Translate this page into:
Consultation at surgical outpatient department and undergraduate medical education: A pilot study
To cite: Sinha MK, Taywade M, Singh PK. Consultation at surgical outpatient department and undergraduate medical education: A pilot study. Natl Med J India 2021;34:251.
Our undergraduate training produces general physicians, who are the backbone of rural health services. They provide care to a large section of society and manage different outpatient departments (OPDs). They need consultancy skills for these services. As independent consultancy is not allowed during the undergraduate training, we planned a pilot study to assess the results during the period of internship when students are authorized to practice under direct supervision. We also wanted to explore the feasibility of similar large-scale studies.
We divided the skill of OPD management into five areas of competency, namely history taking, examination, writing and planning, discussing management and global score and prepared an objective structured clinical examination-based checklist to find areas of weakness. After that, we conducted a single-centre cross-sectional pilot study on students who had completed at least 2 weeks of surgical internship posting. We conducted the study on cases that included sebaceous cyst, hydrocoele, acid peptic diseases, filarial lymphoedema, epididymo-orchitis and haemorrhoids. Each intern was evaluated twice on different cases, and every examination was scored by two independent experts. The scores in different competency domains were tabulated and analysed.
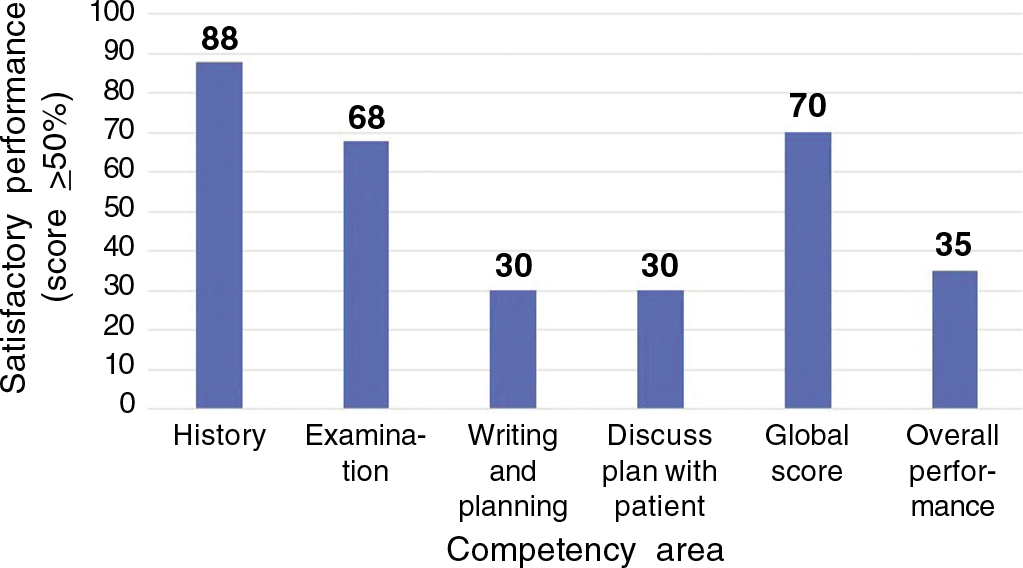
- The interns performed poorly in discussing the management plan and the overall score was 47%
We evaluated 11 interns on 22 cases. Two cases were excluded from analysis as these were not suitable for undergraduate evaluation. A total of 40 scored evaluation sheets were analysed. The average score in discussing the management plan was 24%, and this was badly affecting the overall score (Fig.1). The students performed badly even in simple cases for which adequate training was given in the undergraduate days. It was clear that due to difficulty in formulating and discussing the management plan, the consultancy skill was difficult for young doctors. Therefore, we decided to stop the pilot study.
The discussion of a management plan with patients and their attendants is a complex skill. It requires analysis and synthesis of knowledge, which is a higher-order cognitive function. It is more complicated than medical interviewing, which requires comprehension and application of knowledge. For a good discussion, the active participation of all stakeholders is essential. The practitioner should explain the disease and its possible course. They should discuss the possible interventions and their drawbacks. It is crucial to listen to the patient’s concerns and show appropriate empathy. Maguire et al. described these issues after analysing the consultation skills of 40 doctors, 4 to 6 years after the completion of their graduation. They concluded that the participant-doctors gave little importance to aetiology, future tests and prognosis in their discussion and were bad at providing information.1
Adult learning is a complex process and consists of four distinct stages. The learning is not complete till the individuals practice the skill themselves.2 In our case, we usually do not allow our undergraduate students to formulate the management plan and discuss it with patients during the OPD postings. This lack of opportunity deprives the students of the experience required for learning. Recently, Newcomb et al. tried to train undergraduate students on communication skills during the Covid-19 pandemic. They organized telecommunication sessions and used role-play for different clinical scenarios to expose the students to the art and science of clinical communication. The students found these sessions interactive and encouraging.3
For training on consultancy skills, we need the involvement of senior students in patient care beyond history taking, clinical examination and discussion of science at the clinics. We need to work on teaching modules that encourage students to learn communication on patient care at a place away from clinics. After these training modules, the students should participate in supervised clinical discussions with the patients. This will enable them to learn the art of rapport building resulting in better patient compliance and fewer workplace conflicts.
ACKNOWLEDGEMENT
We are grateful to Professor Manash Ranjan Sahoo for his contribution in the preparation of the OSCE checklist.
Conflicts of interest
None declared
References
- Consultation skills of young doctors: II--Most young doctors are bad at giving information. Br Med J (Clin Res Ed). 1986;292:1576-8.
- [CrossRef] [PubMed] [Google Scholar]
- Applying effective teaching and learning techniques to nephrology education. Clin Kidney J. 2016;9:755-62.
- [CrossRef] [PubMed] [Google Scholar]
- Building rapport and earning the surgical patient's trust in the era of social distancing: Teaching patient-centered communication during video conference encounters to medical students. J Surg Educ. 2021;78:336-41.
- [CrossRef] [PubMed] [Google Scholar]




