Translate this page into:
Approach to family assessment and intervention
Corresponding Author:
Anand Krishnan
All India Institute of Medical Sciences, Ansari Nagar, New Delhi 110029
India
kanandiyer@yahoo.com
| How to cite this article: Krishnan A, Behera P, Nongkynrih B. Approach to family assessment and intervention. Natl Med J India 2017;30:279-284 |
Abstract
Background. Family studies are an integral part of teaching of community medicine to all undergraduate medical and nursing students. It enhances the understanding of students about social determinants and multifactorial causation of disease. However, there is no standard approach towards it and it is seen as a clinical presentation with some elements of family included. We describe a systematic and comprehensive approach to a family study.Methods. Based on the existing literature and personal experience, we identified 11 domains under the acronym Family ASSESSMENT—Structure, Socioeconomic, Sickness, Nutritional, Educational, Environmental, Affordability, System (health), Mental, Family influence, Threats. Under each domain, we present indicative diagnoses and possible solutions. We also suggest that these domain diagnoses can be integrated into a single ‘web of interaction’ which provides a comprehensive understanding of the issues and guides us towards identifying the solutions.
Results. We use a worked out example of a case of tuberculosis to demonstrate the use of this approach and develop a rich web of interaction, which is then linked to identification of possible approaches towards mitigating the impact of disease on the individual and the family. Some suggestions to the departments of community medicine on organizing family studies are also provided.
Conclusion. Availability of a systematic and comprehensive approach would improve students’ understanding of the social model of disease and multifactorial causation of disease. It will also provide a standardized method of teaching this important component of community medicine nationally.
Introduction
Medicine is both a science and an art. Though qualitative components such as ethics and values play an important role in providing medical services, medical education focuses largely on quantitative aspects. Case studies are used in the social sciences to teach qualitative aspects. Clinical case presentations, a form of case study are used in medicine to teach clinical skills, diagnostic reasoning and planning treatment of individual patients. The way of making clinical presentations has remained unchanged for decades.[1] In the social sciences and life sciences, a case study involves an up-close, in-depth and detailed examination of a subject of study (the case), as well as its related contextual conditions.[2] Although no single definition of the case study exists, Thomas defines a case study as ‘analyses of persons, events, decisions, periods, projects, policies, institutions or other systems that are studied holistically by one or more method. The case that is the subject of the enquiry will be an instance of a class of phenomena that provides an analytical frame—an object—within which the study is conducted and which the case illuminates and explicates.‘[3]
Departments of Community and Family Medicine use what is varyingly named as clinico-psycho-social or clinico-social case studies or just family presentations. These are typical clinical case presentations with an added description of family members, socioeconomic status, dietary history and household environment. The focus is on the clinical aspect, reflecting the overwhelmingly clinical training that students undergo as part of their medical education. The web of causation reflects a medical model of disease. The fact that the student visited the case in their home adds little value to the insight the student gains about the disease, its causation or management of the patient or the community-level determinants. One of the reasons for this variation and poor quality is the lack of guidance available on how to do it well.[4],[5] Books are more concerned with definitions and classifications and how to answer viva examination rather than fostering critical thinking in the student. Much better theoretical and practical guidance are available for nurses.[6],[7]
We describe here a framework for studying families and also provide guidance on how to facilitate a good family study. The focus of the paper is not to provide the student with the tools required to do a comprehensive family assessment but on how to synthesize the assessments into a single narrative for better understanding and management.
Objectives of a Family Study
The objectives of a family study state the student should be able to think beyond medical models of disease to social models of disease. They have to understand that there are larger social influences which are more, if not equally, important to medicine, in determining who develops sickness or its consequences. They should understand the role and influence of family members on the disease and its progress as well as the impact of disease on other family members. Family is a social unit and its members influence each other both positively and negatively. Knowledge of this is essential to tackle the health problem effectively. Finally, they should be able to plan a comprehensive intervention that addresses family-level determinants and consequences and also optimally leverages the resources available within the family. Adapting the framework of the Commission of Social Determinants of Health, a family study should:
- identify the composite determinants of health affecting the particular family;
- show how the major determinants relate to each other;
- clarify the mechanisms by which these determinants act to decrease health;
- provide a framework for evaluating which of these are the most important to address; and
- map specific interventions for improvement of the health of the family.[8]
Just like an index case (patient) is an entry point into a family, a family is an entry point into the community. Therefore, we also use the family study to gain insight into the larger health issues in the community. The appreciation of the economic, social, environmental and emotional aspects in the medical problems should result in a change in their attitude and approach to patients.[9] This is essential if we want doctors to engage with the community and perform social roles.[10]
Before we proceed with the framework, let us understand the role of family in health and disease. Family has influence at three levels—causation and progress of the disease; the consequences of the disease on other family members; and how family copes with the disease. These are illustrated below.
Causation
This could include spread of infection from a family member to the index case (tuberculosis, scabies, etc.) or genetic or shared lifestyle (tobacco use, intra-household distribution of food in cases of an undernourished child or an obese mother).
Consequences
The index case can be a source of infection to other family members. The expenditure incurred on treatment of the index case can push the family into impoverishment or school absenteeism of a girl child.
Coping
One of the greatest benefits that a family provides to its members is in terms of financial and emotional support to cope with the problem, which may be different for different diseases. Failure of coping leads to stress which can be measured.
A Family ‘Assessment’ Approach for Family Study in Medicine
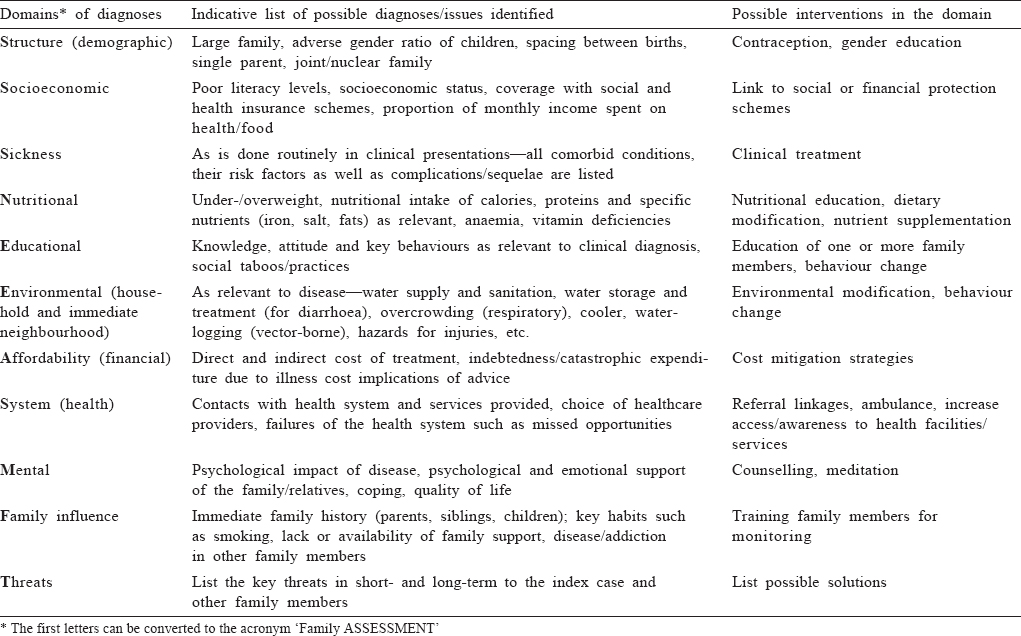
Family presentations are usually built around an index case. We describe eleven domains in which the family should be studied, each resulting in a diagnosis in that domain. While the sequence shown in [Table - 1] is desirable, as an aide de memoire, we have coined the term ‘Family ASSESSMENT’. We emphasize that the points made under each domain are not exhaustive but only indicative. Students should assess the specific situation and adapt the approach accordingly. Also, it is not necessary that all domains would need to be studied in complete detail in all cases.
Structure (demographic)
This section describes the composition of the family in terms of age, sex and relationships. Some of the possible diagnoses in this domain are large (or small) family, presence of eligible couple, elderly, lack of spacing between children, single parent, etc.
Socioeconomic
This follows from the information on education, income and occupation of the members, including the head of the household, ownership of land/house and enables measurement of the socioeconomic status of the family using standard scales. Knowledge about caste and poverty status also enables an assessment of their eligibility to various social schemes of the government. Similarly, knowledge whether the breadwinner is in organized/unorganized, government/private sector, regular/ contractual job gives an idea about the financial security of the family.
Sickness
The choice of the word ‘sickness’, though driven by the need for acronym, also highlights the social aspect of the disease rather than the medical aspect. A standard approach adopted in wards for making a diagnosis can be used. In family presentations, the focus should not be on learning clinical skills or making diagnoses. A diagnosis is important as it binds the whole presentation together. However, a change in diagnosis does not change other aspects and therefore, our approach to management. For example, whether the patient has atrial or mitral stenosis, or haemorrhagic or thrombotic stoke, has little implications for other domains.
Nutritional
Standard techniques of nutritional assessment should be used such as 24-hour dietary recall, anthropometry, blood levels of nutrients or related haematological parameters. The diagnoses would be in the form of degree of under-/over-nutrition; excess or deficiency of a specific nutrient (salt, vitamin A, etc.) intake. Utilization and access of existing nutritional programme such as the Integrated Child Development Services (ICDS) Scheme or iodized salt would also be included in this section.
Educational
This domain covers key issues related to awareness of the causes and consequences of the disease, key behaviours and social customs and taboos which could influence the disease or its prognosis. This enables patient education programme to be tailored to their beliefs.[11] In an undernourished child, this would include feeding practices and social customs related to breastfeeding and complementary feeding.
Environmental
This includes environment within the household as well as immediate neighbourhood. Only those aspects relevant to the index case should be studied. For example, in a case of diarrhoea (or oro-faecally transmitted diseases) one needs to look into source of water supply, access, availability, water storage, treatment and retrieval practices at home. It would be different for a vector-borne disease (breeding places, use of anti-adult measures) or in non-communicable diseases (NCDs) (park nearby) and so on.
Mental
The impact of the disease on the mental health of an individual and family and their coping strategies should be documented. Stress in the cases/caregivers can also be assessed using simple 4-or 10-point scales. This is one of the weakest aspect of current family studies, primarily due to lack of competence of the faculty and lack of practical tools for use by students.
Family influence
Family members influence the occurrence of the disease either because of shared genes or behaviours. Decision-making in the family, especially on health matters should be studied. For example, in advising on contraception or breastfeeding, the mother-in-law may have to be counselled. Use of family members to assist the patient in monitoring disease (blood pressure or blood sugar) or drug adherence should be explored.
Affordability (financial)
The direct (cost of treatment) and indirect (loss of wages) burden of the disease needs to be documented. The impoverishment of the family due to disease should be studied. The cost implications of the advice being given should be considered. For example, often the dietary advice given by students cannot be afforded by the family and becomes an exercise in futility.
System (health)
Health professionals need to understand the larger health system to use it effectively. They should know the health services available in the local area and benefits available under various national programmes/schemes. The health-seeking behaviour (preference for a particular stream of medicine or facility) needs to be understood and factored in the advice. Reasons for utilization or non-utilization of government services available nearby should be explored. Missed opportunities by health system such as immunization and growth monitoring in under-5 children and opportunistic screening in adults should be identified.
Threats
At the end, based on the information provided, the student should identify short-term and long-term threats to the health and well-being of the index case and family, which need to be prevented.
A Synthesizing Framework
While the first step in studying a family is to make broad categories of diagnoses as listed above, the next crucial step is to integrate them into one framework. There is no one right way of doing this. The process of integration is crucial for the student to develop an insight into the complexity and multipolarity of issues. It could be a creative and enjoyable process and students should be given freedom to explore different forms of visual presentations during this stage. These could vary from simple (dividing into modifiable and non-modifiable, positive and negative factors) to complex webs or frameworks. Developing a ‘web of interaction’ is a way to understand the social model of disease. We call this a web of interaction and not causation, as it covers not only causation but also consequences and coping. In this step, all the diagnoses listed in the different domains above are pasted on a board/ paper/slide and linkages between them established. This process of putting arrows between different factors could be fun and a joint activity as well. Once the links are completed into one picture, the complex social model of the disease is revealed.
Complex models such as Fishbone Analysis (Ishikawa diagrams); Problem and Solution Trees (PAST) or using the Commission of Social Determinants of Health (CSDH) Framework can also be used. Fishbone analysis was developed as a quality control tool to discover the root cause of a problem and to graphically illustrate the relationship between an outcome and all the factors that influence it.[12],[13] Problem trees establish the context in which a problem is to be viewed and are made by stating the problem and asking ‘why’ till all whys are exhausted. Reversing the problem tree, by replacing negative statements with positive ones, creates a solution tree.[14],[15] CSDH proposed a framework with three elements: socioeconomic and political context; structural determinants and socioeconomic position and; intermediate determinants of health including biological, behavioural and health system-related factors.[8] These frameworks, though adaptable to a family level, have been described for use in an organization or a community rather than at individual or family level.
Comprehensive Management
For each domain of diagnosis, some measures for management can be identified. Some illustrative examples are shown in [Table - 1]. It needs to be understood that mere prescription of a medicine is not treatment of a disease. If a disease has to be fully addressed, other factors have to be taken into account. This is not only true for chronic diseases but also for acute infectious diseases such as malaria, dengue, diarrhoea or worm infestation. Just treatment of the current episode is poor management of the case, as it is likely that the disease will recur in the near future. Preventive actions to address short-and long-term threats should also be listed.
A Worked-Out Example
We illustrate our approach with an example of a family presentation where we implemented this approach for the first time. The web of interaction succinctly illustrates the multifactorial causation and social model of disease [Table - 2] and [Figure - 1]. It is evident that this family has several disadvantages—it has little social and family support, recent migration, and financial hardships. Tuberculosis has worsened the situation due to the catastrophic expenditure and incapacitation of the patient. The relevant national health programme has covered this patient and has ensured free treatment resulting in good compliance. A mere prescription of drugs by a clinician without addressing other serious issues would have almost certainly resulted in incomplete treatment, leading to multidrug resistance in the patient and the community. The threats that need to be prevented are default (due to poverty), higher risk of death (due to severe undernutrition and anaemia) and husband contracting the disease from the wife (alcoholism, inadequate advice on sputum disposal). In general, this case reflects failure of our social and financial protection programmes to cover the most vulnerable and also raises issues about the role of the private sector in providing affordable and good-quality treatment.
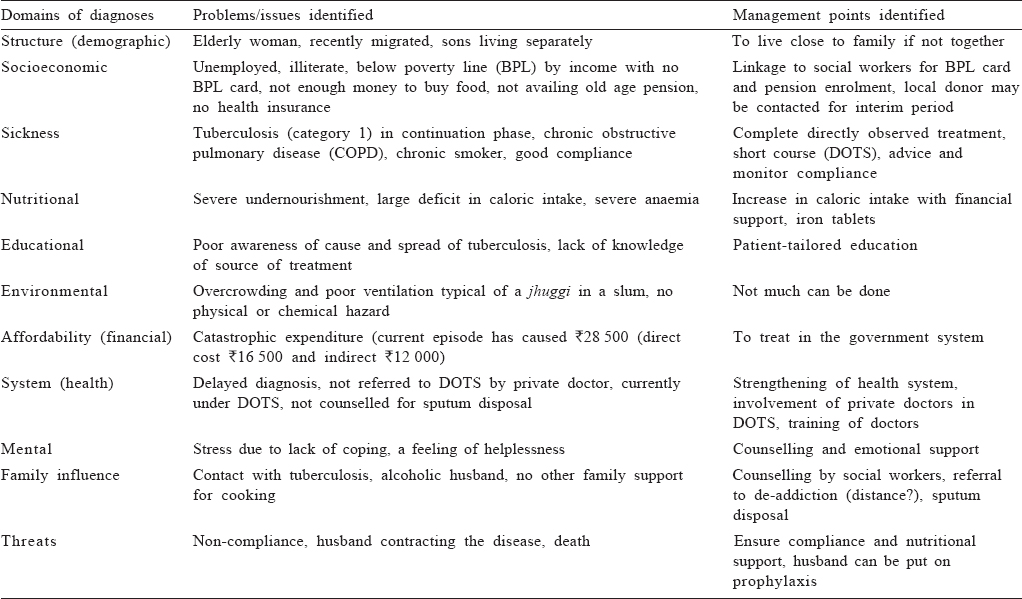
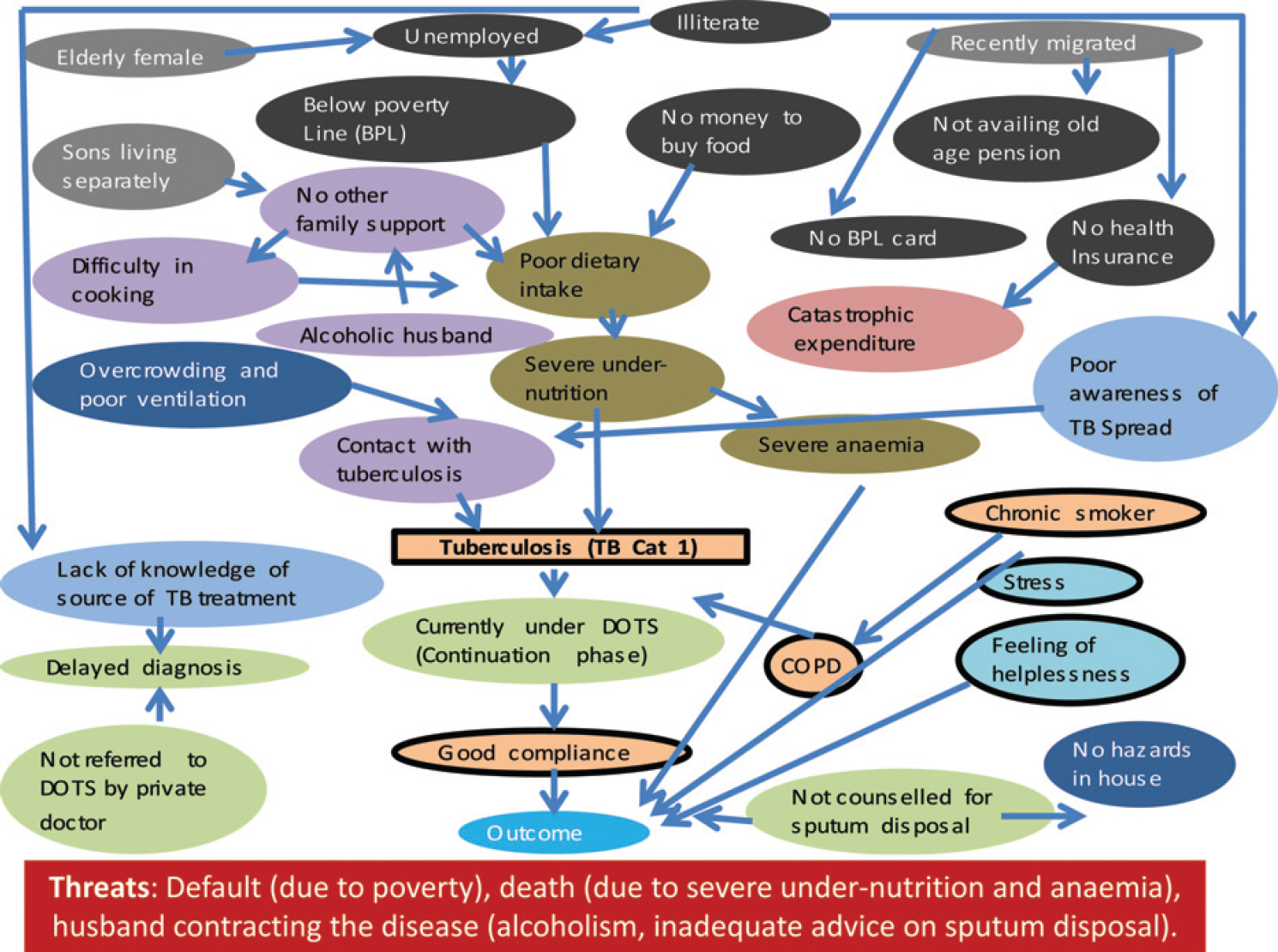 |
| Figure 1: An example of web of interaction of a patient with tuberculosis in a resettlement colony in Delhi DOTS directly observed treatment, short course COPD chronic obstructive pulmonary disease |
Tips on how to Facilitate a Good Family Study by Students
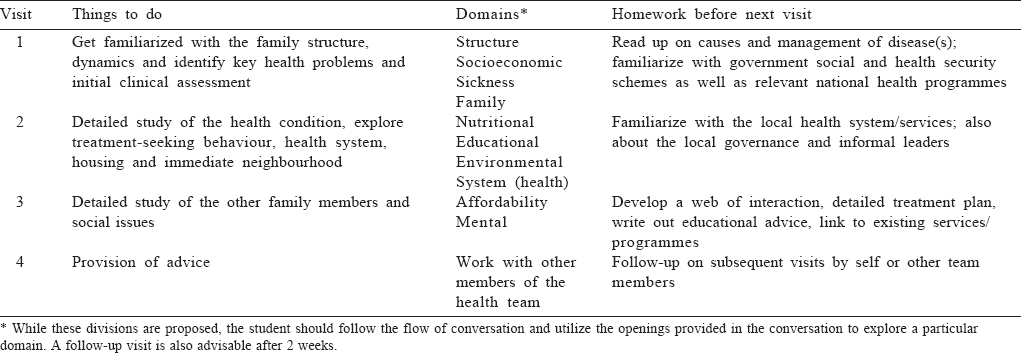
A good family study needs time which would decrease as students gain experience. For undergraduate students, we propose a schedule [Table - 3]. For postgraduates, we believe the process can be accelerated and 2 days should be sufficient. Alternatively, in colleges where there is a practice of allotting certain number of families (10 to 20) to postgraduates for follow up, the same families can be used with much shorter time period (2 hours). The visits should be timed in a manner that key family members are available at home and are able to spend time with the student. The students should be fluent in the local language and training in communication is essential. It is best that these studies are started in the third year (or maybe even earlier) of undergraduates before they are subsumed by their clinical training. It is important that the families are visited by the departmental team (a public health nurse and a medico-social worker) before allotment. This enables an external validation of the diagnoses as well as weeding out of non-cooperative families and prepares the families for the visit of the student. A follow-up visit after 2 weeks to 1 month should be scheduled for the students to assess compliance and reasons for non-compliance. The ethical issues and need for privacy during the family visits should also be discussed.
The maximum learning from these studies would be if these are integrated with clinical departments and are not run by departments of community medicine alone. This gives the impression that this study is not essential for clinical training.[9] In the initial years of training at the All India Institute of Medical Sciences, New Delhi, cases/families would be discussed jointly by clinical and community medicine faculty in the villages of Ballabgarh, Haryana. This was later stopped due to frequent disagreements on modes of management of the patient between them. The ethical and perspective conflict between a public health approach and a clinical approach to a disease has been described by us before.[16] A good understanding of both is needed for a doctor. As the number of students increase in Indian medical colleges, conducting individual family studies might pose a burden on departments because of lack of human resources as well as availability of a large community. In such cases, this could become a group exercise without diluting the approach. Community should also benefit from these exercises. While there will always be families for whom we can do little, there have been many examples in our experience where the students visit benefited the patients.
Making a Presentation of a Family Study
The end-point of a family study is a 15–30 minute presentation made to faculty members. Usually, the focus of presentation and questioning is on the method of data collection especially on clinical methods and dietary history.We recommend that the presentation should include only the diagnoses under each domain, their justification, web of interaction (preferably with animation) and finally a comprehensive management plan. A detailed written narrative should be submitted separately. The last slide should focus on what the student and the family benefited from the exercise. During examination, students should be given at least 2 hours to spend with the family and another 30-60 minutes to assimilate and organize their findings into the proposed framework. Evaluation of a family study should include equal weightage to the aspects of data collection, making diagnoses, web of interaction and management.
Conclusion
Family study/presentations are an important tool in medical education to enhance the understanding of students about social determinants of disease and multifactorial causation. We have proposed a framework and guidance to facilitate a more structured approach to enhance learning from a family study.
With Family Medicine being increasingly recognized as a separate specialty, it is time that family study in medical education is strengthened.
| 1. | Glynn M, Drake W. Hutchison's clinical methods: An integrated approach to clinical practice. 23rd ed. Philadelphia:Saunders; 2012. [Google Scholar] |
| 2. | Yin RK. Case study research: Design and methods. 5 th ed. California: S age Publications; 2014:5-6. [Google Scholar] |
| 3. | Thomas G. A typology for the case study in social science following a review of definition, discourse and structure. Q-ual Inq 2011;17:511-21. [Google Scholar] |
| 4. | Kishore J. Practical and viva-community medicine. New Delhi:Century Publications; 2010:1-48. [Google Scholar] |
| 5. | Tiwari P, Tiwari S. Mastering practicals: Community medicine. 1st ed. Philadelphia:Lippincott Williams and Wilkins; 2013. [Google Scholar] |
| 6. | Eddy LL, Doutrich D. Families and community public health nursing. In: Kaakinen JR, Gedaly-Duff V, Coehlo DP, Hanson SMH (eds). Family health care nursing: Theory, practice, and research. 4th ed. Philadelphia:FA Davis & Company; 2010:470-89. [Google Scholar] |
| 7. | Wright LM, Leahey M. Nurses and families: A guide to family assessment and intervention. 5th ed. Philadelphia:FA Davis & Company; 2009. [Google Scholar] |
| 8. | Commission on social determinants of health. A conceptual framework for action on the social determinants of health: Discussion paper for the Commission on Social Determinants of Health. Geneva, April 2007. [Google Scholar] |
| 9. | Meleney H, Mortara F. Medical-social family studies in medical education. J Med Educ 1952;27:19-23. [Google Scholar] |
| 10. | Bhore J. Report of The Health Survey and Development Committee. Vol 1. 158-75. Available at www.nhp.gov.in/directory-services-and-regulations/committees-and-commissions/bhore-committee1946 (accessed on 7 Jul 2015). [Google Scholar] |
| 11. | Hopp JW, Gerken CM. Making an educational diagnosis to improve patient education. Respir Care 1983;28:1456-61. [Google Scholar] |
| 12. | Phillips J, Simmonds L. Using fishbone analysis to investigate problems. Nurs Times 2013;109:18-20. [Google Scholar] |
| 13. | Hewitt-Taylor J. Identifying, analysing and solving problems in practice. Nurs Stand 2012;26:35-41. [Google Scholar] |
| 14. | Snowdon W, Schultz J, Swinburn B. Problem and solution trees: A practical approach for identifying potential interventions to improve population nutrition. Health Promot Int 2008;23:345-53. [Google Scholar] |
| 15. | World Health Organization. Prioritizing areas for action in the field of population-based prevention of childhood obesity: A set of tools for member states to determine and identify priority areas for action. Geneva:WHO; 2012. [Google Scholar] |
| 16. | Krishnan A, Kapoor SK, Pandav CS. Clinical medicine and public health: Rivals or partners? Natl Med J India 2014;27:99-101. [Google Scholar] |
Fulltext Views
6,534
PDF downloads
2,054




