Translate this page into:
Health systems challenges and opportunities in tackling non-communicable diseases in rural areas of India
Corresponding Author:
Anita Nath
National Centre for Disease Informatics and Research (Indian Council of Medical Research), Nirmal Bhawan, ICMR Complex, Poojanhalli Road, off NH-7, adjacent to Trumpet Flyover of BIAL, Kannamangala Post, Bengaluru 562110, Karnataka
India
anitanath@ncdirindia.org
| How to cite this article: Nath A, Shalini MA, Mathur P. Health systems challenges and opportunities in tackling non-communicable diseases in rural areas of India. Natl Med J India 2021;34:29-35 |
Abstract
The increasing burden of non-communicable diseases in rural areas poses new challenges to an already overburdened health systems. We detail these challenges and identify opportunities to address them. The major challenges in service delivery in rural areas include poor accessibility, shortage of adequate manpower especially specialists in rural areas, irregular supply of medicines and lack of adequate diagnostic facilities. This has led to an increased dependency on the private sector resulting in high out-of-pocket and catastrophic health expenditure. The challenges are amplified by lower health literacy, large pool of informal or untrained healthcare practitioners, and lack of proper referral and follow up. The health system opportunities identified include task-shifting by training of mid-level healthcare providers and practitioners from Indian systems of medicine, widening use of e-health and m-health, community engagement and public–private partnerships. Participatory health governance through community engagement has been shown to improve accountability and quality in health systems. Civil society organizations (CSO) can also improve awareness and health-seeking behaviour. New and evidence-based strategies need to be implemented to address health system challenges for tackling non-communicable diseases in rural areas.Introduction
An alarmingly high proportion of the Indian population is affected by non-communicable diseases (NCDs), which accounted for 61.8% of all deaths in 2016 compared to 37.9% in 1990.[1] Almost a third (28.1%) of NCD deaths are caused by cardiovascular diseases. The distribution of NCDs is no longer skewed towards urban and higher socioeconomic subgroups; studies have shown that the burden of NCDs in rural areas in India is increasing. Rural areas are challenged with the ‘triple burden’ of low awareness coupled with myths and misconceptions about NCDs, a poorly functioning public healthcare system, and rising health costs as a result of increasing reliance on the private health sector. In this article, we identify the challenges in tackling NCDs and explore opportunities for health systems in rural areas of India.
NCD Burden in Rural Areas
Emerging evidence suggests that an epidemiological transition is under way in rural areas of India and the proportion of disease burden caused by NCDs is steadily increasing. The INDIAB study showed that the prevalence of biochemical abnormalities associated with NCDs was similar in rural and urban areas for some of the states surveyed.[2] Over 50% of a rural farming population in Tamil Nadu was found to have diabetes or prediabetes based on the estimates for HbA1c.[3] The rising burden of NCDs in rural population could be attributed to the presence of behavioural and lifestyle risk factors, poor awareness about NCDs and its risk factors, poor treatment-seeking behaviour and accessibility to quality healthcare. The prevalence of risk factors for cancer is reportedly higher in rural than urban areas, as seen in National Family Health Survey (NFHS)-4 wherein the proportion of men and women using tobacco was higher in rural than in urban areas in both genders (men: rural v. urban––48% and 39%, women: rural v. urban––8.1% and 4.4%).[4] Low knowledge and awareness levels are evident from the report of the Indian Council of Medical Research India Diabetes Study (phase I) wherein overall urban residents had higher awareness rates (58.4%) compared to rural residents (36.8%) about diabetes.[5]
The report of the expert committee on tribal health published in 2018 stated that the increasing burden of NCDs among tribal populations indicates an early epidemiological transition and needs action. The District Level Household Survey (DLHS)-4 data showed that the prevalence of cardiovascular disease among tribal population was almost equal to that among non-tribals in 10 states.[6] A report from the community-based programme, known as Jan Swasthya Sahyog in rural central India, revealed that the median age of onset for diabetes was much lower among tribals than for other social groups. In addition, the median body mass index (BMI) of tribal people with diabetes was 16.3 kg/m2, which is much lower compared to the median BMI of 23.1 kg/m2 among people with diabetes belonging to the general category and the median BMI of 20 kg/ m2 among people with diabetes belonging to the Scheduled Caste (SC) and other backward class (OBC) groups and 70.7% of tribal people with diabetes had a BMI <18.5 kg/m2.[7] This suggests that there are knowledge gaps regarding the epidemiology of NCDs among tribal populations. The level of awareness and knowledge regarding NCDs is low in tribal areas. The National Nutrition Monitoring Bureau (NNMB) Tribal study 2008–09 found that 1 of 4 tribal adults who suffered from hypertension were not aware of the signs and symptoms. Awareness regarding hypertension was very low (8.4%) among the adult tribal population.[8]
Healthcare Delivery in Rural Areas
India has a three-tier system of healthcare delivery in rural areas, consisting of a subcentre at the periphery, primary health centre (PHC) and community health centre (CHC) which cater to a determined population size. While the Government of India started ‘The National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular diseases and Stroke’ (NPCDCS) in 2010, its implementation is facing many hurdles.[9],[10] The pattern of healthcare delivery under NPCDCS is shown in [Figure - 1].
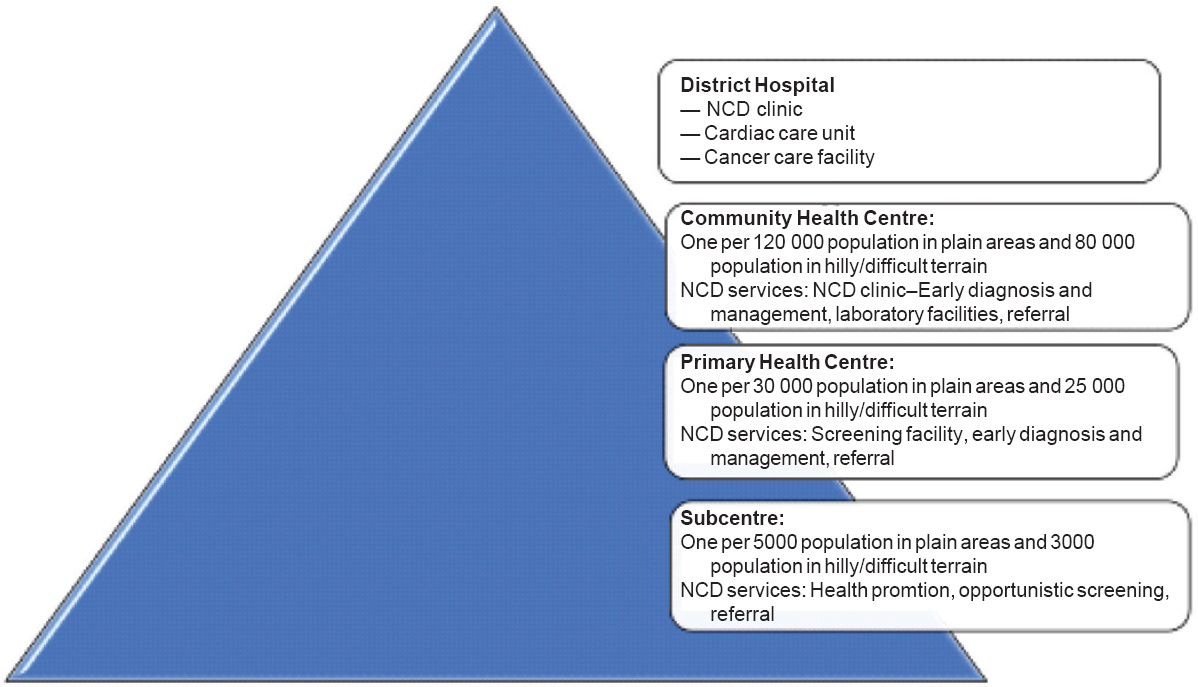 |
| Figure 1: Delivery of care for non-communicable diseases (NCDs) in rural areas |
Health System Challenges in Management of NCDs in Rural Areas
A health system consists of all the organizations, institutions, resources and people whose primary purpose is to improve health.[11] The WHO framework describes health systems in terms of six core components or ‘building blocks’: (i) service delivery, (ii) health workforce, (iii) health information systems, (iv) access to essential medicines, (v) financing and (vi) leader-ship/governance.[12] These components influence healthcare equity and efficiency and have been used here to identify challenges faced by health systems.
Service delivery
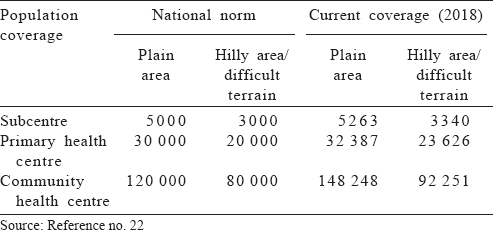
Coverage and accessibility. Over the past few years, there has been an appreciable increase in the number of rural health facilities; however, these do not cater to the prescribed population norms [Table - 1]. Geographical accessibility plays an important role in health-seeking behaviour in rural areas. A study on institutional deliveries in rural areas, which used DLHS data, found that the average distance to the nearest PHC, CHC and district hospital was 9.06, 17.66 and 32.57 km, respectively.[13] In view of poor transport infrastructure and road connectivity, the distance to well-equipped medical facilities is a serious challenge to health systems. This results in resorting to accessing facilities of private healthcare practitioners, most of whom are unregistered.[14],[15]
Quality of care. Population-level studies show that dependency on the private sector for the treatment of NCDs is fairly high in the rural population. Perceptions of better quality of care and medicines and availability of combination medicines are important drivers for the utilization of private healthcare for treating NCDs. A survey done in Tumkur district of Karnataka to assess the utilization of services for treating diabetes and hypertension observed that <10% of household respondents obtained their medicines from a government hospital or PHC.[16] The supply of medicines for treating NCDs is often perceived to be poor and irregular, which results in increased dependency to procure medicines from private chemists. With regard to provider competence, it is seen that PHC doctors are infrequently trained in the management of NCDs; hence, the training component under the NPCDCS needs to be strengthened.[17]
Comprehensiveness. NCDs require a comprehensive approach, including a range of promotive, preventive, curative and rehabilitative service components. Studies have found that the horizontal integration of vertical programmes without improving capacity has overburdened the primary health facilities causing information, education, communication (IEC) activities for prevention of NCDs and screening to take a backseat at the subcentre and PHC levels. Opportunistic screening is prescribed at all levels of health facilities under the NPCDCS. However, screening activities in peripheral health facilities are not up to the prescribed levels. This affects early diagnosis. Even among the treatment services offered for NCDs, there are differences in availability in public healthcare facilities. There is a deficiency of adequate intensive and emergency care facilities in rural areas.[9],[10] Facilities for rehabilitation and home-based palliative care are almost nonexistent in the public health system. Palliative care and end-of-life care are important in NCDs, especially in cancers. Knaul et al. described the lack of palliative care as ‘a medical, public health and moral failing and a travesty of justice’.[18] The Health and Wellness centres launched under the Ayushman Bharat scheme in 2018 have been conceptualized to provide comprehensive primary healthcare and appropriate referral services.[19] However, the implementation will depend on addressing existing health system issues and challenges.
Human resources and infrastructure
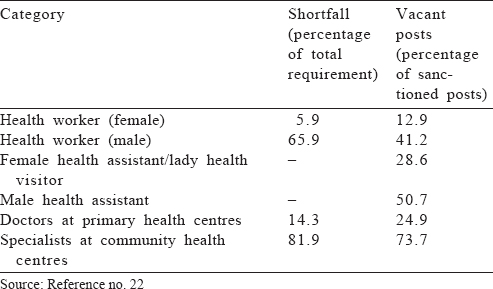
Shortage of health workers. Despite increase in the number of health facilities, a shortfall in availability of workforce remains a key challenge. The proportion of vacant posts against each category of workforce is shown in [Table - 2]. There is reduced retention of specialists and super-specialists at referral units and tertiary care centres, which impairs treatment quality, especially in emergency and intensive care.[20]
There is a need for trained health providers and counsellors at the PHC level for behaviour change communication prescribed for tobacco and alcohol control. With regard to provider competence, PHC doctors are infrequently trained in the management of NCDs, and hence the training component under the NPCDCS needs to be strengthened.[17] The lack of trained and competent staff also affects patient confidence in the healthcare system.
Status of laboratory testing facilities and equipment. Most PHCs do not have adequate basic laboratory equipment and testing facility. Less than a quarter of PHCs (20.72%) were found to be functioning as per the Indian Public Health Standard norms.[21] Other investigations such as echocardiogram, oral glucose tolerance tests and tests to detect complications resulting from diabetes, such as retina evaluation, are scarcely available in public sector facilities. A survey of PHCs in Tumkur district of Karnataka observed that the mean proportion of PHCs having functional laboratory facilities was 84%, and only 40% of the laboratories had testing facilities for NCDs.[16]
Availability of medicines
The WHO Global Action Plan and Monitoring Framework for NCDs proposed that an 80% availability of affordable basic technologies and essential medicines including generics is required to treat major NCDs in all kinds of health facilities.[22] Stockouts of NCD medicines and non-availability of laboratory equipment at PHCs are frequently encountered in rural areas.[16] A study on availability of medicines in public sector facilities of Punjab and Haryana observed that anti-cancer and endocrine medicines were available in <30% of public sector facilities.[23] While none of the studies reported reasons for low availability of essential medicines, the likely reasons include inadequate government funds, issues related to procurement and distribution system and poor prescription practices by health providers.
Governance
NCDs are often not perceived to be a public health priority among state health officials and health personnel in rural areas. More attention is given towards addressing maternal and child health and communicable diseases.
Health financing
The Government of India spends <0.5% of the gross domestic product (GDP) on NCDs and injuries. While the NPCDCS programme has enlisted a series of strategies and action plans, its implementation needs to be supported by a sustainable health financing plan. The control of NCDs is a multisectoral effort that calls for active engagement of all institutions related to healthcare. Of the total public health expenditure on NCDs, 65% is contributed by the Ministry of Health and Family Welfare (MoHFW) and 35% by other central ministries.[24]
Increasing dependency on the private sector for NCD-related treatment results in increased out-of-pocket (OOP) expenditure for medication. It is estimated that NCD-related health expenditure accounts for 48% of the total health expenditure.[25] A secondary analysis of data from the National Sample Survey (NSS) 60th round on ‘Morbidity and Health Care’ on mean OOP on hospitalization due to NCDs showed that the mean annual expenditure was ₹11 327.82 in the public sector and ₹21 917.91 in private facilities.[26] OOP expenditure on private healthcare was higher in urban as well as rural areas. Another study on costing of diabetes care observed that the poorest households in rural areas spent 27% of their income on diabetes care compared to 5% for the richest households.[27]
In spite of availability of several health insurance schemes, the majority of treatment for NCDs is through OOP expenditure. The Government of India has launched Ayushman Bharat Pradhan Mantri Jan Arogya Yojana in 2018, which aims to provide health coverage up to ₹5 lakh per family per year for secondary and tertiary hospitalization to around 50 crore beneficiaries belonging to vulnerable families and provide coverage to the vulnerable and poorest 40% of the population. However, according to the NSS 2017–2018 data, any form of health insurance coverage among the 3rd and 4th wealth quintiles in rural areas were very low at 12.9% and 16%, respectively, compared to 18.2% and 20.4%, respectively in urban areas.[28] This is due to both unaffordability of private insurance and lack of awareness among rural populations. Furthermore, private health insurance comes with caps and sub-limits and considerably higher premiums for older people and people with known risk factors and NCDs. Most insurance schemes do not cover the cost of medicine and investigations incurred in outpatient/clinic consultations. Hence, there is a need to address the problem of high catastrophic expenditure on health, which is pushing middle-income families into a state of poverty and increasing social disparity and inequity.[29]
Health information systems
Monitoring is important for control of NCDs and risk factors. The absence of health records in rural areas affects both individual patient care and overall health monitoring in India. Though vast amounts of data are generated at public health facilities, the flow of information is unidirectional and its quality uncertain. Hence, there is a need for quality assurance procedures for data collected at all levels of health facilities. Electronic Health (eHealth) Records Standards for India were notified by the MoHFW in 2013 and revised in 2016,[30] but adaptation and implementation of these in rural areas still faces several challenges. Monitoring of behavioural and metabolic risk factors necessitates intersectoral approach for data collection. A comprehensive information system that uses multiple sources including health records to monitor risk factors, outcomes and health system responses (including changes in policy) will be important in strengthening health delivery in rural areas.[31]
Health System Opportunities to Address Rising Burden of NCDs in Rural Areas
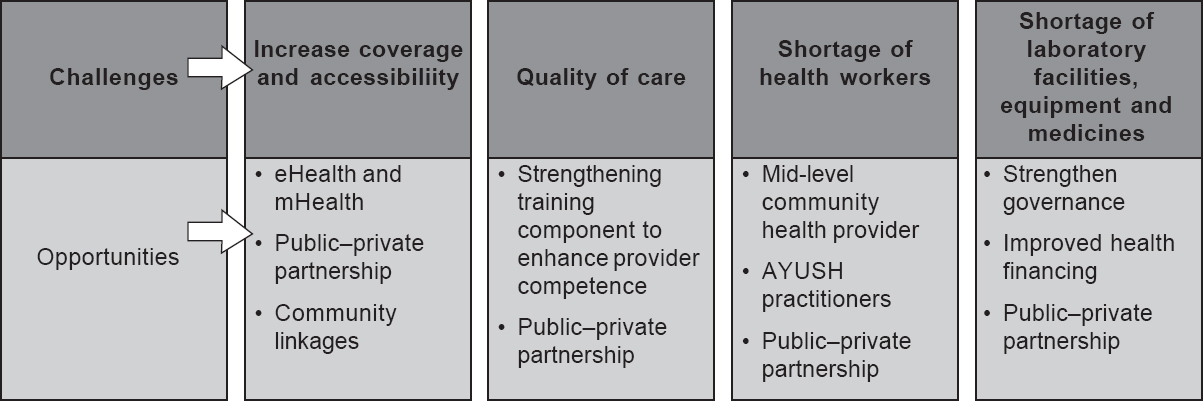
While the existing health systems need to be empowered by addressing the key issues discussed in the preceding section by better governance and health financing schemes, evidence-based measures could be explored and adopted to strengthen health systems for control of NCDs in rural areas. The operationalization of primary healthcare system in a rural area must be characterized by the Starfield ‘4C’ functions: first-contact access, continuity, coordination of care and comprehensiveness.[32] The enlisted challenges and opportunities to overcome these are shown in [Figure - 2].
 |
| Figure 2: Overcoming the challenges by a set of opportunities |
Addressing shortage of workforce
Task shifting is a process of delegation, where some appropriate and carefully selected tasks are moved to less specialized and available health workers. This helps in increasing productivity utilising the existing workforce and expanding the human resource pool affordably and within a shorter timeframe. Task shifting raises concerns about decreased healthcare quality and lack of public trust. However, with an adequate regulatory framework and appropriate training and retraining activities, task shifting can lead to improvement in the quality of healthcare services provided.[33],[34],[35] Existing examples include training ASHA (accredited social health activist) workers to provide screening services, creation of a mid-level cadre of health workers[36] and training AYUSH practitioners to provide basic health services in rural areas. A key factor in the success of these measures was found to be the development and implementation of diagnostic and management algorithms and protocols, to improve capability. Other factors affecting success of task shifting include motivation, patient preference, technical capability and knowledge.[34]
Given the large rural population and shortage of health providers in public health facilities, the government has made an effort to address this shortfall by making provision for a mid-level community health provider in the National Medical Commission Bill 2019. Mid-level providers are health workers who have completed secondary school education and have undergone 2–3 years of healthcare training.[3] After completion of training, they are equipped to perform tasks that are usually carried out by doctors and nurses, such as clinical or diagnostic functions. They will be positioned at the Health and Wellness Centres (HWCs), which are being set-up under the Ayushman Bharat scheme to deliver comprehensive primary health care,[19] as a component of universal health coverage. At present, 25 302 HWCs are functional in India. Although the National Health Policy of 2017 identifies this requirement, an introduction of cadre of such health providers has often been fraught with opposition.
In many countries, mid-level providers are at the forefront of healthcare provision in health facilities. A review of the literature shows that there is no significant difference in the effectiveness of care provided by mid-level health workers and that provided by higher level health workers in high- as well as low-to-middle-income (LMICs) countries.[37] Promoting training courses in rural healthcare to increase the cadre of mid-level providers could be an effective solution to manage workforce shortage. Assam is at present the only state that runs such a course (Diploma in Medicine and Rural Health Course). A few states in southern India and West Bengal run a 4-year university graduate course of Physician Assistant. The graduates are trained in delivering preventive and promotive services in primary care settings. It may be worthwhile for universities/teaching institutions to take up such courses.
The low modern medicine doctor to population ratio in India can be supplemented by creating a well-defined role for AYUSH practitioners in providing NCD care. Training workshops for AYUSH professionals in India on public health approaches towards prevention and control of NCDs are shown to increase capacity for management of NCDs.[38] A pilot project is being implemented in eight districts to explore the knowledge available in the AYUSH system of medicine for prevention and control of NCDs in the form of health promotion, cost-effective AYUSH solutions and yoga intervention.[39],[40] It is hoped that this strategy will yield favourable outcomes.
Widening use of electronic health and mobile health
‘Given the rapid advances in information and mobile phone technology, there is an emerging interest in putting these for use in health systems. Both eHealth and mobile health (mHealth) are becoming important components of healthcare in rural and difficult-to-access areas. eHealth, refers to healthcare services provided with the support of information and communication technology (ICT)—such as computers, mobile phones and satellite communications—for health services and information, while mHealth, refers to the use of smart or portable devices for health services and information’,[41] mHealth can be useful in NCD care from the perspective of clients/patients as well as health providers and programme managers. There are over 1 billion mobile phone users in India, which translates into a population coverage of 86.8%, of which 42% reside in rural areas.[42],[43]
Awareness and treatment adherence: As an example of role of mHealth from a client’s perspective, the MoHFW has partnered with the WHO, and the International Telecommunication Union is initiating the use of mobile technology for tobacco cessation known as the ‘mCessation programme’, which encourages tobacco users to quit the habit by customized guidance in the form of text messages.[44] While 2 million individuals are claimed to have registered for the programme, a beneficial outcome is yet to be ascertained. Likewise, mDiabetes has been initiated with an aim for preventing onset of the disease and its complications. The other areas in which mHealth may be found useful for individual health include ensuring treatment compliance, surveillance of physical activity and dietary intake. Evidence supports the importance of mHealth in addressing NCDs through health education and self-management and improvement in treatment adherence.[45]
Remote monitoring. Use of mHealth innovations to provide monitoring services, including remote electrocardiogram monitoring for cardiac arrhythmias especially in children,[46],[47] remote blood glucose monitoring,[48],[49] and physical activity monitoring and remote guidance for cardiac rehabilitation,[50],[51] are being tried in other parts of the world. These innovations have the potential to make available services that are not otherwise possible in remote and rural areas.
Clinical diagnosis support. From a health provider’s viewpoint, mobile technology can be used in patient management by means of use of diagnostic algorithm, patient monitoring and follow-up.[52] In addition to aiding task shifting, evidence exists that using technology for clinical diagnosis support will improve the quality of health services and patient outcomes.[53] However, further development and evaluation of these applications and their usefulness is necessary.[54]
Big data and machine learning (ML). In relation to using such technology which would be useful for health programmers and policy-makers, mHealth could be integrated with big data, which will make it easier to study, monitor and understand patients’ health status.[55] This is potentially done by extracting health information from multiple sources, analysing by means of big data algorithmic and ML systems and generating robust evidence for improving quality of care.[56]
Telemedicine. This well-known component of eHealth is defined by WHO as, ‘the delivery of health-care services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities’.[57] The MoHFW has partnered with the Department of Information Technology in providing telemedicine services in the country. The National Digital Health Authority of India/National eHealth authority have been tasked with a vision of achieving high-quality health services by employing cost-effective and secure use of ICT in health and health-related fields.[58] Although promoting telemedicine initiatives and widening the use of mobile technology is bound to be fraught with operational and logistic issues, it is certainly promising in improving NCD-related care and improving disease outcomes in the rural population.
Public–private partnership
Public–private partnerships are viewed as an effective strategy to complement the relative strengths of the public and private sectors and overcome each other’s shortcomings. The focus of this partnership is to bring about meaningful contribution from the private sector, charitable and non-governmental organizations in collaboration with the government sector to overcome inequality in the distribution of health services. Such engagements are found to be scalable and sustainable in other LMICs.[59],[60] The Government of India, through NITI Aayog and MoHFW has laid guidelines for strengthening health systems to tackle NCDs by engaging with the private sector.[61] Given the statutory and regulatory frameworks that such support partnerships, it is likely that public–private partnerships will have a meaningful impact on reducing NCD burden.
Community engagement and participation Even though not a component of health systems, civil society forms the core of healthcare delivery. In spite of lack of regulatory or economic authority, civil society influences all areas of health system from policy development to utilisation of services.
Building community linkages for NCD care. At the primary level, NCD health services should have a robust link with the community they serve. This is relevant for activities on prevention of risk factors such as tobacco and alcohol cessation. The MoHFW started Tobacco Cessation Clinics in district hospitals, which target smokers and smokeless tobacco users. A major disadvantage of these clinics is the limited usage by tobacco users from rural areas.[62] Thus, tobacco cessation must be suitably integrated with the primary healthcare system in India, which will result in higher quit rates for tobacco intake.[63] The same applies for alcohol cessation. It is shown that usage of psychosocial or non-pharmacological is affordable and feasible for implementation in primary care facilities.[64]
Civil society organizations. Community engagement through participatory health governance in the National Health Mission has been shown to have a constructive effect on community mobilization and capacity for claiming health rights and has supported the demand for better services.[65],[66],[67] It has had a demonstrable impact on the quality of services, service utilization, coverage and health outcomes. Participatory governance and oversight initiatives have led to heightened awareness of health system functions in the community and improvement in the performance of and support for peripheral health staff.[68]
Conclusion
Among the health system core components or ‘building blocks’, availability of health services is fairly adequate, in view of the intensified efforts of the government. However, the weaker components are inadequate health staff, poor competence, shortage of medicines, inadequate diagnostic services and low health financing. The opportunities lie in identifying innovative and evidence-based strategies to address these challenges. Governance in making NCDs a priority and health spending must be enhanced substantially. There is a need to have an ongoing and sustainable surveillance of the risk factors of NCDs and health system response to identify the gaps in the delivery of quality healthcare in addressing NCDs in rural areas.
Conflicts of interest. None declared
| 1. | Indian Council of Medical Research, Public Health Foundation of India, and Institute of Health Metrics and Evaluation. India-Health of the Nation’s States–The India State Level Disease Burden Initiative. New Delhi, India:ICMR, PHFI and IHME; 2017. [Google Scholar] |
| 2. | Indian Council of Medical Research, Madras Diabetes Research Foundation. ICMR-INdia DIABetes [INDIAB] study (Phase I) Final Report (2008–11). Indian Council of Medical Research, Madras Diabetes Research Foundation; 2016. [Google Scholar] |
| 3. | Swaminathan K, Veerasekar G, Kuppusamy S, Sundaresan M, Velmurugan G, Palaniswami NG. Noncommunicable disease in rural India: Are we seriously underestimating the risk? The Nallampatti noncommunicable disease study. Indian J Endocrinol Metab 2017;21:90–5. [Google Scholar] |
| 4. | International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-4), 2015-16: India. Mumbai:IIPS; 2017. [Google Scholar] |
| 5. | Deepa M, Bhansali A, Anjana RM, Pradeepa R, Joshi SR, Joshi PP, et al. Knowledge and awareness of diabetes in urban and rural India: The Indian Council of Medical Research India Diabetes Study (Phase I): Indian Council of Medical Research India Diabetes 4. Indian J Endocrinol Metab 2014;18:379–85. [Google Scholar] |
| 6. | Ministry of Health and Family Welfare and Ministry of Tribal Affairs. Report of the Expert Committee on Tribal Health, Tribal Health in India: Bridging the Gap and Roadmap for the Future-Policy Brief. Ministry of Health and Family Welfare and Ministry of Tribal Affairs; 2018. [Google Scholar] |
| 7. | Jain Y, Kataria R, Patil S, Kadam S, Kataria A, Jain R, et al. Burden and pattern of illnesses among the tribal communities in central India: A report from a community health programme. Indian J Med Res 2015;141:663–72. [Google Scholar] |
| 8. | National Nutrition Monitoring Bureau. Diet and Nutritional Status of Tribal Population and Prevalence of Hypertension among adults. 2008–09. Technical Report. Hyderabad:National Institute of Nutrition, ICMR; 2009. [Google Scholar] |
| 9. | Ainapure K, Sumit K, Pattanshetty SM. Study on implementation of national programme for prevention and control of cancer, diabetes, cardiovascular diseases and stroke in Udupi district, Karnataka. Int J Community Med Public Health 2018;5:2384–7. [Google Scholar] |
| 10. | Jasani P, Nimavat J, Joshi J, Jadeja Y, Kartha G. Study on evaluation of non-communicable disease control programme in Surendranagar district. Int J Sci Res 2015;4:685–8. [Google Scholar] |
| 11. | World Health Organization. The World Health Report 2000: Health Systems: Improving Performance. Geneva:WHO; 2000. [Google Scholar] |
| 12. | WHO. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. Geneva:WHO; 2010. [Google Scholar] |
| 13. | Kumar S, Dansereau EA, Murray CJ. Does distance matter for institutional delivery in rural India? Appl Econ 2014;46:4091–103. [Google Scholar] |
| 14. | Bhandari L, Dutta S. Health infrastructure in rural India. In: Kalra P, Rastogi A (eds). India Infrastructure Report. 1st ed. New Delhi:Oxford University Press; 2007:265–85. [Google Scholar] |
| 15. | Iyengar S, Dholakia RH. Access of the rural poor to primary healthcare in India. Rev Market Integr 2012;4:71–109. [Google Scholar] |
| 16. | Elias MA, Patil MK, Aivalli P, Srinath B, Munegowda C, Shroff ZC, et al. Preparedness for delivering non-communicable disease services in primary care: Access to medicines for diabetes and hypertension in a district in South India. BMJ Global Health 2018;2:e000519. [Google Scholar] |
| 17. | Bavoria S, Nongkynrih B, Krishnan A. Health workforce availability and competency to manage noncommunicable diseases at secondary care level hospitals of Delhi. Int J Non Commun Dis 2019;4:38–42. [Google Scholar] |
| 18. | Knaul FM, Farmer PE, Krakauer EL, Lima LD, Bhadelia A, Kwete XJ, et al. Alleviating the access abyss in palliative care and pain relief––An imperative of universal health coverage: The Lancet Commission report. Lancet 2018;391:1391–454. [Google Scholar] |
| 19. | Bharat A. Comprehensive Primary Health care through Health and Wellness Centers Operational Guidelines. Ministry of Health and Family Welfare, Government of India; 2018. [Google Scholar] |
| 20. | Bajpai V. The challenges confronting public hospitals in India, their origins, and possible solutions. Adv Public Health 2014;2014:898502. [Google Scholar] |
| 21. | Ministry of Health and Family Welfare. Statistics Division: Rural Health Statistics 2017–18. Government of India, MOHFW; 2019. [Google Scholar] |
| 22. | WHO. Draft Comprehensive Global Monitoring Framework and Targets for the Prevention and Control of Noncommunicable Diseases. Geneva:World Health Organization; 2013:1–9. [Google Scholar] |
| 23. | Prinja S, Bahuguna P, Tripathy JP, Kumar R. Availability of medicines in public sector health facilities of two North Indian States. BMC Pharmacol Toxicol 2015;16:43. [Google Scholar] |
| 24. | Gupta I, Ranjan A. Public expenditure on non-communicable diseases & injuries in India: A budget-based analysis. PLoS One 2019;14:e0222086. [Google Scholar] |
| 25. | Garg CC, Evans DB. What is the Impact of Noncommunicable Diseases on National Health Expenditures: A Synthesis of Available Data. Discussion Paper no 3. Geneva:WHO; 2011. [Google Scholar] |
| 26. | Jeyashree K, Prinja S, Kumar MI, Thakur JS. Inequity in access to inpatient healthcare services for non-communicable diseases in India and the role of out-of-pocket payments. Natl Med J India 2017;30:249–54. [Google Scholar] |
| 27. | Ramachandran A, Ramachandran S, Snehalatha C, Augustine C, Murugesan N, Viswanathan V, et al. Increasing expenditure on health care incurred by diabetic subjects in a developing country: A study from India. Diabetes Care 2007;30: 252–6. [Google Scholar] |
| 28. | National Statistical Office. Key Indicators of Social Consumption in India: Health, NSS 75th round, June 2017–June 2018, Ministry of Statistics and Programme Implementation. Government of India; 2019. [Google Scholar] |
| 29. | Xu K. Household catastrophic health expenditure: A multi-country analysis. Lancet 2003;362:111–17. [Google Scholar] |
| 30. | Ministry of Health and Family Welfare. e-Health Division. Electronic Health Record (EHR) Standards for India. Government of India, MOHFW; 2016. [Google Scholar] |
| 31. | Narain JP, Thankappan KR. Noncommunicable diseases surveillance in India: Moving toward a more comprehensive approach. Int J Non Commun Dis 2018;3:111–14. [Google Scholar] |
| 32. | Starfield B. Is primary care essential? Lancet 1994;344:1129–33. [Google Scholar] |
| 33. | Okyere E, Mwanri L, Ward P. Is task-shifting a solution to the health workers’ shortage in Northern Ghana? PLoS One 2017;12:e0174631. [Google Scholar] |
| 34. | Feiring E, Lie AE. Factors perceived to influence implementation of task shifting in highly specialised healthcare: A theory-based qualitative approach. BMC Health Serv Res 2018;18:899. [Google Scholar] |
| 35. | Seidman G, Atun R. Does task shifting yield cost savings and improve efficiency for health systems? A systematic review of evidence from low-income and middle-income countries. Hum Resour Health 2017;15:29. [Google Scholar] |
| 36. | Global Health Workforce Alliance, World Health Organization. Mid-Level Health Providers a Promising Resource to Achieve the Health Millennium Development Goals. Geneva:World Health Organization; 2010. [Google Scholar] |
| 37. | Lassi ZS, Cometto G, Huicho L, Bhutta ZA. Quality of care provided by mid-level health workers: Systematic review and meta-analysis. Bull World Health Organ 2013;91:824–33I. [Google Scholar] |
| 38. | Kumar D, Raina SK, Bhardwaj AK, Chander V. Capacity building of AYUSH practitioners to study the feasibility of their involvement in non-communicable disease prevention and control. Anc Sci Life 2012;32:116–19. [Google Scholar] |
| 39. | Ministry of Health and Family Welfare. Annual Report 2017-18. New Delhi:Department of Health and Family Welfare, Ministry of Health and Family Welfare, Government of India; 2018:112–13. [Google Scholar] |
| 40. | Saleem MN, Akhtar J, Swasticharan L, Khan MA, Rauf E, et al. Integration of Unani system of medicine in mainstream healthcare for prevention and control of non-communicable diseases. Am J Ethnomed 2018;5:10. [Google Scholar] |
| 41. | Moss RJ, Süle A, Kohl S. eHealth and mHealth. Eur J Hosp Pharm 2019;26: 57–8. [Google Scholar] |
| 42. | Bassi A, John O, Praveen D, Maulik PK, Panda R, Jha V. Current status and future directions of mHealth interventions for health system strengthening in India: Systematic review. JMIR mHealth uHealth 2018;6:e11440. [Google Scholar] |
| 43. | International Telecommunication Union–BDT. Country Profile. India:ITU; 2018. Available at www.itu.int/net4/itud/icteye/CountryProfileReport.aspx?country ID=113 (accessed on 12 Oct 2019). [Google Scholar] |
| 44. | World Health Organization. The Missing O: Scaling up Tobacco Cessation in India Using Mobile Technology. World Health Organization; 2016. Available at http://who.int/tobacco/quitting/scaling-up-cessation-india-using-mobile-technology/en/ (accessed on 5 Oct 2019). [Google Scholar] |
| 45. | Arambepola C, Ricci-Cabello I, Manikavasagam P, Roberts N, French DP, Farmer A. The impact of automated brief messages promoting lifestyle changes delivered via mobile devices to people with type 2 diabetes: A systematic literature review and meta-analysis of controlled trials. J Med Internet Res 2016;18:e86. [Google Scholar] |
| 46. | Kyriacou E, Pattichis C, Pattichis M, Jossif A, Paraskeva L, Konstantinides A, et al. An m-health monitoring system for children with suspected arrhythmias. In: 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2007:1794–7. [Google Scholar] |
| 47. | Bansal A, Kumar S, Bajpai A, Tiwari VN, Nayak M, Venkatesan S, et al. Remote health monitoring system for detecting cardiac disorders. IET Syst Biol 2015;9:309–14. [Google Scholar] |
| 48. | Lanzola G, Losiouk E, Del Favero S, Facchinetti A, Galderisi A, Quaglini S, et al. Remote blood glucose monitoring in mHealth scenarios: A review. Sensors (Basel) 2016;16:1983. [Google Scholar] |
| 49. | Kaiserman K, Buckingham BA, Prakasam G, Gunville F, Slover RH, Wang Y, et al. Acceptability and utility of the my sentry remote glucose monitoring system. J Diabetes Sci Technol 2013;7:356–61. [Google Scholar] |
| 50. | Kitsiou S, Thoma MM, Marai GE, Maglaveras N, Kondos G, Arena R, et al. Development of an innovative mHealth platform for remote physical activity monitoring and health coaching of cardiac rehabilitation patients. doi: 10.1109/BHI.2017.7897223. [Google Scholar] |
| 51. | Geraedts H, Zijlstra A, Bulstra SK, Stevens M, Zijlstra W. Effects of remote feedback in home-based physical activity interventions for older adults: A systematic review. Patient Educ Couns 2013;91:14–24. [Google Scholar] |
| 52. | Meyer AN, Thompson PJ, Khanna A, Desai S, Mathews BK, Yousef E, et al. Evaluating a mobile application for improving clinical laboratory test ordering and diagnosis. J Am Med Inform Assoc 2018;25:841–7. [Google Scholar] |
| 53. | Bakken S, Jia H, Chen ES, Choi J, John RM, Lee NJ, et al. The effect of a mobile health decision support system on diagnosis and management of obesity, tobacco use, and depression in adults and children. J Nurse Pract 2014;10:774–80. [Google Scholar] |
| 54. | Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: A systematic review and meta-analysis. PLoS Med 2013;10:e1001363. [Google Scholar] |
| 55. | Madanian S, Parry DT, Airehrour D, Cherrington M. mHealth and big-data integration: Promises for healthcare system in India. BMJ Health Care Inform 2019;26:e100071. [Google Scholar] |
| 56. | Kayyali B, Knott D, Van Kuiken S. The Big-Data Revolution in US Health Care: Accelerating Value and Innovation. New York:Mc Kinsey & Company; 2013. [Google Scholar] |
| 57. | Telemedicine-Opportunities and Developments in Member States. 2nd ed. Geneva, Switzerland:WHO Press; 2010. [Google Scholar] |
| 58. | NeHA. National eHealth Authority (NeHA). National Health Portal of India. Available from: https://www.nhp.gov.in/national_eHealth_authority_neha_mtl. [Google Scholar] |
| 59. | Maza M, Alfaro K, Garai J, Velado MM, Gage JC, Castle PE, et al. Cervical cancer prevention in El Salvador (CAPE)-An HPV testing-based demonstration project: Changing the secondary prevention paradigm in a lower middle-income country. Gynecol Oncol Rep 2017;20:58–61. [Google Scholar] |
| 60. | Shannon GD, Haghparast-Bidgoli H, Chelagat W, Kibachio J, Skordis-Worrall J. Innovating to increase access to diabetes care in Kenya: An evaluation of Novo Nordisk’s base of the pyramid project. Glob Health Action 2019;12:1605704. [Google Scholar] |
| 61. | NITI Aayog. Guidelines for public private partnership for non-communicable diseases. New Delhi:NITI Aayog; 2019. [Google Scholar] |
| 62. | Murthy P, Saddichha S. Tobacco cessation services in India: Recent developments and the need for expansion. Indian J Cancer 2010;47 (Suppl 1):69–74. [Google Scholar] |
| 63. | Lancaster T, Stead L, Silagy C, Sowden A. Effectiveness of interventions to help people stop smoking: Findings from the Cochrane Library. BMJ 2000;321: 355–8. [Google Scholar] |
| 64. | Ballesteros J, Duffy JC, Querejeta I, Ariño J, González-Pinto A. Efficacy of brief interventions for hazardous drinkers in primary care: Systematic review and meta-analyses. Alcohol Clin Exp Res 2004;28:608–18. [Google Scholar] |
| 65. | Adsul N, Kar M. Study of Rogi Kalyan Samitis in strengthening health systems under national rural health mission, district Pune, Maharashtra. Indian J Community Med 2013;38:223–8. [Google Scholar] |
| 66. | Nongdrenkhomba H, Prasad BM, Baishya A, Shome B. Local governance system for management of public health facilities: Functioning of Rogi Kalyan Samiti in North Eastern States of India. South East Asia J Public Health 2014;4:16–22. [Google Scholar] |
| 67. | Ved R, Sheikh K, George AS, VR. Village health sanitation and nutrition committees: Reflections on strengthening community health governance at scale in India. BMJ Global Health 2018;3 (Suppl 3):e000681. [Google Scholar] |
| 68. | Chand V. Reinventing Public Service Delivery in India: Selected Case Studies. India:SAGE Publishing; 2006. [Google Scholar] |
Fulltext Views
11,629
PDF downloads
3,567




