Translate this page into:
Sonographic measurement of cervical length and its relation to the onset of spontaneous labour and the mode of delivery
2 Department of Obstetrics and Gynecology, School of Medical Sciences, Tehran University of Medical Sciences, Tehran, Iran
3 Department of Social Medicine, School of Medical Sciences, Zanjan University of Medical Sciences, Zanjan, Iran
4 Baharloo Hospital, Tehran University of Medical Sciences, Tehran, Iran
5 Department of Reproductive Health and Midwifery, School of Medical Sciences, Faculty of Medical Sciences, Tarbiat Modares University, P.O. Box: 14115-331, Tehran, Iran
Corresponding Author:
Minoor Lamyian
Department of Reproductive Health and Midwifery, School of Medical Sciences, Faculty of Medical Sciences, Tarbiat Modares University, P.O. Box: 14115-331, Tehran
Iran
lamyianm@modares.ac.ir
| How to cite this article: Giyahi H, Marsosi V, Faghihzadeh S, Kalbasi M, Lamyian M. Sonographic measurement of cervical length and its relation to the onset of spontaneous labour and the mode of delivery. Natl Med J India 2018;31:70-72 |
Abstract
Background. We aimed to investigate the relationship between cervical length at 37 weeks of pregnancy and the onset of spontaneous labour as well as mode of delivery.
Methods. We did a prospective observational study of 126 low-risk pregnant women with cephalic presentation who were not in labour, attending a south Tehran health centre for prenatal care. The length of the cervix was measured using transvaginal ultrasound (10 MHz endovaginal transducer) by a single sonographer at 37 weeks of gestation. The outcomes were the onset of spontaneous labour and the mode of delivery.
Results. The mean cervical length was 26.1 mm (range 10-51 mm), with a non-significant difference between nulliparous and parous women (p = 0.36). There was a significant association between cervical length and onset of spontaneous labour (r=0.33, p<0.001 ). When controlled for parity, maternal height and onset of spontaneous labour, cervical length did not predict the mode of delivery (p = 0.79).
Conclusion. Measurement of cervical length at 37 weeks could predict the onset of spontaneous labour, but it failed to predict the mode of delivery.
Introduction
One of the most important issues in prenatal care is to determine the time of delivery. Being aware of delivery time has several potential benefits. Pregnant women could plan their social activities and get prepared for delivery. In addition, clinicians may be able to better manage term pregnancies. The last menstrual period (LMP) and ultrasound scan or a combination of these two methods are usually used to determine the estimated date of confinement (EDC).[1] The LMP method is simple and inexpensive. However, limitations such as recall bias, irregular menstrual cycles, oral contraceptive use and bleeding in early pregnancy, as well as delayed ovulation, could result in inaccurate estimates of EDC.[2] To estimate EDC using ultrasound, foetal measurements are compared with a gestational age-specific reference, so the gestational age estimates for a symmetrically large or small foetus will be inaccurate.[1] Even if the above-mentioned limitations are disregarded, using the LMP method, delivery occurred at the predicted date in only 3.6% of women while using the ultrasound- based method, only 4.3% of women gave birth at the predicted date.[3]
In 1964, the Bishop score was introduced as a method to predict the onset of spontaneous labour in multiparous women.[4] The Bishop score was a subjective method that was vulnerable to inter- and intra-examiner variations, which cause its use to be limited.[5] Then, other more objective and reproducible techniques such as ultrasonographic assessment of cervical length were proposed. To date, numerous studies have evaluated the value of cervical length measurement in predicting pre-term labour and found that using transvaginal ultrasound to measure cervical length is useful in predicting pregnancies that are at risk for pre- term birth.[6]·[7] Also, there has been interest in assessing cervical length to predict the time and mode of the delivery at term.
We measured cervical length using transvaginal ultrasound to predict the onset of spontaneous labour and the mode of delivery in low-risk pregnancies at 37 weeks’ gestation.
Methods
We studied 148 low-risk pregnant women who attended South Tehran health antepartum clinics for prenatal care from August 2011 to June 2012. Written informed consent was obtained from the participants. The inclusion criteria were singleton pregnancies at 37 weeks’ gestation, live foetus with cephalic presentation, no maj or foetal abnormalities, no complications such as pre-eclampsia or foetal growth restriction, no clinical evidence of regular contraction or ruptured membranes and no previous or planned caesarean section. We used two methods, LMP and first trimester ultrasound, to determine the gestational age. When the difference between the gestational ages obtained by these two methods was <7 days, the gestational age was determined on the basis of LMP. Otherwise, it was determined as per the ultrasound. All women underwent a transvaginal ultrasound at the 3 7th week of gestation and were followed up until the onset of spontaneous labour. The outcomes were onset of spontaneous labour and mode of delivery. Spontaneous labour was defined as regular uterine contractions, ruptured membranes or bloody show leading to admission to the delivery unit. Women who had induction of labour or caesarean section before the onset of spontaneous labour were excluded from the study.
To measure cervical length, a 10 MHz transvaginal transducer (GE logic 500, USA) was used by a single specialist sonography physician. The women were asked to empty their bladder before an examination and to lie down in the dorsal lithotomy position. The ultrasound probe was placed in the anterior fornix of the vagina and was withdrawn until an appropriate sagittal view of the cervix was obtained. In the absence of uterine contractions, cervical length was measured from the internal os to the external os along the cervical canal. All measurements were repeated three times and the shortest length was recorded.
The normality of variables was confirmed by the Kolmogorov- Smirnov test. The /-test was used to compare the means of the two groups (parous and nulliparous). The Pearson correlation coefficient was used to quantify the association between cervical length with maternal age, maternal height, body mass index and birth weight. To determine whether or not cervical length could predict the onset of spontaneous labour, linear regression was used. For predicting the mode of delivery, we used multivariate logistic regression to create a model including variables such as cervical length, parity, maternal height and onset time of spontaneous labour. All reported p values were two-sided, and p<0.05 was considered statistically significant. SPSS software version 16 (SPSS, Chicago, IL, USA) was used for statistical analysis.
Our prospective observational study was approved by the Institutional Review Board and the Ethics Committee of Tarbiat Modares University.
Results
Of the 148 women recruited, 4 had breech presentation diagnosed at the time of transvaginal ultrasound and 18 had induction of labour or caesarean section before spontaneous onset of labour. These pregnancies were excluded from analysis. Thus, 126 women were included in the analysis. Sixty-five of them (51.5%) were nulliparous and 61 (48.5%) were parous. The mean (SD) maternal age was 26.5 (5.16) years. The cervical length was normally distributed with a mean (SD) of 26.10 (8.9) mm. About 67.5% of the women had a vaginal delivery, while the rest had a caesarean section after the onset of spontaneous labour.
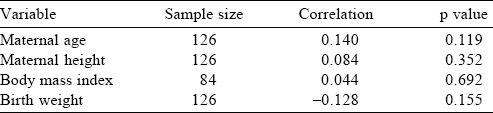
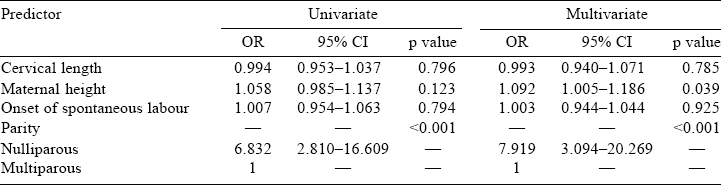
The mean cervical lengths were not significantly different between nulliparous and parous women (25.4 v. 26.9 mm, respectively, p=0.36). There was no significant association between cervical length at 37 weeks and maternal age, maternal height, body mass index and birth weight [Table - 1]. Cervical length was not able to predict the mode of delivery, while the parity, maternal height and the onset time of spontaneous labour were controlled [Table - 2]. In linear regression analysis, the linear relationship between cervical length by ultrasound and onset of spontaneous labour was statistically significant (r=0.333, p<0.001, [Figure - 1].
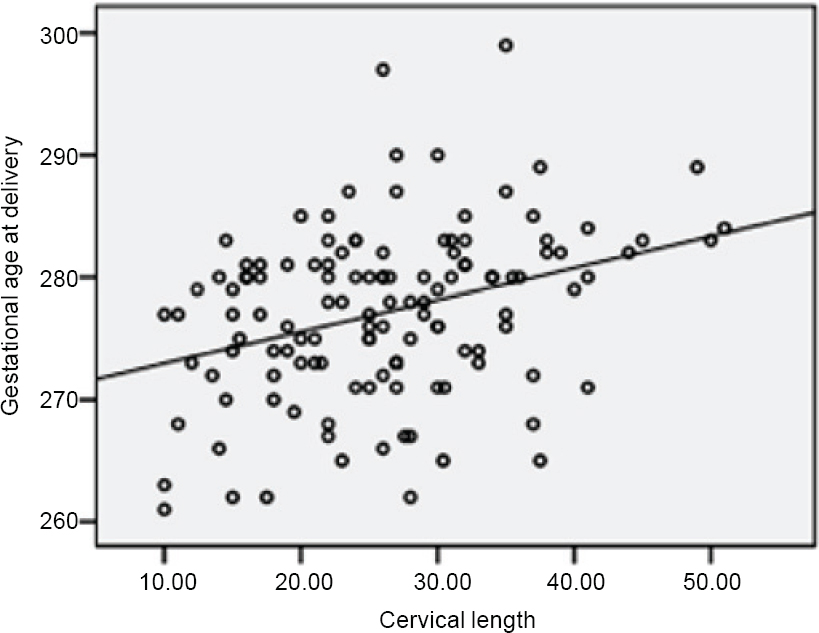 |
| Figure 1: Association between gestational age at delivery and cervical length measured by ultrasound at 37 weeks of gestational age at delivery (days)=270/4+(cervical length [mm]× 0/333); R2=0/11 |
Onset of spontaneous labour occurred in 120 cases (95.2%) at/or before the 41st week of gestation. In the remaining 6 cases (4.8%), it occurred after the 41st week. In these cases, the cervical length at the 37th week was significantly longer than in the former (34.08 [8.5] mm v. 25.70 [8.7] mm, p=0.024). The onset of spontaneous labour after the 41st week increased from 0% to 5.6%, 6.7% and 12.5% for cervical lengths at the 37th week of 10-20, 21-30, 31-40 and 41-50 mm, respectively.
Discussion
Our study revealed that cervical length measured at the 3 7th week of gestation could predict the onset of spontaneous labour but not the mode of delivery in low-risk singleton pregnancies.
Most similar previous studies on cervical length and onset of spontaneous labour had results similar to our study. Rozenberg et al.[8] evaluated 128 singleton vertex pregnancies between 39 weeks and 4 days’ gestation and 40 weeks and 3 days’ gestation. They compared the Bishop score, foetal fibronectin assays and ultrasound measurement of cervical length to ascertain the best marker for onset of spontaneous labour at term and the risk of caesarean section. The Bishop score and ultrasound measurement of cervical length were useful for predicting the onset of spontaneous labour within 7 days, whereas foetal fibronectin was useful to assess the need for caesarean section. Ramanathan et al.[9] measured cervical length by transvaginal sonography at 37 weeks of gestation in 1571 singleton low-risk pregnancies. Their findings showed a significant association between cervical length and gestational age at delivery (r=0.73, p<0.001). Souka et al.[10] examined 647 women with a singleton pregnancy between 24 and 40 weeks of gestation. They found that women with a short cervix had a higher chance for spontaneous delivery after adjustment for gestational age (hazard ratio 1.8). They opined that cervical measurements in the third trimester can be used to calculate the probability of delivery at any gestational age.
Giyahi et al.[11] showed that cervical length at the 3 7th week was significantly more in women who delivered after the 41st week than in those who delivered in or before the 41st week (34.1 mm v. 25.7 mm, respectively, p=0.024). Bayramoglu et al.[12] measured cervical length by transvaginal ultrasonography in 93 pregnant women at 37 completed weeks of gestation and weekly thereafter to predict spontaneous labour in a 7-day period at term. They reported that cervical length predicted spontaneous onset of labour within 7 days. The optimal cut-off values for predicting the onset of spontaneous labour within 7 days were 29.5 mm for cervical length at 37 weeks, 27.5 mm at 38 weeks, 25.5 mm at 39 weeks and 24.5 mm at 40 weeks of gestation.
However, Grotegut et al.[13] found that cervical length did not correlate with onset of spontaneous labour. They had delivery data for 119 women but only 78% ofthese women went into spontaneous labour. Their study had some drawbacks. They included data of only those women who had gone into labour spontaneously and that was a smaller number and the cervical length measurements were done by more than one sonographer. Hence, there is likely to be inter-examiner variability. These could be the possible reasons for the difference in their findings from those of the others.[8],[9],[10],[11],[12]
The strengths of our study are that we measured the cervical length in the 37th week of gestation and not in a range of several weeks. Also the same machine and sonographer measured cervical length, eliminating inter-examiner variability. We also controlled for parity, maternal age and height, body mass index and birth weight.
We found that cervical length could not predict the mode of delivery. Giyahi et al. on nulliparous women (unpublished data, 2012) and Kim et al.[14] and Rozenberg et al.[8] also showed similar results. However, some other studies did find that cervical length predicted the likelihood of caesarean section.[131516] For efficient labour and normal parturition, cervical and myometrial ripening should take place before the onset of spontaneous labour. Those are two independent physiological processes.[1718] Usually, cervical ripening occurs prior to myometrial ripeness. If either process does not happen properly, labour cannot progress well and may lead to caesarean section. The length of the cervix is an indicator of ripeness of the myometrium and not cervical ripening.[1718] Hence, we did not find a relationship between cervical length and mode of delivery. If we had included a factor indicative of cervical ripening, it may have helped predict the mode of delivery.
Conclusion
Transvaginal measurement of cervical length at 37 weeks of gestation can predict the onset of spontaneous labour. This may help identify pregnant women at risk of a protracted pregnancy. It also assists in better management of women who are required to terminate the pregnancy in the near future. If the cervical length was short, the onset of labour is highly likely in the coming week. Hence, the clinician could wait for the woman to go into spontaneous labour. However, if the cervical length was long, induction of labour may be the better course of action.
Acknowledgements
We gratefully acknowledge the Institutional Review Board of Tarbiat Modares University for their approval of the current research. We also acknowledge Tarbiat Modares University Tehran, Iran for financial support for our study.
Conflicts of interest. None declared
| 1. | Lynch CD, Zhang J. The research implications of the selection of a gestational age estimation method. PaediatrPerinatEpidemiol 2007;21 Suppl 2:86-96. [Google Scholar] |
| 2. | Nakling J, Buhaug H, Backe B. The biologic error in gestational length related to the use of the first day of last menstrual period as a proxy for the start of pregnancy. Early Hum Dev 2005;81:833-9. [Google Scholar] |
| 3. | Mongelli M, Wilcox M, Gardosi J. Estimating the date of confinement: Ultrasonographic biometry versus certain menstrual dates. Am J Obstet Gynecol 1996; 174:278-81. [Google Scholar] |
| 4. | Bishop EH. Pelvic scoring for elective induction. Obstet Gynecol 1964;24:266-8. [Google Scholar] |
| 5. | Dhall K, Mittal SC, Kumar A. Evaluation of preinduction scoring systems. Aust N Z J Obstet Gynaecol 1987;27:309-11. [Google Scholar] |
| 6. | Larma JD, Iams JD. Is sonographic assessment of the cervix necessary and helpful? Clin Obstet Gynecol 2012; 55:324-35. [Google Scholar] |
| 7. | Arisoy R, Yayla M. Transvaginal sonographic evaluation of the cervix in asymptomatic singleton pregnancy and management options in short cervix. J Pregnancy 2012;2012: 201628. [Google Scholar] |
| 8. | Rozenberg P, Goffinet F, Hessabi M. Comparison of the Bishop score, ultrasonographically measured cervical length, and fetal fibronectin assay in predicting time until delivery and type of delivery at term. Am J Obstet Gynecol 2000;182: 108-13. [Google Scholar] |
| 9. | Ramanathan G, Yu C, Osei E, Nicolaides KH. Ultrasound examination at 37 weeks’ gestation in the prediction of pregnancy outcome: The value of cervical assessment. Ultrasound Obstet Gynecol 2003;22:598-603. [Google Scholar] |
| 10. | Souka AP, Papastefanou I, Papadopoulos G, Chrelias C, Kassanos D. Cervical length in late second and third trimesters: A mixture model for predicting delivery. Ultrasound Obstet Gynecol 2015;45:308-12. [Google Scholar] |
| 11. | Giyahi H, Lamyian M, Marsosi V, Faghihzadeh S, Kalbasi M. The prediction of prolonged pregnancy by transvaginal ultrasonographic measurement. Zanjan Univ Med Sci J 2013;21:64-73. [Google Scholar] |
| 12. | Bayramoglu O, Arslan M, Yazici FG, Erdem A, Erdem M, Bayramoglu K, et al. Prediction of spontaneous onset of labor at term: The role of cervical length measurement and funneling of internal cervical os detected by transvaginal ultrasonography. Am J Perinatol 2005;22:35-9. [Google Scholar] |
| 13. | Grotegut CA, Dulitzki M, Gaughan JP, Achiron R, Schiff E, Geifman-Holtzman O. Transvaginal ultrasound of cervical length and its correlation to digital cervical examination, time to spontaneous labor and mode of delivery. Arch Gynecol Obstet 2011;284:855-9. [Google Scholar] |
| 14. | Kim SN, Park KH, Jung HJ, Hong JS, Shin DM, Kang WS. Clinical and sonographic parameters at 37 weeks’ gestation for predicting the risk of primary Cesarean delivery in nulliparous women. Ultrasound Obstet Gynecol 2010;36:486-92. [Google Scholar] |
| 15. | Liu X, Yang J, Bian X. Transvaginal ultrasound assessment of cervical changes before onset of labor. Zhonghua Fu Chan Ke Za Zhi 1998;33:588-90. [Google Scholar] |
| 16. | Rao A, Celik E, Poggi S, Poon L, Nicolaides KH; Fetal Medicine Foundation Prolonged Pregnancy Group. Cervical length and maternal factors in expectantly managed prolonged pregnancy: Prediction of onset of labor and mode of delivery. Ultrasound Obstet Gynecol 2008;32:646-51. [Google Scholar] |
| 17. | Granström L, Ekman G, Ulmsten U. Myometrial activity after local application of prostaglandin E2 for cervical ripening and term labor induction. Am J Obstet Gynecol 1990;162:691-4. [Google Scholar] |
| 18. | Garfield RE, Saade G, Buhimschi C, Buhimschi I, Shi L, Shi SQ, et al. Control and assessment of the uterus and cervix during pregnancy and labour. Hum Reprod Update 1998;4:673-95. [Google Scholar] |
Fulltext Views
2,592
PDF downloads
597




