Translate this page into:
Competency-based postgraduate training: Mentoring and monitoring using entrustable professional activities with descriptive rubrics for objectivity— A step beyond Dreyfus
Correspondence to ARCHANA ARETI; archanaareti@gmail.com
[To cite: Ravishankar M, Areti A, Hemanth Kumar VR, Sivashanmugam T, Rani P, Ananthakrishnan N. Competency-based postgraduate training: Mentoring and monitoring using entrustable professional activities with descriptive rubrics for objectivity—A step beyond Dreyfus. Natl Med J India 2023;36:176–81. DOI: 25259/NMJI_860_2021]
Abstract
Background
At Sri Balaji Vidyapeeth, a competency-based learning and training (CoBaLT©) model for postgraduate (PG) curriculum, within the regulatory norms, was implemented in 2016 after adequate faculty development programmes. This focused on well-defined outcomes.
Methods
A review of the outcomes was undertaken in 2018 as part of internal quality assurance receiving feedback from all stakeholders, viz. students, alumni and faculty. Recent publications were also reviewed. A major problem identified was lack of clarity in definition of levels leading to subjectivity in assessment while grading. It was also noted that the process needed to be aligned with the programme outcomes. Further refinements were, therefore, made to align and objectivize formative assessment using entrustable professional activities (EPA) with the aid of descriptive rubrics of sub-competencies and milestones. Addition of detailed rubrics for objectivity takes assessment a step beyond the Dreyfus model, aligning overall to the programme outcomes.
Results
Achievement of appropriate grades in EPAs by individual candidates ensures entrustability in professional activities by the time of completion of the PG programme. The modification was found more transparent and objective with reference to grading by the teachers and more conducive to reflections by the residents on their performance and how to improve it.
Conclusions
The use of descriptive rubrics along with EPAs brings transparency and plays a key role as an objective assessment tool, which can lend direction to individual resident learning and entrustability. This is an important component of outcome-based education.
INTRODUCTION
The National Medical Commission (NMC) published the revised version of the postgraduate curricula on their website in 2019.1 It is an improvement on the 2000 version and describes competencies in three domains (knowledge, skill and attitude). In 2021 the NMC posted a draft of the Postgraduate Medical Education Regulations 2021,2 which outlines in detail the format to be followed by medical universities for competency-based curriculum development.
However, at Sri Balaji Vidyapeeth (SBV), a competency-based model for postgraduate curriculum was initiated in 2013 and implemented in 2016 within the regulatory norms. The programme was called competency-based learning and training for postgraduates (CoBaLT©).* This model has been copyrighted and published enumerating the steps of implementation and the prerequisites.3 The most important problem in competency-based training was the lack of description of appropriate assessment tools as well as alignment of the assessment process to the curricular delivery.4 There was also a lack of understanding and training of faculty for the process, which added to the difficulty.5 While summative evaluation is entirely in regulatory hands, a lot can be done by universities and the institutions to have a robust system of formative assessment and monitoring, to ensure that residents attain a high standard of knowledge, skill and attitude.6 In this article, we explain the process undertaken by SBV to align and objectivize formative assessment with entrustable professional activities (EPA) with the aid of descriptive rubrics of milestone description.
REVIEW
A complete review of the CoBaLT© model was undertaken two years after implementation, in 2018, as part of internal quality assurance receiving feedback from the stakeholders namely, alumni, current residents in the specialty and faculty. The available literature published in the past 5 years formed a part of the review for introducing modifications.7–11
The main observation, from the SBV curriculum, was that the grading of EPA milestones based only on the Dreyfus model was entirely dependent on observations by the faculty in the workplace and grading tended to be highly subjective with variation between different faculty with no obvious justification. Besides, it took into account only skill performance without assessment of background knowledge required for exhibiting the skills and varying levels of difficulty for the same procedural skills. For entrustment decision, i.e. transfer of trust to the resident for performing the task, various trustee factors which include capability, integrity, reliability, humility and agency must also be considered.4,11 These factors were not clearly defined for documenting improvement in attitude. The milestone project of the Accreditation Council for Graduate Medical Education (ACGME)9 gave a detailed description of various levels of progression in sub-competency but was not found suitable for correlation with the EPA-based formative assessment. The other observations were that the EPA statements were not clear enough for certification of sustained competence and were not reflective of the programme outcomes (POs).
Refinements to the CoBaLT© programme
The major task was to identify specialty-specific criteria for progression in sub-competencies as milestones, such that the resident’s progression can be monitored objectively. These milestones were not time-based but gave a description using rubrics to assess progression over five levels. It is possible that some residents might reach a higher level in a shorter time compared to others. The milestones are linked to formative assessment to give feedback regarding the resident’s progression. The faculty and the programme coordinators worked jointly at least for an hour every day for about a month to complete the task. Every level had multiple nodes, and progression in each of them was considered. A sample milestone description, of one sub-competency each in knowledge and procedural skills, is shown in Tables I and II, respectively. After completing the milestone description, it was discussed among the entire faculty and relevant modifications were made as considered necessary. A check was carried out to ensure that the syllabus was covered in entirety by these descriptions.
| Milestone level 1 | Milestone level 2 | Milestone level 3 | Milestone level 4 | Milestone level 5 |
|---|---|---|---|---|
| Acquires knowledge about the basic airway anatomy. |
In addition to milestone level 1, acquires knowledge about assessment of anticipated difficult airway in adults. |
In addition to milestone level 2, acquires knowledge of difficult airway management— DAS guidelines. |
In addition to milestone level 3, acquires knowledge of management of compromised airways— due to trauma, obstruction or intubation failure. |
Acquires knowledge about recent advances related to airway management. |
| Acquires knowledge about basic assessment of normal airway in adults. |
Comprehends adequately to teach others. |
|||
| Acquires knowledge about differences of paediatric and neonatal airway and assessment. |
Acquires knowledge of airway changes in pregnancy. |
|||
| Acquires knowledge about the basic equipment related to the normal airway management. |
||||
| Acquires knowledge of lung isolation techniques, fibreoptic assessment of position. |
||||
| Acquires knowledge about airway anaesthesia, nasotracheal intubation, video laryngoscopy. |
||||
| Acquires knowledge about positioning and pre- oxygenation. |
Acquires knowledge about the equipment related to the difficult airway management. |
|||
| Acquires knowledge about the risk of aspiration and implication of full stomach. |
Acquires knowledge regarding blunting of haemodynamic stress response during airway manipulation. |
|||
| Acquires knowledge for intubation and extubation of a normal airway. |
||||
| Acquires knowledge about commonly used drugs for airway management. |
Acquires knowledge about preparation prior to airway management—position, supportive equipment and emergency drugs. |
Acquires knowledge about complications and management of airway manipulation. |
DAS difficult airway society
| Milestone level 1 | Milestone level 2 | Milestone level 3 | Milestone level 4 | Milestone level 5 |
|---|---|---|---|---|
| Performs airway assessment of normal airway. Appropriately prepares drugs, equipment and adjuncts for airway management. |
In addition to milestone level 1, performs assessment of anticipated difficult airway and formulates plans for securing airway. |
In addition to milestone level 2, performs basic airway management in obstetric patients. |
In addition to milestone level 3, performs airway interventions in difficult situations—trauma, obstruction, failure to intubate. |
Independently assesses and manages the airway for all clinical situations utilizing appropriate advanced airway techniques, including cricothyroidotomy. |
| Performs advanced airway management techniques, including awake intubations, video laryngoscopy and fibreoptic intubations. |
||||
| Positions patient for airway management; acquires correct use of oral and nasal airways; performs bag–valve–mask ventilation. |
Performs basic airway management in patients with normal airways, including endotracheal intubation, supraglottic airways. Recognizes and vocalizes need for assistance and/or equipment. |
Performance of lung isolation techniques. |
||
| Independently supervises and provides consultation to other members of the healthcare team for airway management. |
||||
| Appropriately manages tracheostomies. Performs basic paediatric airway management. |
||||
| Performs assessment, preparation and formulates plans for routine paediatric airway management. |
||||
| Performs paediatric airway management for difficult cases. |
||||
| Takes appropriate precautions when managing patients with full stomach. |
Identifies complications of airway interventions and takes appropriate measures to manage them. |
Redefining EPAs
The next step was to redefine the EPA statements that aligned with POs as well as to the milestone description in all six domains.
For example, airway management was written as two EPAs as shown below:
EPA3 Securing airway in patients with normal airway anatomy
EPA4 Securing airway in patients with difficult airway anatomy
Even though the EPAs are two, the required sub-competencies for knowledge and procedural skills are one, but the milestones that need to be reached vary. For example, fulfilment of EPA3 requires level 2 in MK5 and PC/PS2; whereas EPA4 requires level 4 in the same sub-competencies (Tables III and IV). The complete list of EPAs pertinent to the subject of Anaesthesiology is given in Annexure 1.
| EPA3. Securing airway in patients with normal airway anatomy | |||
| Description for the activity | The resident should be able assess and perform management of normal airway; this includes appropriate use of bag and mask, supraglottic, subglottic devices and airway gadgets. |
||
| Resident will be entrustable when these sub-competency milestone levels are attained |
Relevant domains of competency |
Sub-competencies within each domain |
Milestone level (L) in sub-competency |
| Medical knowledge | 5 | 5 – L2 | |
| Patient care/procedural skill (PC/PS) | 2 | 2 – L2 | |
| System-based practice (SBP) | 1, 2 | 1 – L3; 2 – L3 | |
| PBLI | 2 | 2 – L2 | |
| IPCS | 1, 2 | 1 – L2; 2 – L4 | |
| Professionalism | 3 | 1 – L3 | |
| Method of assessment | 1. Medical knowledge assessment will be done by the faculty either by direct interaction, written examination or e-portfolio. | ||
| 2 . PC/PS, SBP and PBLI assessment will be done by the faculty at the workplace and e-portfolio. | |||
| 3 . Communication skills and professionalism will be assessed by multisource feedback. | |||
| 4 . EPA assessment done during General Surgery and Ear, Nose and Throat postings. | |||
PBLI practice-based learning and improvement IPCS interpersonal and communication skills
| EPA4. Securing airway in patients with difficult airway | |||
| Description for the activity | The resident should be able to assess and perform management of difficult airway; this includes appropriate use of bag and mask, supraglottic, subglottic devices (including surgical access) and airway gadgets. |
||
| Resident will be entrustable when these sub-competency milestone levels are attained |
Relevant domains of competency | Sub-competencies within each domain | Milestone level (L) in sub-competency |
| Medical knowledge | 5 | 5 – L4 | |
| Patient care/procedural skill (PC/PS) | 2 | 2 – L4 | |
| System-based practice (SBP) | 1, 2 | 1 – L3; 2 – L4 | |
| PBLI | 2 | 2 – L3 | |
| IPCS | 1, 2 | 1 – L4; 2 – L4 | |
| Professionalism | 3 | 1 – L3 | |
| Method of assessment | 1. Medical knowledge assessment will be done by the faculty either by direct interaction, written | ||
| examination or e-portfolio. | |||
| 2 . PC/PS, SBP and PBLI assessment will be done by the faculty at the workplace and e-portfolio. | |||
| 3 . Communication skills and professionalism will be assessed by multisource feedback. | |||
| 4 . Assessment done in Ear, Nose and Throat and Oromaxillofacial Surgery posting. | |||
PBLI practice-based learning and improvement IPCS interpersonal and communication skills
The above procedure allowed the faculty to evaluate residents and assign graded responsibility to them according to their level of knowledge to the procedural skill. The milestone description gave in detail the rubrics for assessment and introduced objectivity. It ensured that the faculty understood the interpretation of the grading system. Finally, a grade of entrustability was assigned, according to their proficiency in performing the skill. The Dreyfus and Dreyfus model12 was modified as follows for grading EPA:
Grade 1. Can observe and assist
Grade 2. Can perform with strict supervision
Grade 3. Can perform with loose supervision
Grade 4. Can perform independently
Grade 5. Expert, able to teach others.
This grading system considers both the milestone reached and workplace-based assessment (WBA) at the same time bringing objectivity into assessment.
DISCUSSION
At SBV, we developed specialty-specific curricula encompassing the NMC recommendations. The curricular document of Anaesthesiology has been copyrighted† and is taken as an example for detailed discussion. The salient features of this document include defining the programme educational objectives (PEOs) for the postgraduate programme as a whole; the POs based on the competencies to be practised by the specialist and programme-specific sub-competencies and their progression in the form of milestones in all domains. EPA statements have been refined as per the recommended norms using the continuous verb form and plural when the title includes a verb and an object.13
The compilation of the milestone description in five levels automatically leads to the formation of the required syllabus. This process allows the mentors to monitor progress in sub-competency milestone levels. Although NMC has described three domains of competencies,14 we have used the six-competency domain model (ACGME),15 viz. medical knowledge (MK), patient care/procedural skill (PC/PS), practice-based learning and improvement (PBLI), system-based practice (SBP), professionalism (P), and interpersonal and communication skills (IPCS). This gave better clarity and in-depth explanation. The sub-competencies and their milestone levels are mapped to EPAs that are specific to the individual postgraduate programmes. During this whole process, it was ensured that the syllabus prescribed by the NMC was fully incorporated into the curriculum. To make the programme more relevant, PEOs, POs and EPAs are mapped with each other (Annexure 2).
EPAs, which are activity-based, are used for formative assessment and graded. EPA assessment is based on WBA, multisource feedback (MSF) and an e-portfolio. Much emphasis is placed on monitoring the progress in acquisition of knowledge, skill and attitude through various appraisal forms and mentoring through the e-portfolios during the 3 years of residency.
Transparency in formative assessment.
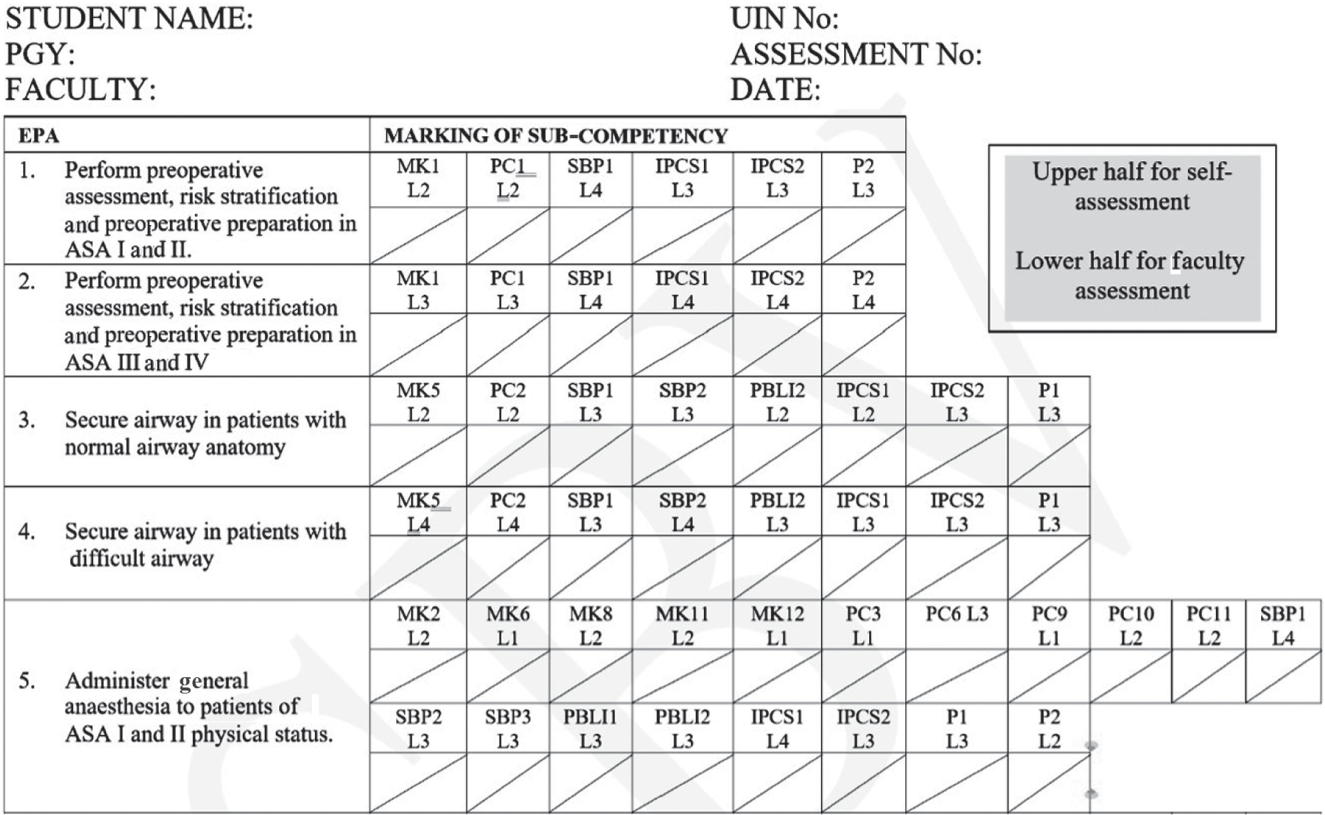
The residents are given a copy of the curriculum as soon as they enrol in residency. They undergo 2 days of orientation about the curriculum focusing on the EPA assessment form, which has the EPA titles and milestone levels to be achieved in each sub-competency. A sample of the form with five EPAs is shown in Fig. 1. The residents are apprised of the EPAs, milestone descriptions and how each level is assessed using these descriptions. They are then asked to self-assess at various milestone levels. This gives the residents an opportunity to understand the sub-competencies, milestones, the syllabus, and the EPAs and realize how they would be assessed. After spending a month in the department, faculty assess the residents on the same EPA assessment form and any difference in levels between self-assessment and the faculty assessment as well as the reason for the difference are discussed in detail. The milestone levels achieved are translated into EPA grades, based on which entrustability is assigned. On attaining the required milestone levels the EPA will be graded as 3. If the milestone level is not achieved in even one sub-competency, the EPA grade will be less. Further progression in EPA will be based on the proficiency exhibited by the resident. This ensures quality and safety in patient handling.
This formative assessment is done every quarter in year 1 and then every 6 months for the rest of the residency. Each faculty assessment is preceded by self-assessment by the resident, followed by a group discussion and giving feedback to the resident. This enables a robust formative assessment with feedback as well as lends direction to the residents on what is expected from them. Additional opportunities are created for them to improve on the EPA if found lacking. The grades to be obtained for each EPA for certification are prefixed by the curriculum committee. The EPA levels are certified with grades before the summative examination.
Recently, there is an increasing emphasis on programmatic assessment for competency-based medical education (CBME).16 After analysing ACGME outcomes, the milestone writing has been modified to include clear definitions of desired outcomes.17 It is suggested to develop a systems approach for programmatic assessment to accurately identify the progression to achieve the goal.17 In our model, we have written clear progressive milestone descriptions and linked them to the EPA grading for formative assessment, which uses multiple inputs over time from various sources. Further progress needs the acceptance of the model by the regulators and further deliberations at the national level. As such, our model fulfils the requirements for programmatic assessment.
The curriculum, however, cannot be covered in entirety by EPAs, which are activity based. Hence for these other areas, methods like the written, oral and clinical examinations are to be used to assess the knowledge, comprehension and interpretation, which make up the summative examination. Robust formative assessment in postgraduate medical education ensures practice readiness and quality control as independent specialists.
Conclusions
The CoBaLT© programme has been refined to make it more transparent, objective and aligned to the POs. Writing descriptive rubrics, for sub-competencies in the form of milestone levels linked to EPAs as regards the knowledge, the skill and the affective components, facilitates objectivity as all faculty are on the same page in terms of requirements for each EPA. The residents are familiarized with the content of the EPAs, the assessment process and the rubrics of milestones. Engaging in periodic self-assessment followed by faculty assessment drives the process with the grades being used for feedback, mentoring and monitoring. Students learn in confidence about their deficiencies and if required are given additional training inputs to reach the desired goals. A candidate’s achievement of appropriate grade, as decided by the curriculum committee, ensures entrustability by the completion of the postgraduate programme.
Conflicts of interest
None declared
References
- PG Curricula, NMC. Available at www.nmc.org.in/information-desk/for-colleges/pg-curricula-2/ (accessed on 29 Oct 2021)
- [Google Scholar]
- The Postgraduate Medical Education Regulations. 2021. Available at www.nmc.org.in/MCIRest/open/getDocument?path=/ Documents/Public/Portal/LatestNews/Draft%20PGME%20Regulation%20 Octoberr%202021.pdf (accessed on 29 Oct 2021)
- [Google Scholar]
- Competency-based learning and training for medical postgraduates within regulatory guidelines in India: The SBV Competency-Based Learning and Training Model©. Natl Med J India. 2019;32:365-8.
- [CrossRef] [PubMed] [Google Scholar]
- Competency-based medical education, entrustment and assessment. Indian Pediatr. 2015;52:413-20.
- [CrossRef] [PubMed] [Google Scholar]
- Competency-based medical education: An overview and application in pharmacology. Indian J Pharmacol. 2016;48(Suppl 1):S5-S9.
- [CrossRef] [PubMed] [Google Scholar]
- The role of assessment in competency-based medical education. Med Teach. 2010;32:676-82.
- [CrossRef] [PubMed] [Google Scholar]
- Competency-based curriculum. 2016. International Bureau of Education. published online May 20. Available at www.ibe.unesco.org/en/glossary-curriculum-terminology/c/competency-based-curriculum (accessed on 23 Dec 2020)
- [Google Scholar]
- HSC Faculty Development. Available at www.hsc.wvu.edu/faculty-development/assessment-materials/developing-a-competency-based-curriculum/ (accessed on 29 Oct 2021)
- [Google Scholar]
- Milestones by specialty. Available at https://acgme.org/what-we-do/accreditation/milestones/milestones-by-specialty/ (accessed on 29 Oct 2021)
- [Google Scholar]
- Perspectives on designing the competence based curriculum. Procedia-Soc Behav Sci. 2015;180:972-7.
- [CrossRef] [Google Scholar]
- The ingredients of a rich entrustment decision. Med Teach. 2020;42:1413-20.
- [CrossRef] [PubMed] [Google Scholar]
- The Dreyfus model of clinical problem-solving skills acquisition: A critical perspective. Med Educ Online. 2010;15
- [CrossRef] [PubMed] [Google Scholar]
- The recommended description of an entrustable professional activity: AMEE Guide No. 140. Med Teach. 2021;43:1106-14.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines for competency based postgraduate training programmes for MD in Anaesthesiology. Available at www.nmc.org.in/wp-content/uploads/2019/09/MD-Anesthesia.pdf (accessed on 29 Oct 2021)
- [Google Scholar]
- The ACGME outcome project: Retrospective and prospective. Med Teach. 2007;29:648-54.
- [CrossRef] [PubMed] [Google Scholar]
- Programmatic assessment: The secret sauce of effective CBME implementation. J Grad Med Educ. 2020;12:518-21.
- [CrossRef] [PubMed] [Google Scholar]
- The importance of competency-based programmatic assessment in graduate medical education. J Grad Med Educ. 2021;13(2 Suppl):113-19.
- [CrossRef] [PubMed] [Google Scholar]
Annexure 1
List of EPAs for Anaesthesia programme
| EPA1 | Assessing normal patients/patients with controlled comorbid illness preoperatively, risk stratifying and optimizing them before surgery |
| EPA2 | Assessing patients with comorbidity/patients with varying degrees of end-organ damage preoperatively, risk stratifying and optimizing them before surgery |
| EPA3 | Securing airway in patients with normal airway anatomy |
| EPA4 | Securing airway in patients with difficult airway |
| EPA5 | Administering general anaesthesia to patients of ASA I and II physical status |
| EPA6 | Administering general anaesthesia to patients of ASA III and IV physical status |
| EPA7 | Managing central neuraxial blockade in patients with ASA I and II physical status |
| EPA8 | Managing central neuraxial blockade in patients with ASA III and IV physical status |
| EPA9 | Performing peripheral nerve/fascial plane blocks |
| EPA10 | Providing monitored anaesthesia care |
| EPA11 | Securing peripheral and central vascular access including invasive arterial access |
| EPA12 | Managing acute pain conditions |
| EPA13 | Managing chronic pain conditions |
| EPA14 | Managing anaesthesia for cardiac surgery |
| EPA15 | Managing anaesthesia for thoracic surgery |
| EPA16 | Managing anaesthesia for neurosurgery |
| EPA17 | Managing anaesthesia in paediatric patients |
| EPA18 | Managing anaesthesia in obstetrics patients |
| EPA19 | Managing the critically ill patient |
| EPA20 | Conversant with pedagogic and andragogic methods of teaching and learning |
| EPA21 | Formulating a research protocol, performing literature search, data collection and analysis |
Annexure 2
List of programme educational objectives (PEOs)
| PEOs | are broad statements that describe what graduates are expected to attain within few years of completing their programme. These are based on the needs of the society as analysed and outlined by the regulatory body. |
| PEO1 | Specialist who can provide comprehensive care related to anaesthesiology, critical care and pain management |
| PEO2 | Be a leader and team member who understands the healthcare system and acts to provide safe patient care with accountability and responsibility |
| PEO3 | Communicator possessing adequate communication skills to convey required information in an appropriate manner in various healthcare settings |
| PEO4 | Lifelong learner keen on updating oneself regarding advancement in the healthcare field and able to perform the role of researcher and teacher |
| PEO5 | Professional who understands biomedical research and follows the principle of bioethics/ethics related to healthcare system |
List of programme outcomes (POs)
| PO1 | The resident should have knowledge of basic sciences as applied to anaesthesia. |
| PO2 | The resident should be a competent anaesthesiologist with required knowledge, procedural skills and attitude that will enable her/him to practise anaesthesiology independently in broad specialties with adequate knowledge and gain exposure in super-specialties. |
| PO3 | The resident should be up to date in the recent advances related to anaesthesiology. |
| PO4 | The resident should be familiar with the various teaching and training methods including simulators. |
| PO5 | The resident should develop appropriate organizational and communication skills, to function in a group as leader or member in operating room/intensive care unit. |
| PO6 | The resident should ensure patient safety and develop a systematic approach to management of medical errors. |
| PO7 | Identify the needs of patients and society and provide cost-effective care and advocacy. |
| PO8 | Communicate with stakeholders of the healthcare system. |
| PO9 | Develop and execute a protocol for a scientific research project, collect, analyse the data, and scientifically communicate to the others. |
| PO10 | Develop skills for self-directed learning and critical appraisal of the medical literature. |
| PO11 | The resident should understand the importance of informed consent and shared responsibility. |
Mapping of EPA, POs and PEOs together
| PEO1 | PEO2 and PEO3 | PEO4 | PEO5 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| PO1 | PO2 | PO3 | PO4 | PO5 | PO6 | PO7 | PO8 | PO9 | PO10 | PO11 | |
| EPA1 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||
| EPA2 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||
| EPA3 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||
| EPA4 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA5 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA6 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA7 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA8 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA9 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||
| EPA10 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA11 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA12 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA13 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA14 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||
| EPA15 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA16 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA17 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA18 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | |||
| EPA19 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||
| EPA20 | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ||||
| EPA21 | ✔ | ✔ | ✔ | ✔ | |||||||




