Translate this page into:
Elements of a successful hospital-based deceased donation programme in India: Zero to eighty-five in two years
2 Department of Critical Care Medicine, Lakeshore Hospital, Kochi, Kerala, India
3 Department of Hospital Administration, Lakeshore Hospital, Kochi, Kerala, India
Corresponding Author:
Philip G Thomas
Multi-Organ Transplant, Renaissance Transplant Institute, 1100E. Dove Avenue, Ste 201, McAllen, Texas 78504
India
p.thomas@dhr-rgv.com
| How to cite this article: Thomas PG, Aswathy C, Joshy G, Mathew J. Elements of a successful hospital-based deceased donation programme in India: Zero to eighty-five in two years. Natl Med J India 2018;31:201-205 |
Abstract
Background. Legislation has made organ donation after brain death (DBD) possible in India since 1994. However, no organs are donated in most parts of the country; the national organ donation rate is estimated at between 0.08 and 0.34 donors per million population—one of the lowest in the world.Methods. A 350-bedded private hospital in Kochi started its DBD programme in September 2013 with a structured approach based on counselling of family members of critically ill individuals. A counsellor trained to diagnose family dynamics, and recognize different stages of the grieving process, chose the right time, and the correct family member to whom the donation request could be made. Regular debriefing sessions of the core team consisting of a transplant surgeon, a transplant coordinator, an ICU counsellor and a unit administrator resulted in setting up systems that supported families of patients with catastrophic brain injury, and created an environment conducive to obtaining consent.
Results. A total of 85 organ donations took place in the first 24 months (September 2013 to September 2015) of instituting the programme.
Conclusion. It is possible with hospital-based teamwork and a structured approach to consistently elicit organ donation.
Introduction
Organ donation after death has remained sporadic in India, although the Transplantation of Human Organs Act has been in force since 1994, which recognized brain death (BD) and made organ donation after brain death (DBD) possible.
Modifications of the Transplant Act in 2012 mandated the state governments to create organ procurement organizations for retrieval, allocation and sharing of donated organs within the region. Recognized transplant centres were required to appoint transplant coordinators charged with the task of eliciting consent for DBD from the next-of-kin of the deceased. Hospitals that were not doing transplants, but with active trauma and neurology services, could apply for recognition as ‘non-transplant organ retrieval centres’ (NTORCs), and recover expenses for donor maintenance and the retrieval operation. However, this has not resulted in a major change, begging the question: What is necessary to break the impasse? More public education? Or focus on changing the culture within hospitals and among doctors?
The government of the highly literate southern Indian state of Kerala formed the Kerala Network of Organ Sharing (KNOS) in August 2012. Influential public figures and the press supported the government initiative, a film about heart donation became a box office hit, and a small uptick in organ donation occurred. Families of patients who were dying began volunteering to donate organs. However, most hospitals refused to participate in the programme.
Negative attitudes towards organ donation after death have become entrenched in hospitals and among doctors. Good medical management of individuals with catastrophic brain injuries is seen as additional (unremunerated) work for neurosurgeons. A programme to elicit organ donation is shunned by hospital administrators as it could, in theory, result in a bad reputation. Transplant coordinators are not welcome in neurology/ neurosurgery intensive care units (ICUs). Large government teaching hospitals, with busy neurological trauma services funded entirely by tax-payers, have had no donations in the 22 years since the Transplant Act was passed.
No hospital has a structured programme for deceased organ donation in India. Transplant centres focus on live donor transplants, leaving it to public education to somehow generate deceased donor organs, which they are happy to accept.
In the Kochi region, DBD was started by a non-governmental organization called Society for Organ Retrieval and Transplantation (SORT) in 2004. Starting in 2003, through 2013, our 350-bedded private hospital performed 523 live donor kidney transplants and 22 live donor liver transplants. One deceased donor liver and 3 kidneys were obtained via SORT during this time.
The in-house deceased donation programme was started in September 2013. It received recognition in 2015 at the state and national levels for the largest number of organs donated in one centre: 85 in the first 24 months. We describe how success was achieved, which may be useful to hospitals where DBD is seen as a daunting prospect.
Methods
The in-house deceased donation programme, launched in September 2013, can be described in 3 main categories:
- Administration and personnel. Mission statement, creation of jobs, description of duties and goals for every member of the team.
- Training
- Systems development.
Administration and personnel
Mission statement: Develop deceased donor organ transplantation.
- Transplant surgeon. A transplant surgeon experienced in deceased donor transplantation was recruited as the team leader. Responsibilities, apart from surgical duties, included building cooperative links within the hospital with the Chiefs of Critical Care Medicine (CCM), Neurosurgery, Neurology, other transplant units in the region, and KNOS.
- ICU counsellor. A counsellor was recruited to work alongside nurses in all ICUs. The ICU counsellor reported to the Chief of CCM, doing daily rounds with the CCM team, and liaisoned with the transplant coordinator when required.
- Transplant coordinator. Daily duties focused on potential recipients, their medical and social management, rank on KNOS website, post-transplant patient care, maintain records related to outcomes, and other tasks within the transplant unit connected with surgery and patient care.When called by CCM consultants or the ICU counsellor, the transplant coordinator went to the ICU to discuss organ donation with identified decision-makers among the next-of-kin of the deceased.
- Administrator. A transplant unit administrator was identified among the senior managers of the hospital to champion the initiative of deceased donation.
ICU counsellor
This was a unique job description in India. Training the ICU counsellor focused on 2 main areas:
- Recognition and management of the stages of grief
Elements integral to good counselling include gradually taking the family through the process of understanding a rapidly changing situation, explaining neurological diagnoses and the Glasgow Coma Scale in simple and culturally appropriate terms. While dealing with anger and denial are part of the skill set of social workers, the ability to recognize the stage of acceptance of death using verbal and non-verbal cues is critical.
- Identification of the ‘power person’ in the family
While studying relationships and dynamics within each family, the ICU counsellor had to quickly determine who the decision-maker was, and arrange for the person to be present whenever the neurology or CCM team needed to discuss the patient’s condition with the family. A designated counselling room was identified close to the neurology trauma ICUs, and posters of KNOS encouraging organ donation posted at appropriate places around the hospital.
Nursing education
No ICU counselling can happen without the active participation of nurses. The important task of educating nurses could not be based solely on didactic classroom lectures. To solve this problem, a day-long course of ‘Ethics Education’ was devised. These teaching sessions termed as ‘ICU counselling’ were structured according to the principles of adult education to be ‘needs based’ and interactive [Appendix 1]. A year after instituting the programme, a 22 item-questionnaire was circulated among all ICU nurses, nursing supervisors, and any other nurses who wished to participate in assessing the effectiveness of the training and attitudes to DBD. The responses were anonymous.
Eliciting organ donation
There is no easy formula for success in this complex task. However, it is amenable to a time-honoured tradition in warfare and sports: ‘debriefing’.
After every 5 attempts at eliciting organ donation, whether successful or not, members of the team would gather, usually over dinner, for a relaxed discussion of each case. The counsellor would take the lead, and go over each case describing events, the power person identified, attitudes encountered and dealt with, problems encountered that could (or could not) be fixed, and whatever happened that should not be repeated. These discussions led to developing the following systems: (i) workflow for catastrophic brain injury [Appendix 2]; (ii) workflow for brain death [Appendix 3]; (iii) workflow for donation request [Appendix 4].
Results
During the 24-month period from 1 September 2013 to 30 August 2015, 41 potential BD donors were identified. There were 34 men and 7 women with an age range of 14–71 years (mean age 37.3 years). All were considered suitable for organ donation. A request for donation was made in 38 cases, whose families were available for ICU counselling. For 3 potential donors, the family could not be contacted in time, and donation was not possible. Of the 38 donor families counselled, 32 gave consent (consent rate of 84%).
In the first year (2013–14) of the initiation of the programme, 44 organs were donated and in the second year (2014–15), 41 organs were donated. The organs donated included kidneys (53; from 1 child donor 2 kidneys were transplanted en bloc and are considered as 1 organ), liver (24), heart (6) and lung, pancreas and small bowel (1 each).
Feedback from nurses
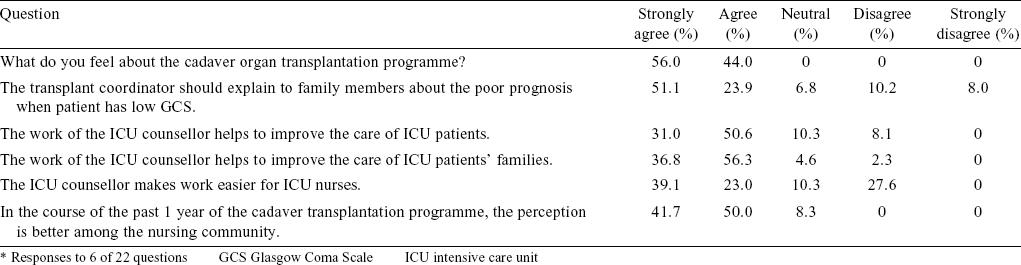
All the nurses supported the in-house DBD programme.There was no difference in the number of those who felt that the ICU counsellor should make the donation request compared with those who felt that the transplant coordinator should make the request; 82% felt that the ICU counsellor had positively impacted patient care in the ICU; 93% felt that the ICU counsellor had improved the care of ICU patients’ families, but only 62% felt that their work had been made easier by the addition of an ICU counsellor [Table - 1].
In fact, their workload increased, and the Nursing Administration had to recruit 2 nurses for all potential organ donors, if they became unstable, until brain death tests were done, and through till completion of the organ donation.
Feedback from families
Although no formal survey was done among donor families, they were felicitated at functions sponsored by non-governmental organizations, and at an annual function conducted by KNOS. Hospitals are expected to extend the invitation to donor families to attend these functions, and organize their transport to the state capital. Our donor families had the highest attendance compared with other transplant hospitals. All our donor families expressed satisfaction with the care received in the hospital, and the opportunity they got to positively impact others’ lives.
Discussion
It is universally experienced, and accepted, that organ donations after death do not happen unless an effort is made to make them happen. Worldwide, this effort has taken the form of innovative public education to create a culture of donation and change attitudes in society. Community participation is usually forthcoming and enthusiastic, recruiting celebrities for drives to make people sign donor cards, pledge their organs, join donor registries, etc. This is done with the expectation, but with no guarantee, that hospitals and medical professionals entrusted with the care of potential organ donors will do their part.
In India, with one of the lowest donation rates of 0.34 per million, attempts to increase organ donation after death have hitherto focused on public education and establishment of organ donor registries.[1],[3] About 86% of individuals are aware of organ donation.[3] Cornea donation has been successful for several decades, and over 98% of the population is aware that eyes can be donated after death.[2] The absence in India of cultural, regional or religious bias against eye donation has also been documented.[1],[2] It may not be unreasonable to assume that this is a good surrogate marker for social acceptability of organ donation after death.
The record of deceased organ donations has remained dismal in the 22 years since legislative sanction was obtained in India. Organ donation after death remains sporadic, and patients needing transplants who do not have a suitable live donor suffer the agony of having no options.
There is confusion about what should be done. Public education via the media is expensive, and has so far had minimal impact on initiating or increasing organ donations after death in India.
We have described the successful effort made by our hospital to improve organ donation. Based on these results, it may be postulated that organ donations are more likely to result from structured hospital programmes based on good ICU care and counselling of families of patients with catastrophic brain injuries, than from additional public education to promote deceased donation.
Few hospitals, even large transplant centres, have attempted a structured approach to eliciting organ donation within the institution, despite Army hospitals reporting some early success using ‘trained staff with requisite systems’.[5] There is either a reluctance to do so, or lack of information as to how to proceed. Transplant surgeons, physicians and hospital administrators who are happy to participate in community programmes to promote organ donation, hesitate to take an active role within their own institutions, preferring to stand aside and wait ineffectively for others to elicit organ donation. ‘Ethical considerations’ and ‘conflicts of interest’ are cited as reasons not to get involved in a process that would save the lives of their patients.
In a recent publication from Germany, it has been recognized that successful organ donation requires the expertise of ICU personnel in the medical management of the brain stem dead donor. This important aspect of management cannot be left to neurosurgeons, and indeed they must gradually withdraw from the care with a clear transition from ‘patient-centred care’ to ‘donation-centred care’ [Figure - 1].[6]
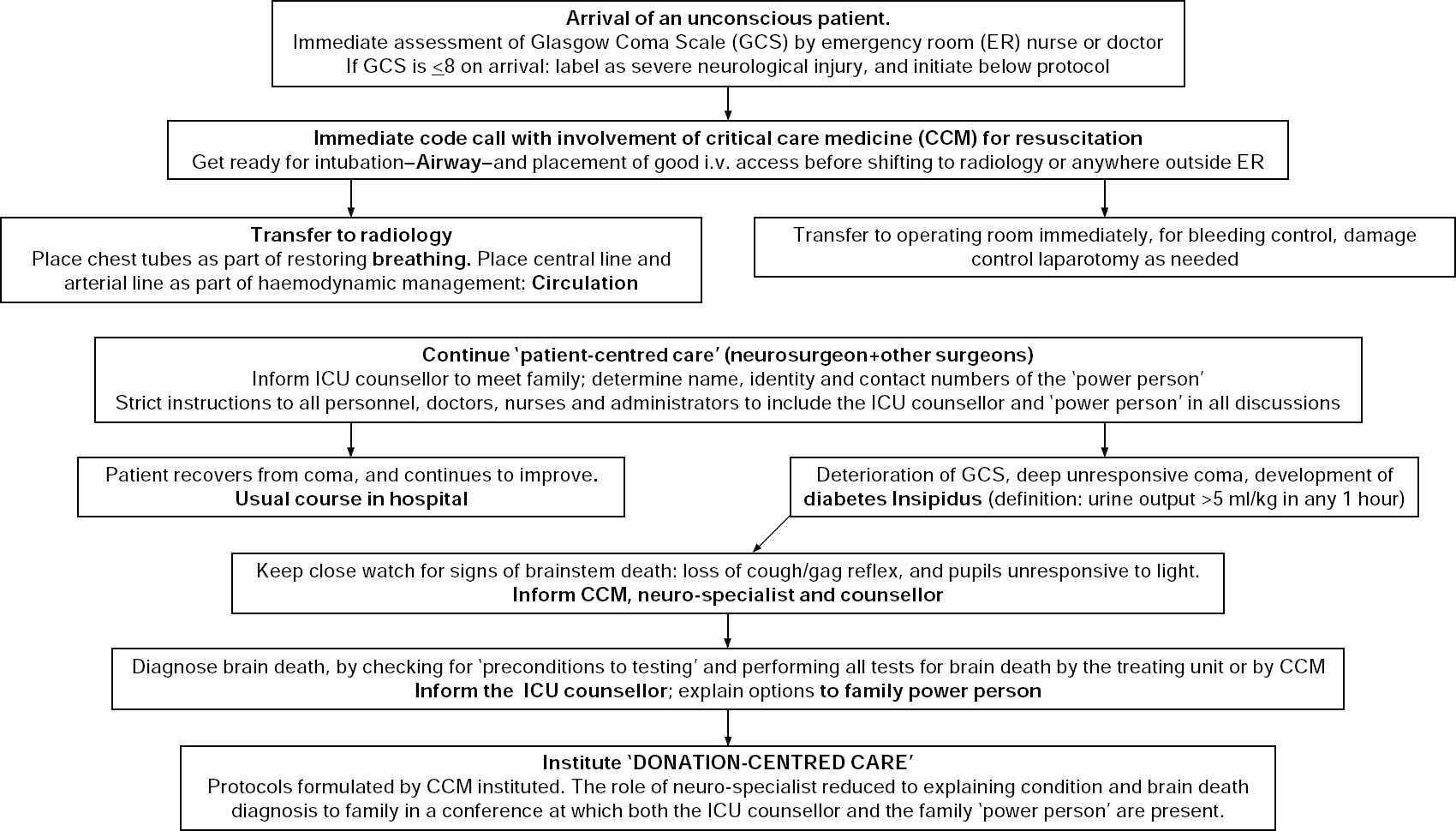 |
| Figure 1: Flow sheet for management of potential organ donors (incorporating the German model)[6] |
It is also recognized that involvement of transplant surgeons in the setting up of protocols for donation-centred care is essential, incorporating the best practices from the literature and also from transplant conferences to which ICU and neuro-specialists may not go. It is the duty of the hospital administration to ensure that protocols put in place by consensus by the different specialties are adhered to, as this is the only way to avoid the tragedy, with possible medicolegal consequences, of consent being given by the next-of-kin, but the organs being untransplantable due to poor management in the ICU.
The process outlined above provides a solution. Good counselling in the ICU is the key. Every patient admitted with catastrophic brain injury, defined as GCS <8, has an uncertain outcome and high cost, and families of these individuals need help as they stand and fret outside the ICU. If the empathetic help these individuals need is provided, they become future clients and even ambassadors of the hospital no matter what the outcome of care within the ICU. It is only when they are satisfied with everything that has been done to save their patient that families consent to organ donation. Organ donation thus becomes a metric of effective communication, ‘client’ satisfaction and an important safeguard against litigation. Participation of transplant professionals in instituting effective ICU counselling of families of potential organ donors is in the interest of hospital management, and the community at large.
Hospitals are where organ donations take place. We seek to prove that a hospital-based approach is key, changing the culture within a hospital is possible, and without this no amount of public education is likely to result in a successful organ donation programme.
Appendix 1
Nursing education is integral to Indian culture. Accordingly 4 modules were designed, each one centred around a skit playacted by previously rehearsed actors recruited from among the nurses. The venue was an auditorium with an elevated stage visible easily to the audience seated in a semi-circle. The stage was divided into 2 parts. On one side was a mock-up intensive care unit (ICU) cubicle with bed, patient mannequin, drip stand, infusion pumps, ventilator and monitors. At the centre was an area designated the ‘Counselling room’, with a sofa, comfortable chairs, a flower arrangement and Kerala Network for Organ Sharing (KNOS) posters adorning the walls.
A lectern was placed at the side of the stage for the facilitator to conduct discussions at the end of each skit. The skits were:
- Scenario #1: An ideal situation in which a patient with catastrophic brain injury is diagnosed as brain dead, the family is counselled well, accepts the diagnosis and goes on to donate organs.
- Scenario #2: To illustrate the difficulties resulting from lack of a structured approach to counselling of family members in the ICU, with different members of the team showing no understanding of the process. In particular, it depicts the difficulties that arise with premature request for organ donation, also called ‘prequest’, which is recognized as a risk factor for unsuccessful organ donation and also for confusion, anger and lack of good grief resolution in the ICU.
- Scenario #3: In this skit, the ICU room is not used. The main action is in the Counselling room. The premise is that a lot of the initial counselling has been done, and the counsellor has successfully managed the grief counselling required in a situation of catastrophic brain injury and brain death. However, a disruptive family member has seized control of the situation, forcing withdrawal of consent.
- Scenario #4: Here the approach to a ‘Medicolegal case’ is depicted. In this situation, police have to conduct an inquest, and an autopsy by a police surgeon is customary. This situation lends itself favourably to organ donation wherein the next-of-kin have the opportunity to retain and exercise their autonomy. It also gives the counsellor an opportunity to provide a number of services including counselling regarding the untimely death, education regarding the medicolegal procedure, as well as the additional service of facilitating completion of medicolegal obligations by supporting the family during interactions with the police.
Each skit has notes for the facilitator, and discussion points to be covered. At the end of each skit, the instructor would ask the audience: (i) what they thought of each skit; (ii) what went right; and (iii) what went wrong. Suggestions of how things could have gone better were elicited. This completed the individual module.
The atmosphere soon became one of fun and excitement. Many valuable suggestions were made which helped the ICU counsellor to work better subsequently, and perhaps more importantly, introduced the idea of counselling, and the counsellor to the entire nursing community removing any room for rumours as to what the agenda of the counsellor was.
Appendix 2
Workflow for catastrophic brain injury
- Casualty officer and nurses perform primary assessment, and initiate resuscitation on arrival.
- Immediate notification of anaesthesiology and critical care medicine if GCS<8, or hypotensive on arrival.
- Expert assessment of airway, breathing and fluid resuscitation immediately, focused assessment by sonography in trauma (FAST) examination for intra-abdominal bleeding, and if necessary immediate transfer from casualty to operating room.
- CT of head and neck after stabilization of airway and neck, and when considered haemodynamically safe.
- Neurosurgery decision regarding surgery or conservative management of the head injury.
- ICU counsellor interacts with the family to determine family dynamics, identify the ‘power person’, and ensure effective communication between caregivers inside the ICU, and the family members waiting outside.
Assistance with financial concerns, and medicolegal matters
All patients requiring assisted ventilation receive a central venous line and arterial line for monitoring. If GCS deteriorates, measures to prevent hypothermia, and the early detection and management of diabetes insipidus are instituted. Diabetes insipidus is suspected by ICU nursing staff if urine output goes over 5 ml/kg in any 1 hour. Immediate information to CCM and monitoring of electrolytes every 12 hours.
Appendix 3
Workflow for brain death
- When brain death (BD) is suspected, neurosurgeons are immediately informed.
- After ascertaining cranial nerve function, and when appropriate, neurosurgeons give permission for CCM to proceed with performing apnoea test.
- Positive first test: ICU counsellor is alerted to interact with the family, explain the situation, organize a family conference with doctors, making sure the decision-makers are present.
- Ascertaining the wishes of the next-of-kin as to further management:
- ICU counsellor to assess the needs of the family with respect to time required for understanding the information, and accepting the diagnosis.
- Grief counselling, assessment of stage of grief of main decision-makers in the family.
- When considered appropriate, information to transplant coordinator and unit administrator to make organ donation request.
- Continued support of family, assistance with documentation, certificates, funeral arrangements.
- Transplant coordinator to inform KNOS, document serial organ function tests, clinical condition, and ascertain interest in organs to be retrieved based on age, medical and social history, and condition of the patient. Documentation of blood type and completeness of infectious diseases screen. Blood samples to tissue antigen laboratory for screening cross-matches of waitlisted patients.
- Transplant coordinator to inform medical superintendent, and in conformity with legal procedure, organize the panel of 4 doctors who will confirm brain death. This is timed to follow 6 hours after the first set, done by in house doctors.
- After the expert panel gives the green signal to proceed, operating time fixed based on the organs to be retrieved, and the time needed for retrieval teams to arrive.
- In the operating room: Transplant coordinator to make sure documentation of organ anatomy, packaging, operation notes to accompany body of the deceased to the medicolegal autopsy.
- Liaison with donor family throughout the process of organ retrieval, and post-donation follow-up.
If consent is given for organ donation:
Appendix 4
Workflow for donation request
Gradually a pattern emerged:
- Acceptance: During the grieving process, identification of the stage of acceptance of death is critical.
- Request: The organ donation request could only be made after the first set of BD tests, including the apnoea test. If consent was obtained, a consultant neurologist from outside the hospital would be called in to verify the diagnosis, in conformity with the law. However, in cases where consent was not given, the family’s wishes regarding ‘Do not resuscitate’ (DNR) orders and comfort measures could be ascertained and instituted.
- Bargaining: Bargaining was seen to follow acceptance of BD diagnosis, to a varying degree, and tough bargainers in some families required a tough bargainer on the part of the hospital. The motivation for the ‘hospital bargainer’ was the possibility of saving lives of recipients waiting for organs. His main armamentarium was the published list of waiting patients maintained on the KNOS website. He was in reality working not for the hospital but for society, along with KNOS.
- Donor maintenance: Playing for time was critical to the success of counselling, and for a successful organ donation request. This required the cooperation of CCM and neurosurgery to maintain the donor medically so that organs did not deteriorate and donation become impossible when family members (finally) came back with a decision.
- Medicolegal cases: In medicolegal cases, the transplant coordinator would activate the ‘Green Channel’ provision to fast track medicolegal and inquest formalities including autopsy.
| 1. | Vania DK, Randall GE. Can evidence-based health policy from high-income countries be applied to lower-income countries: Considering barriers and facilitators to an organ donor registry in Mumbai, India. Health Res Pol-icy Syst2016;14:3-14 [Google Scholar] |
| 2. | Patil R, Ram Prasath E, Boratne A, Gupta SK, Datta SS. Status of eye donation awareness and its associated factors among adults in rural Pondicherry. J Clin Diagn Res 2015;9:LC01-4. [Google Scholar] |
| 3. | Balwani MR, Gumber MR, Shah PR, Kute VB, Patel HV, Engineer DP, et al. Attitude and awareness towards organ donation in western India. Ren Fail 2015;37:582-8. [Google Scholar] |
| 4. | Navin S, Shroff S, Niranjan S. Deceased organ donation in India. Organ donation and transplant resources. Chennai: Mohan Foundation. Available at www.mohanfoundation.org/organ-donation-transplant-resources/organ-donation-in-india.asp (accessed on 1 May 2017). [Google Scholar] |
| 5. | Seth AK, Nambiar P, Joshi A, Ramprasad R, Choubey R, Puri P, et al First prospective study on brain stem death and attitudes toward organ donation in India. Liver Transpl2009;15:1443-7. [Google Scholar] |
| 6. | Hahnenkamp K, Bohler K, Wolters H, Wiebe K, Schneider D, Schmidt HH. Organ- protective intensive care in organ donors. DtschArztebl Int2016; 113:552-8. (English translation available at www.ncbi.nlm.nih.gov/pmc/articles/PMC5015577/ (accessed on 1 May 2017). [Google Scholar] |
Fulltext Views
2,216
PDF downloads
692




