Translate this page into:
Knowledge, attitude and practice towards Ayurveda among patients attending cardiology and neurology clinics at a tertiary care institute in India
Correspondence to GAUTAM SHARMA; drgautamsharma12@gmail.com
[To cite: Sharma G, Sharma V, Mridula MK, Agrawal A, Ram A, Khuntia BK, et al. Knowledge, attitude and practice towards Ayurveda among patients attending cardiology and neurology clinics at a tertiary care institute in India. Natl Med J India 2023;36:145–9. DOI: 10.25259/NMJI_63_21]
Abstract
Background
Ayurveda, the Indian system of medicine, has been practised in India since ages. We evaluated the overall awareness regarding Ayurveda among patients attending two specialty clinics at a tertiary care institute.
Methods
We did a cross-sectional study on patients attending the cardiology and neurology clinics at a tertiary care hospital in India. We conducted this paper-based survey using a standardized, validated questionnaire. Statistical analysis was performed using STATA version 14.2.
Results
Three hundred and ninety-seven patients agreed to participate in the study. Their mean (SD) age was 45.65 (15.02) years. Among them 68.5% were men and 56.9% were from urban areas. Participants perceived that Ayurveda comprised herbal drugs (77.6%), metallic/herbo-mineral preparations (44.3%), Panchakarma therapy (22.2%) and personalized medicine (37.8%). Principal sources of information were TV promotional programmes (34.7%) and newspaper advertisements (13.9%). Nearly two-thirds (63%) of participants opined that Ayurveda is effective in chronic disorders. Although only 9.1% of participants reported the use of Ayurvedic medicines, 89.2% believed it would be beneficial if the All India Institute of Medical Sciences (AIIMS), New Delhi had Ayurveda services. Three-fourths (75.8%) of respondents were interested to participate in research studies integrating Ayurveda with modern medicine.
Conclusion
Imprecise knowledge and awareness towards Ayurveda appears to prevail in addition to the low practice among the patients surveyed. We found imprecise knowledge of Ayurvedic therapies and its low usage among patients attending specialized OPDs in a tertiary care hospital. The major source of information reported was promotional advertisements in the print and electronic media. Our survey shows a need for awareness programmes for general public at various levels.
INTRODUCTION
According to the WHO estimate, about three-quarters of the world’s population uses herbal or traditional medicine (TM) to treat various ailments.1 TM plays an important role in the medical system of China, Korea and Japan. Chinese TM accounts for around 40% of all healthcare delivered and it is used to treat approximately 200 million patients annually. Nearly 69% of the Korean population uses Traditional Korean Medicine and 60%–70% of modern doctors in Japan prescribe herbal medicines for their patients. These countries introduced the use of TM in their national healthcare systems and developed national policies.2 Among all hospitals in China, 90% have set up dedicated TM departments and 13.8% are specialized TM hospitals.3 On similar lines, the Government of India is also promoting the AYUSH systems of medicine. The term AYUSH is an acronym for five systems of medicine, namely, Ayurveda, Yoga, Unani, Siddha and Homoeopathy. In this scenario of medical pluralism, the level of awareness among patients regarding Ayurveda optimizes the success of the healthcare system.
Ayurveda has been practised in India since 1500 BC4 and its acceptance as an alternative medicine is growing all over the world. Ayurveda has a personalized approach in predictive, preventive and curative aspects of medicine.5 Plant-based formulations, Panchakarma therapy, dietary modifications and lifestyle changes have been used for thousands of years to maintain homoeostasis to improve the quality of life in chronic lifestyle disorders.6 Among chronic lifestyle disorders, coronary heart disease (CHD) has witnessed an alarming rise, thereby attaining the status of a global epidemic.7 India has witnessed a disturbing increase in the prevalence of CHD and cardiovascular mortality over the past two decades.8 Prevalence of CHD has increased from 1% to 9%–10% in the urban population and <1% to 4%–6% in the rural population over the past 60 years.7 Dyslipidaemia, smoking, diabetes, hypertension, abdominal obesity, psychosocial stress, unhealthy diet and physical inactivity are identified as risk factors for CHD in India by various case–control studies.7 Thus, steps must be taken to promote primordial, primary and secondary prevention of CHDs. This will prevent the occurrence of risk factors, early screening and control of risk factors and better management of acute and chronic cardiovascular events.
In India, patients often search for therapies that are alternative to conventional treatment such as Ayurveda, Siddha, Homoeopathy, Yoga, etc. for lifestyle disorders. The Centre for Integrative Medicine and Research (CIMR) has been established at AIIMS, Delhi, by the Ministry of AYUSH, Government of India with the aim of promoting an integrative approach to healthcare. The role of integrative medicine is still in its infancy in India,9,10 although patients routinely take Ayurvedic medicines along with modern medicines for their disease conditions, for example stem bark of Arjuna (Terminalia arjuna) is taken as cardiotonic by many patients visiting cardiology OPD at AIIMS, Delhi.
There are several research papers on the use of complementary and alternative medicine in patients of rheumatoid arthritis,11 infertility12 and inflammatory bowel disorder13 in different parts of the world. However, there is a scarcity of data regarding the use of Ayurvedic medicine in patients suffering from cardiovascular or neurological disorders along with modern medicine in India. To the best of our knowledge, there are no such surveys reporting the knowledge, attitude and practice of Ayurveda among patients attending cardiology and neurology OPD of a tertiary care hospital in India.
We did this study to investigate the level of knowledge and attitude of patients about Ayurveda and to generate data regarding the concomitant use of Ayurveda as therapy.
METHODS
Study design and setting
This was a cross-sectional, questionnaire-based study done among patients attending cardiology and neurology clinic of a tertiary care hospital in India during November 2018 and February 2019. The participants were surveyed in the order of appearance at the clinics.
Sample size
Considering that approximately 500 patients visit the specialty OPDs on an average day, patient population for 3 months was calculated (n=45 000). With confidence interval of 95% and margin of error as 5%, a sample size of 381 was calculated.
Eligibility criteria
Patients attending cardio-neurology OPD, both genders and age above 18 years were eligible. Subjects who could understand Hindi/English language and gave written informed consent were included.
Data collection tool
The survey was conducted using a standardized paper-based questionnaire, developed and validated by the multidisciplinary team of CIMR. The questionnaire was designed by researchers after literature review and its content validity was confirmed by 15 Ayurveda experts from different Ayurveda institutes all over India. The first part of the questionnaire enquired about demographic characteristics (age, gender, religion, area of residence and socioeconomic status) and the second part contained 28 questions about the knowledge, attitude and practice of the Ayurveda system of medicine. The knowledge domain questions assessed participant’s knowledge of Ayurveda with its treatment modalities, efficacy of Ayurveda in acute/chronic disorders and associated side-effects. The attitude domain questions assessed the participant’s approach for Ayurveda in chronic conditions, related safety issues and concomitant usage with modern medicines. It was also asked whether the participants would be interested in Ayurveda/integrated research trials and OPD/inpatient services at the tertiary care centre. Practice domain questions queried regarding the current and previous use of Ayurvedic medicines, source of prescription and improvements achieved. There were six other close-ended questions related to sources of information about Ayurveda and disease conditions, for which Ayurveda was preferred by the participant. Of 30 questions, 18 had options as Yes/No/Don’t know. There were six open-ended questions, in which the participants were asked about advantages of Ayurveda, name of the medicines used and the reasons of opting for Ayurveda. The third part of the questionnaire had two questions regarding accessibility of Ayurveda healthcare services. Data were collected by trained staff and healthcare professionals of CIMR.
Ethics committee approval
The permission of the Institutional Ethics Committee was taken before the initiation of the study. Participants were free to withdraw at any time. Written informed consent was obtained before start of the study. Anonymity and confidentiality of the data was maintained while collecting, analysing and reporting data.
Statistical analysis
Data were analysed using STATA version 14.2. All continuous variables were expressed as mean (SD) and categorical variables were expressed as percentages. Chi-square test was used to compare categorical variables. The correlation between scores of different domains was determined by Pearson product moment correlation coefficient. While analysing the data, a value of p<0.05 was considered to be statistically significant.
RESULTS
A total of 409 patients were screened, of which 397 gave consent for the study. The mean (SD) age of the participants was 45.7 (15.02) years. Of 397 participants, 68.5% were men and 56.9% belonged to urban areas. Participants represented upper (2.0%), upper middle (25.7%), lower middle (30.0%), upper lower class (35.5%) and lower (6.8%) as per Kuppuswamy socioeconomic scale 2017 (Table I).
| Variable | Ayurveda user n(%) |
Ayurveda non-user n(%) |
Total, n(%) |
|---|---|---|---|
| Total | 36 (9.1) | 361 (90.9) | 397 (100) |
| Mean (SD) age (in years) |
49.9 (16.94) | 45.2 (14.78) | 45.7 (15.02) |
| Gender | |||
| Men | 21 (58.3) | 251 (69.5) | 272 (68.5) |
| Women | 15 (41.7) | 110 (30.5) | 125 (31.5) |
| Residence | |||
| Urban | 20 (55.6) | 206 (57.1) | 226 (56.9) |
| Rural | 16 (44.4) | 155 (42.9) | 171 (43.1) |
| Religion | |||
| Hindu | 27 (75.0) | 306 (84.8) | 333 (83.9) |
| Muslim | 6 (16.7) | 42 (11.6) | 48 (12.1) |
| Sikh | 2 (5.6) | 4 (1.1) | 6 (1.5) |
| Jain | 1 (2.7) | 3 (0.8) | 4 (1.0) |
| Christian 0 | 6 (1.7) | 6 (1.5) | |
| Marital status | |||
| Married | 33 (91.7) | 276 (76.5) | 309 (77.8) |
| Single | 3 (8.3) | 85 (23.5) | 88 (22.2) |
| Family type | |||
| Nuclear | 17 (47.2) | 165 (45.7) | 182 (45.8) |
| Joint | 19 (52.8) | 196 (54.3) | 215 (54.2) |
| Socioeconomic status | |||
| Upper 0 | 8 (2.2) | 8 (2.0) | |
| Upper middle | 10 (27.8) | 92 (25.5) | 102 (25.7) |
| Lower middle | 10 (27.8) | 109 (30.2) | 119 (30.0) |
| Upper lower | 12 (33.3) | 129 (35.7) | 141 (35.5) |
| Lower | 4 (11.1) | 23 (6.4) | 27 (6.8) |
Among the surveyed patients, 70% were not aware about the term ‘AYUSH’ or had heard the acronym. Some participants erroneously correlated the term ‘AYUSH’ with ‘Ayushman Bharat Scheme’ launched by the Government of India, related to providing free medical care for low-income families/poor people.
Participants correlated Ayurveda with herbal drugs (77.6%), metallic/herbo-mineral preparations (44.3%), Panchakarma therapy (22.2%) and diet and seasonal regimens (43.8%). Nearly 54.7% of patients were aware about the effectiveness of Ayurveda in treating acute disorders such as fever and 63% believed that it was effective in treating chronic disorders.
Nearly 65.7% of participants believed that Ayurvedic medicine should be taken only after consultation with an Ayurveda physician. Concomitant use of Ayurvedic medicines along with modern medicines was supported by 40.1% of participants. Nearly 58.9% of responders believed that Ayurvedic medicines have no side-effects. Around 89.2% opined that it will be beneficial for them if AIIMS, Delhi had Ayurveda OPD and inpatient services. Around 75.8% of patients were interested in participating in integrative research studies at AIIMS (Table II).
| Question | Yes, n (%) | No, n(%) | Don’t know, n(%) | |
|---|---|---|---|---|
| 1. | What does Ayurveda therapy include? | |||
| Herbal drugs | 308 (77.6) | 14 (3.5) | 75 (18.9) | |
| Metallic/herbomineral preparation | 176 (44.3) | 43 (10.8) | 178 (44.8) | |
| Diet and lifestyle recommendations | 231 (58.2) | 32 (8.1) | 134 (33.8) | |
| Panchakarma therapy | 88 (22.2) | 70 (17.6) | 239 (60.2) | |
| Daily and seasonal regimen | 174 (43.8) | 35 (8.8) | 188 (47.4) | |
| Individualized treatment for patients | 150 (37.8) | 35 (8.8) | 212 (53.4) | |
| 2. | Ayurveda is effective in treating: | |||
| Acute disorder such as fever | 217 (54.7) | 60 (15.1) | 120 (30.2) | |
| Chronic disorders such as hypertension, diabetes, obesity, joint pain | 250 (63.0) | 23 (5.8) | 124 (31.2) | |
| 3. | Is it safe to take Ayurvedic medicine without consulting a physician? | 95 (23.9) | 261 (65.7) | 41 (10.3) |
| 4. | Can Ayurvedic medicine be taken with modern medicine? | 159 (40.1) | 118 (29.7) | 120 (30.2) |
| 5. | Does Ayurvedic medicine have side-effects? | 54 (13.6) | 234 (58.9) | 109 (27.5) |
| 6. | Would you participate in integrative research studies? | 301 (75.8) | 32 (8.1) | 64 (16.1) |
| 7. | Would it be beneficial if AIIMS Delhi had Ayurveda outpatient and inpatient facilities? | 354 (89.2) | 9 (2.3) | 34 (8.6) |
Question Yes, n (%) No, n (%) Don’t know, n (%)
The major source of information for the participants was TV promotional programmes (34.7%), newspaper advertisements (13.9%) and family (12.1%; Fig. 1). Around 21.7% of participants reported that they had read some literature related to Ayurveda. Nearly 84.9% of participants were aware that faulty diet and lifestyle play a role in the manifestation of diseases.
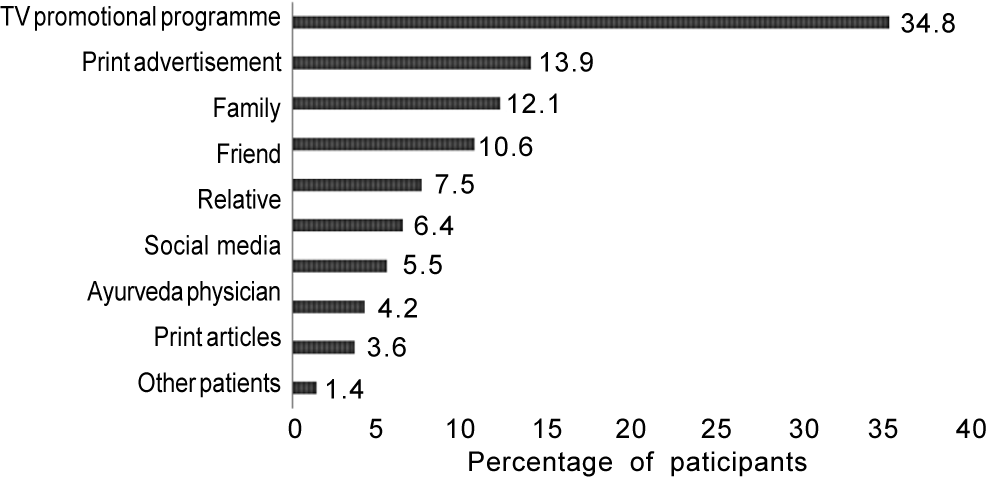
- Sources of information related to Ayurveda
A positive correlation was observed among the knowledge and attitude domain (r=0.43). Socioeconomic status of the participants was significantly associated (p<0.001) with knowledge of Ayurveda. Participants belonging to higher socioeconomic classes had proportionately higher level of knowledge of Ayurveda than those from the lower socioeconomic classes (Fig. 2).
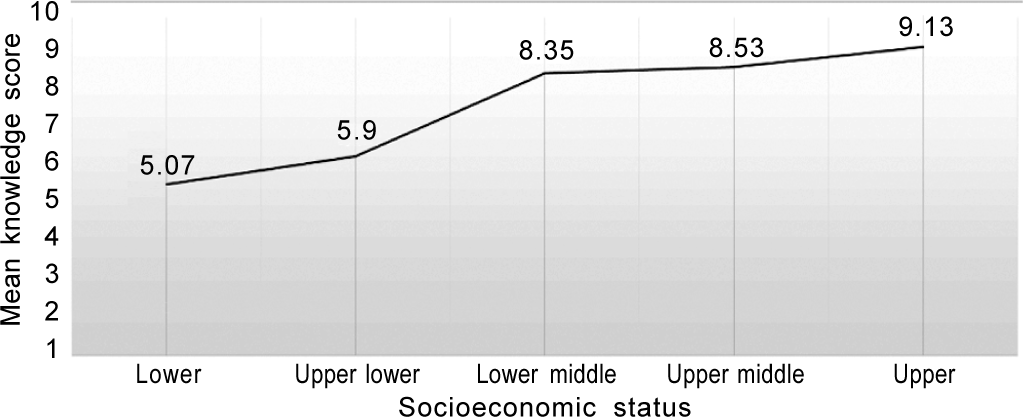
- Association between socioeconomic status and level of knowledge
Nearly 9.1% of participants reported the current use of Ayurvedic medicines, among this 12.6% and 4.2% reported Ayurvedic medicines usage for cardiac and stroke rehabilitation, respectively (Fig. 3). However, 46.3% said they or their family members had used Ayurvedic medicines in the past. Among Ayurvedic medicine users, 50% had consulted an Ayurvedic physician and 5.6% had taken advice of an Ayurvedic pharmacist or non-registered practitioner. Around 30.6% of patients were taking Ayurvedic medicine for more than a year. Around 75% of current users reported that they had not experienced any side-effect of Ayurvedic medicines. When asked about improvement, the mean (SD) score was 5.45 (2.77) on a scale of 0–10, where ‘0’ denoted no improvement and ‘10’ maximum improvement/complete relief of symptoms (Table III).
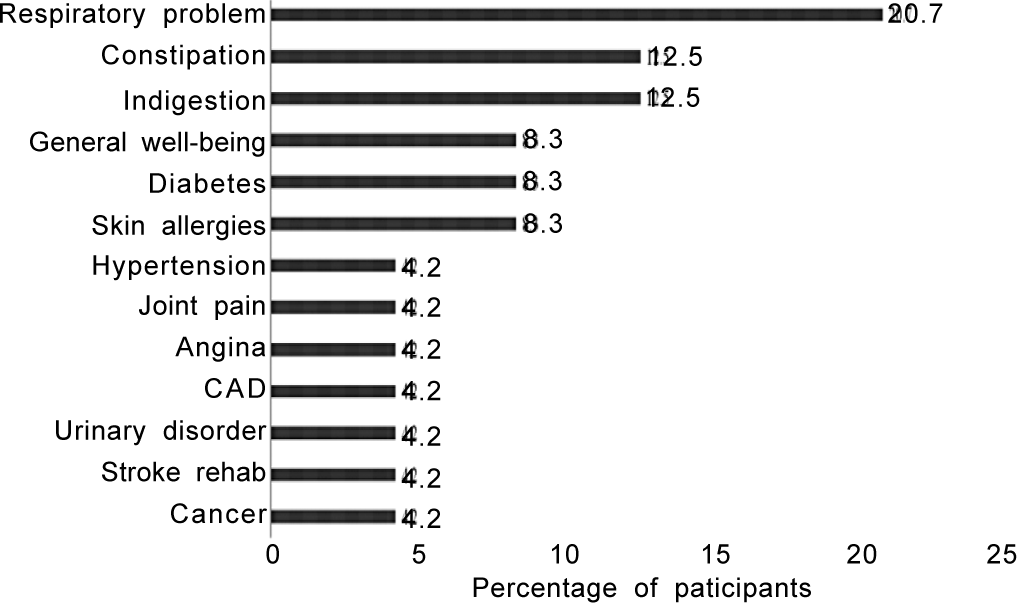
- Distribution of patients taking Ayurvedic medicine for specific diseases CAD coronary artery disease
| Question | Yes, n (%) | No, n(%) | Don’t know, n(%) | |
|---|---|---|---|---|
| 1. | Are you currently taking Ayurvedic medicine? | 36 (9.1) | 361 (90.9) | 0 |
| 2. | Have you/your family taken Ayurvedic medicine in the past? | 184 (46.3) | 213 (53.7) | 0 |
| 3. | Have you experienced any side-effect of Ayurvedic medicine? | 2 (5.6) | 27 (75.0) | 7 (19.4) |
| 4. | Whether Ayurveda treatment has improved your general well-being? | 22 (61.1) | 9 (25.0) | 5 (13.9) |
Around 30.6% of Ayurvedic medicine users had communicated to the treating modern medicine physician regarding their use of Ayurvedic medicines, whereas 69.9% of participants did not reveal their use of Ayurvedic medicine to the treating modern doctor. Upon asking further, 40% said that the doctor did not enquire about it, 16% reported that they did not intend to disclose it and 4% said that they did not disclose it due to the fear that doctor will not treat them properly or they may ask to stop the Ayurvedic medicine. Around 41.7% of participants believed that their treating physician would support the use of Ayurvedic medicine.
Regarding accessibility to Ayurvedic physician and clinical settings, participants reported that Ayurvedic physicians (37%), dispensaries (30%) and hospital/institutions (15%) were available within 5 km from their residence.
DISCUSSION
We investigated the KAP of patients with cardiac and neurological disorders, regarding Ayurveda. Overall, participants had moderate level of knowledge of Ayurveda (50.8%) and moderate attitude score (53.1%). Notably, socioeconomic status of the participants was significantly associated with their knowledge and attitude towards Ayurveda. Lower socioeconomic class usually confronts with issues such as health-related informational disparity, lack of perception of need and fear of additional expenses, which leads to low awareness regarding health-related awareness. However, gender, family type, residential area and religion did not significantly influence the knowledge or attitude.
Ayurveda adopts personalized approach in diagnosing disease and while prescribing lifestyle modification according to the Prakriti (individual constitution), age and geographical location and season, etc. Moreover, selection of treatment varies according to the stages of diseases based on the stages and patterns of disease progression.14 However, most participants correlated Ayurveda with herbal drugs (77.6%). This prevalent perception may be due to the finding that majority of the responders derived information regarding Ayurveda either from TV promotional programmes or newspaper advertisements. These advertisements usually portray herbal products as Ayurveda, devoid of any adverse effects and try to influence perception of the audience. These factors need to be addressed in order to enhance the knowledge of Ayurveda. The Ministry of AYUSH, Government of India has conducted many conferences and promotional programmes to create awareness in public, but the need to educate patients attending hospitals even in Delhi is needed.15,16
Most responders believed that Ayurveda would be effective in chronic conditions17 and can be taken concomitantly with modern medicines. Ayurvedic medicines being safe or with no side-effects and rendering relief to different symptoms were the reasons cited by participants for using Ayurvedic medicines along with modern medicine.18
A low proportion of participants using Ayurvedic medicines currently reflects the imprecise knowledge of specific therapies of Ayurveda such as Panchakarma (other than herbal drugs). In addition, most participants had a history of surgical interventions, which may be associated with their apprehensions about the use of Ayurvedic medicine. Regarding communicating the concomitant use of Ayurvedic medicine to the treating physician, the participants had mixed views. To support this assumption, 40% of participants said that the doctor did not enquire for any concomitant use of Ayurvedic medicines and 16% reported that they did not intend to disclose it. Only 42% of participants believed that their consulting physician at a tertiary care hospital supports the simultaneous use of Ayurvedic medicines. These findings reflect the gap between moderate knowledge, attitude and low practice level.
However, the majority of participants were interested to participate in integrative research studies at AIIMS and avail Ayurveda clinical services. The positive response of patients reflects positive attitude towards Ayurveda as well as trust and faith in AIIMS, Delhi, which has the image of delivering excellence in healthcare and quality research. This emphasizes the need to scale up integrative approaches for authentic and better use of both the systems of medicines.
Among current users of Ayurvedic medicine, the majority cited safety and previous positive experience as the reason for opting for Ayurvedic medicines. The current users reported that they felt improvement in general well-being and that their complaints related to different systems were relieved. This suggests the willingness of the patients to adhere to the Ayurveda system of medicine (Table IV).
| Question | n(%) | |
|---|---|---|
| 1. | Reason for taking Ayurvedic medicines | |
| Ayurveda medicines are safe (no side-effects) | 12 (46.2) | |
| Previous positive experience | 9 (34.6) | |
| Motivated by others | 5 (19.2) | |
| 2. | Benefits of Ayurvedic medicines | |
| Improve strength/immunity/well-being | 11 (34.4) | |
| Relief in different system-wise complaints | 10 (31.2) | |
| No effect yet | 11 (34.4) | |
Our study has several implications for health policy and practice. The findings provide preliminary evidence for the need of awareness regarding Ayurveda and integrative approach in a specific patient group in a tertiary care hospital in Delhi. A major proportion of patients surveyed relied on TV promotional advertisements. Thus, sources of knowledge regarding Ayurveda should be expanded and every effort should be made to prevent the dissemination of misleading information about Ayurvedic drugs and their therapeutic benefits through some advertisements. Infrastructural facilities for integrative management of diseases need to be increased. Educational programmes related to specific disease conditions, judicious use of alternative treatment modalities for better management should be undertaken and integrative studies should be initiated to gather evidence regarding their rationality and benefits. Further studies are needed to investigate in detail the pattern of use of Ayurvedic medicines in specific groups of patients to elicit the underlying factors.
Our study has some limitations. First, the sample is representative of a tertiary care hospital of Delhi; thus, the results may not be generalizable to other hospitals in India and to the Indian population. Since the study is cross-sectional, we do not have information on the actual change in knowledge and attitude of any specific cohort of respondents over time. Third, it cannot be clearly said that the positive response of the participants to the question regarding patients’ interest in integrative research in AIIMS was due to trust in the reputation of the Institute or participants’ belief in the concept of integrated practice.
Conclusion
Our study reveals that the use of Ayurvedic medicines was low among the patients surveyed. Except socioeconomic status, other factors such as age, gender, family type and residential area were not associated with the moderate level of knowledge and attitude observed. Despite imprecise knowledge and limited access to reliable source of information, the responders were willing to participate in integrative research studies and avail Ayurveda OPD and inpatient services if provided at tertiary care level. Initiatives should be taken to enhance the level of knowledge, attitude and fill the gap of practice.
Conflicts of interest
None declared
References
- Prevalence and current therapy in chronic liver disorders. Inflammopharmacology. 2019;27:213-31.
- [CrossRef] [PubMed] [Google Scholar]
- Traditional medicine in China, Korea, and Japan: A brief introduction and comparison. Evid Based Complement Alternat Med. 2012;2012:429103.
- [CrossRef] [PubMed] [Google Scholar]
- Views on traditional Chinese medicine amongst Chinese population: A systematic review of qualitative and quantitative studies. Health Expect. 2014;17:622-36.
- [CrossRef] [PubMed] [Google Scholar]
- The history of medicine in India and Burma. Med Hist. 1968;12:52-61.
- [CrossRef] [PubMed] [Google Scholar]
- Ayurgenomics: A new approach in personalized and preventive medicine. Sci Cult. 2011;77:10-17. Available at www.scienceandculture-isna.org/journal.htm (accessed on 20 Dec 2020)
- [Google Scholar]
- Indian traditional ayurvedic system of medicine and nutritional supplementation. Evid Based Complement Alternat Med. 2013;2013:376327.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in coronary heart disease epidemiology in India. Ann Glob Health. 2016;82:307-15.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary heart disease and risk factors in India: On the brink of an epidemic? Indian Heart J. 2012;64:364-7.
- [CrossRef] [PubMed] [Google Scholar]
- Incubating integrative medicine in India through PMO's Atal incubator scheme of Niti Aayog. Ann Neurosci. 2017;24:131-3.
- [CrossRef] [PubMed] [Google Scholar]
- Health sector reforms for 21(st) century healthcare. J Ayurveda Integr Med. 2015;6:4-9.
- [CrossRef] [PubMed] [Google Scholar]
- Complementary and alternative medicine use in rheumatoid arthritis: An audit of patients visiting a tertiary care centre. Natl Med J India. 2007;20:236-9.
- [Google Scholar]
- Prevalence and determinants of complementary and alternative medicine use among infertile patients in Lebanon: A cross sectional study. BMC Complement Altern Med. 2012;12:129.
- [CrossRef] [PubMed] [Google Scholar]
- Experiences of complementary and alternative medicine in patients with inflammatory bowel disease-A qualitative study. BMC Complement Altern Med. 2014;14:407.
- [CrossRef] [PubMed] [Google Scholar]
- Insights on personalized medicine from Ayurveda. J Altern Complement Med. 2013;19:370-5.
- [CrossRef] [PubMed] [Google Scholar]
- Changing scenario for promotion and development of Ayurveda-way forward. J Ethnopharmacol. 2012;143:424-34.
- [CrossRef] [PubMed] [Google Scholar]
- Government policies and initiatives for development of Ayurveda. J Ethnopharmacol. 2017;197:25-31.
- [CrossRef] [PubMed] [Google Scholar]
- Ayurveda and the battle against chronic disease: An opportunity for Ayurveda to go mainstream? J Ayurveda Integr Med. 2010;1:9-12.
- [CrossRef] [PubMed] [Google Scholar]
- Perception, attitude and usage of complementary and alternative medicine among doctors and patients in a tertiary care hospital in India. Indian J Pharmacol. 2015;47:137-42.
- [CrossRef] [PubMed] [Google Scholar]




