
| Systemic lupus erythematosus | 1 7 9 |
| Other (sarcoid, systemic sclerosis, dermatomyositis, etc.) | 1 4 4 |
| Below poverty line (income less than $11.16 per capita per month for rural areas and $13.80 per capita per month for urban areas) | 1469 |
| Literacy level | |
| Illiterate | 1648 |
| Primary | 9 6 7 |
| Intermediate | 4 7 0 |
| Graduation and above | 4 9 8 |
| Patients from tribal areas | 1362 |
The patients lived at a median distance of 248 (13 to 510) km from the SCB MCH telemedicine hub and 10–60 km from the nearest health centre. The most common disorders were rheumatoid arthritis (63%) followed by spondyloarthritis (16%), juvenile idiopathic arthritis and osteoarthritis (6% each), systemic lupus erythematosus (5%) and others (3%; Table I). Patients were managed based on their complaints, locally procured investigation reports and previous prescriptions. Most were under control with analgesics/non-steroidal anti-inflammatory drugs (NSAIDs) and disease-modifying anti-rheumatic drugs (DMARDs). Patients observed to be sick or with fresh complaints were advised to consult their local physicians or get admitted to the nearest medical college depending on the situation (Table I).
A total of 1110 (31%) patients had single visit, 645 (18%) had two visits, 430 (12%) had three visits and 1397 (39%) had more than four visits to the telemedicine hub. All were follow-up visits and the average time spent on each consultation was 5–10 minutes. On analysis, it was deduced that if 11 201 visits had been done physically to SCB MCH then patients would have had to travel 3 227 889 cumulative kilometres. Patients’ financial savings by opting for tele-rheumatology care were calculated appropriately by combining second class travel cost by railways or travel by bus, the commonest mode of transport from rural areas, plus food and lodging for a day. Total cumulative savings were `2.4 crore (24 million). The median travel time saved was 7 hours (30 minutes to 12 hours) per patient per visit and a median of `6700 was saved per visit per patient, which is a large saving for a poor rural patient.
We did not have a control arm (physical follow-up) to compare the satisfaction with the tele-follow-up group. But at the end of each follow-up session, we asked if patients were satisfied with the consultation. None of the patients reported that they were not satisfied with the telemedicine follow-up and wanted a physical visit instead. Few patients were required to visit the hub for their annual investigations, injections, etc. These numbers were small (5–10 patients per month).
DISCUSSION
Our study presents the observations of a specialized centre located in a state which is below the national average on many health indicators. This is probably the largest cohort of rheumatology patients being followed-up via telemedicine in a comparatively backward state of India with a large number of below poverty line (BPL) persons, and a substantial tribal population with low literacy rate.
We reviewed the scientific literature extensively and found successful implementation of tele-rheumatology programmes in many developed countries covering rural regions.4–10 Poulsen et al.10 reported that telemedicine service supplements the 3-monthly physical visits between Townsville Hospital and Mount Isa, a remote town in Queensland. The distance between Mount Isa and Townsville is approximately 900 km and takes nearly 10 hours travel time. Rural patients preferred telemedicine over face-to-face visits as it saved extensive travelling. In our study, apart from travel hours, financial savings were another major factor in choosing telemedicine. Another randomized controlled intervention trial from follow-up clinics in rural Saskatchewan reported the effectiveness of tele-rheumatology in Canada.9 However, both these studies were from developed countries where rural communities are well educated and have a high per capita income. Compared to this population, Odisha’s per capita income was `82 000 for the financial year 2017–18, one of the lowest among Indian states. This low financial status leads to an out-of-pocket expenditure for the patient and further burdening their family financially. Such a situation leaves only a few options for poor patients. Most of them forgo treatment and just suffer in pain and hope for the best, some go for alternative and local medicines, to continue with allopathic treatment some have to borrow heavily or sell whatever assets they have, which further pushes them deeper into poverty.
Another peculiar barrier to healthcare in LMICs is gender disparity. A large public hospital in Delhi, India11 has reported that about 400 000 women patients missed their outpatient visits from the states of Delhi, Haryana, Uttar Pradesh and Bihar, which was 50% of the total appointments for women. Unfortunately, these states are far better than Odisha in healthcare indices and economy. Women face discrimination while receiving healthcare when it amounts to out-of-pocket expenditure or distressed family financial situation.12 This gender disparity in healthcare financing implies that the male members of the household are prioritized when distressed financing is required and healthcare expenditure on women is generally of lower priority.12 These observations highlight the importance of telemedicine in LMICs, with regard to gender disparity in healthcare expenditure. Our observations indicate that 66% of users of telemedicine programmes were women.
Furthermore, officially known as ‘tribals’ or ‘adivasis’, Odisha is home to 10% of India’s total tribal population, which constitutes more than 22.5% of the state’s population. The Government of India recognizes these indigenous populations by national legislation termed ‘Scheduled Tribes’. Of 62 tribal communities of Odisha, 13 are known as ‘Particularly Vulnerable Tribal Groups’.13 Our cohort had a large number of patients from tribal areas. This unique observation reiterates that telemedicine programmes can help in overcoming gender disparity, racial inequality, provide access to quality healthcare and prevent the financial burden of poor patients.
However, there are certain limitations in our study. The absence of doctors at teleconsultation centres in district headquarter hospitals led to difficulty in physical examination and in treating new patients. Patients not seen by a rheumatologist earlier have to visit the hub for comprehensive examination, investigation and management. Patients also need to visit the hub for annual investigations or injectables. Another limitation is the lack of a control arm to assess satisfaction. Cost calculations were also indirect as it is difficult to measure and verify expenditure incurred by each patient with the available resources. Despite these barriers, sustained efforts have led to better care of patients with rheumatological disorders residing in remote parts of the state by using the telemedicine service: a model for providing specialist care nearest to their residence.
Conclusion
Our tele-rheumatology facility decreased long distance travel, with reduced loss of wages and helped avoid difficulties associated with travelling for a patient with arthritis in crowded public transports. Quality rheumatology follow-up consultation can be effectively delivered via telemedicine to an under-priviledged population and less cared for women patients residing in remote parts of LMICs. Sustained effort is required before a considerable outcome is discernible.
Conflicts of interest
None declared
References
- Telemedicine. Pilot study of telephone follow up in rheumatology has just been completed. BMJ. 1997;314:520-1.
- [CrossRef] [PubMed] [Google Scholar]
- Healthy States Progressive India: Report on the ranks of states and Union Territories. Published online June 2019. Available at http://social.niti.gov.in/uploads/sample/health_index_report.pdf (accessed on 3 Jan 2024)
- [Google Scholar]
- Outcomes, satisfaction, and costs of a rheumatology telemedicine program: A longitudinal evaluation. J Clin Rheumatol. 2019;25:41-4.
- [CrossRef] [PubMed] [Google Scholar]
- Telemedicine and other care models in pediatric rheumatology: An exploratory study of parents' perceptions of barriers to care and care preferences. Pediatr Rheumatol. 2017;15:55.
- [CrossRef] [PubMed] [Google Scholar]
- Rheumatology care using telemedicine. Telemed J E Health. 2020;26:335-40.
- [CrossRef] [PubMed] [Google Scholar]
- Telerheumatology: A technology appropriate for virtually all. Semin Arthritis Rheumatism. 2016;46:380-5.
- [CrossRef] [PubMed] [Google Scholar]
- Addressing rural and remote access disparities for patients with inflammatory arthritis through videoconferencing and innovative interprofessional care models. Musculoskeletal Care. 2018;16:90-5.
- [CrossRef] [Google Scholar]
- Telehealth followup strategy for tight control of disease activity in rheumatoid arthritis: Results of a randomized controlled trial. Arthritis Care Res. 2018;70:353-60.
- [CrossRef] [Google Scholar]
- Satisfaction with rural rheumatology telemedicine service. Int J Rheum Dis. 2015;18:304-14.
- [CrossRef] [PubMed] [Google Scholar]
- Missing female patients: An observational analysis of sex ratio among outpatients in a referral tertiary care public hospital in India. BMJ Open. 2019;9:e026850.
- [CrossRef] [PubMed] [Google Scholar]
- Gender disparities in health care expenditures and financing strategies (HCFS) for inpatient care in India. SSM Popul Health. 2019;9:100372.
- [CrossRef] [PubMed] [Google Scholar]
- Census of India 2001. Published online 2001. Available at https://censusindia.gov.in/Tables_Published/SCST/dh_st_orissa.pdf (accessed on 10 Jan 2021)
- [Google Scholar]




